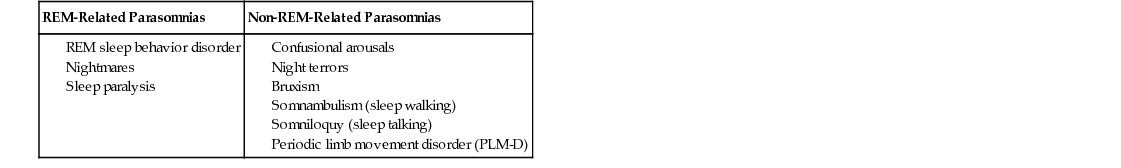
Emily S. Gillett, Raj Dasgupta Excessive daytime sleepiness (or hypersomnolence) in adults is often due to chronic insufficient sleep from self-imposed sleep restriction (due to a “busy lifestyle”). Environmental factors (such as loud noises) or chronic medical conditions (such as joint pain or heartburn) can also cause repeated awakenings overnight and lead to nonrestorative sleep. Insomnia, defined as difficulty falling asleep or difficulty staying asleep, may be a primary problem but is often secondary to chronic medical conditions or psychiatric diagnoses, including anxiety and depression. Excessive alcohol use and abuse of illicit substances or prescription medications, such as narcotics or stimulants, may also lead to irregular sleep patterns and daytime fatigue. It is important to address these sensitive issues in confidential patient interviews and to consider drug testing when appropriate. Chronic snoring may be indicative of obstructive sleep apnea (OSA), particularly in patients who are reported to have multiple short pauses (apneas) in their breathing during sleep. Obstructive apneas are often followed by a loud gasp or snort, which allows the patient to take a deep breath but also arouses him or her from sleep. Although each arousal is short, repeated arousals throughout the night lead to poor quality sleep and a decrease in the percentage of restorative slow-wave (N3) and rapid eye movement (REM) sleep. These arousals are also associated with releases of sympathetic stress hormones that cause repeated, brief increases in pulse rate and blood pressure throughout the night. Over time, untreated OSA may contribute to development of hypertension, arrhythmia, stroke, and other medical conditions. Several physical findings, including elevated body mass index (BMI), large neck circumference, large tonsils, and a small or recessed jaw (micro- or retro-gnathia), make a diagnosis of OSA more likely. One helpful screening tool is the STOP BANG questionnaire. Parasomnias are disruptive behaviors or distressing experiences that occur during sleep or sleep–wake transitions. Sleep deprivation may worsen the severity of any parasomnia. Parasomnias can be divided into those that are REM-related or non-REM-related. In addition to its characteristic rapid eye movements, which can be seen on electrooculogram (EOG) tracings, two important characteristics of normal REM sleep are dreams and atonic paralysis. Nightmares are the most common REM-related parasomnias, consisting of troubling or disturbing dream content that may lead to awakening. Other REM-related parasomnias involve an uncoupling of atonic paralysis from the appropriate stage of sleep. In atonic paralysis, most skeletal muscles (aside from the diaphragm) do not move, and this is important to prevent a person from acting out his or her dreams. In REM sleep behavior disorder, a person does not become atonic and physically acts out aspects of his or her dreams. In sleep paralysis, the opposite occurs and a person’s mind is awake but he or she is atonic and unable to move for a few minutes after awakening. Non-REM parasomnias include night terrors, confusional arousals, teeth grinding (bruxism), sleepwalking (somnambulism), and periodic limb movement disorder (PLM-D), which is often associated with daytime symptoms of restless legs syndrome and difficulty falling asleep. A list of common parasomnias is included in Table 33.1. Drowsy driving is a significant contributing factor in many motor vehicle fatalities. It is important to counsel patients with excessive daytime sleepiness not to drive when they feel drowsy. In the interest of public safety, physicians in some jurisdictions may be required to report to local agencies those individuals with severe, refractory hypersomnia that may render them unfit to operate a motor vehicle. Drowsy driving is also an important issue for overnight shift workers and medical trainees. Surveys of medical residents have suggested that working a shift lasting over 24 hours increases the risk of having a motor vehicle collision by more than twofold. Sleep deprivation can also contribute to medical errors. Most residency programs now teach trainees how to recognize signs of fatigue and encourage them to employ techniques, such as strategic napping, to mitigate fatigue and its potential impacts on education and patient care. The Epworth Sleepiness Scale is a validated questionnaire that measures a patient’s general level of daytime sleepiness. It has been modified for use in pediatric populations and translated into many different languages. Scores ≥9 out of 24 suggest excessive daytime sleepiness and merit evaluation by a sleep specialist.
A 25-Year-Old Female With Excessive Daytime Sleepiness
What are common causes of excessive daytime sleepiness in adults?
Why might a history of snoring be medically important?
What are parasomnias?
Why is it important to ask about driving in patients with excessive daytime sleepiness?
What is the Epworth Sleepiness Scale?
33 A 25-Year-Old Female With Excessive Daytime Sleepiness
Case 33