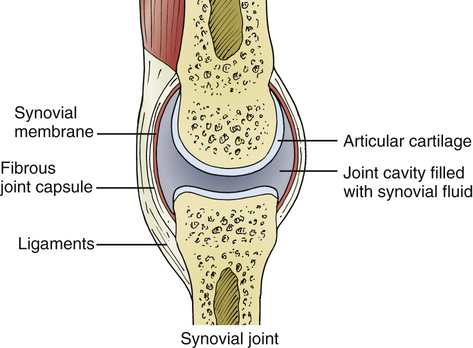
R. Michelle Koolaee The most important question to ask is the duration of symptoms, as the differential diagnosis can be vastly different for acute (<6 weeks) versus chronic (>6 weeks) joint pain. Secondly, questions such as the presence/duration of morning stiffness and presence of joint swelling help to determine whether the joint pain is due to an inflammatory (versus noninflammatory) arthritis. Morning stiffness greater than 1 hour along with joint swelling is more typical of an inflammatory arthritis. Last, the distribution and number of joints involved should always be elicited, as this may also help determine the etiology of joint pain. Monoarticular refers to one joint, oligoarticular refers to fewer than five joints, and polyarticular refers to five or more joints. Common considerations for someone with acute arthritis include infectious etiologies as well as crystalline arthritis (i.e., gout and pseudogout). Causes of acute viral polyarthritis include parvovirus B19, hepatitis B virus (HBV), hepatitis C virus (HCV), and rubella. Other infectious etiologies include septic arthritis (usually monoarticular), Lyme arthritis (a late manifestation of Lyme disease characterized usually by a monoarticular or oligoarticular arthritis), poststreptococcal reactive arthritis (arthritis following throat infection with β-hemolytic group A streptococcus), and reactive arthritis (arthritis in the setting of a recent urethritis or enteric infection). Causes of chronic arthritis are vast but would usually exclude common infectious causes or crystalline arthritis. As broad categories, connective tissue disease and paraneoplastic processes would be higher considerations in someone with chronic symptoms and less likely in someone with acute symptoms. The patient has chronic polyarticular joint pain, which likely represents an inflammatory arthritis. The duration of her symptoms (in conjunction with her other clinical manifestations) make an infectious or crystalline arthritis less likely (furthermore, a crystalline arthritis would not explain her systemic manifestations). She is young and has no constitutional symptoms, so malignancy-associated arthritis is less likely at this point. Her shortness of breath and pleuritic chest pains are suspicious for serositis. Serositis can be a manifestation of many connective tissue diseases, although most commonly associated with systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Thus, overall, the suspicion is highest at this time for a connective tissue disease–associated illness. The term synovial thickening is often used interchangeably with synovitis. The synovial membrane is a structure that resides in between the joint capsule and the joint cavity (see Fig. 16.1) and is responsible for producing synovial fluid. This membrane can become inflamed in any type of inflammatory arthritis, which may include infectious, autoimmune, crystalline, or neoplastic etiologies. Physical findings of synovial thickening are usually characterized by a “boggy” sensation to the joint, which is typically associated with tenderness and swelling. Effusions are also a feature of synovial thickening. TABLE 16.1 Initial Laboratory Tests This is a young female who presents with a chronic polyarticular inflammatory arthritis, serositis (pleural effusions), and fatigue, with laboratory evidence of leukopenia, anemia, and marked thrombocytopenia. Connective tissue disease is highest on the differential at this time, particularly given the chronicity of the inflammatory arthritis in conjunction with evidence of other systemic organ involvement. The combined arthritic, pleuritic, and hematologic manifestations are very characteristic features of SLE, which would carry the strongest likelihood of all the connective tissues illnesses. RA is also a possibility, given the chronic polyarticular inflammatory arthritis and serositis; however, it usually does not present with severe pancytopenia. Patients with Sjögren’s syndrome may present with extraglandular manifestations and occasionally do lack overt symptoms of oral or ocular dryness. However, this would be much lower on the differential. Pancytopenia and serositis are not usual manifestation of the seronegative spondyloarthritis (SpA) and would be very unlikely as well. Systemic vasculitis should always be considered in anyone with multisystem organ involvement; however, this would not be a consideration at this time given the much higher likelihood of SLE.
A 26-Year-Old Female With Joint Pain
What are critical questions to ask in anyone with a history of joint pain?
How does this information help you to form a differential diagnosis?
What is synovial thickening and how do you test for it? What does it mean?
Leukocyte count
3000/µL (3.0 × 109/L)
Hemoglobin
9.8 g/dL (98 g/L)
Platelet count
8000/µL (8 × 109/L)
Leukocyte differential
Normal
Erythrocyte sedimentation rate
86 mm/h
Serum creatinine
0.6 mg/dL
Urinalysis
1+ protein; 0-2 erythrocytes/HPF; 5-10 leukocytes/HPF
Chest radiograph
Blunted costophrenic angles bilaterally without infiltrate
What is your differential diagnosis at this point?
16 A 26-Year-Old Female With Joint Pain
Case 16