Regeneration in the Alveolar Lining
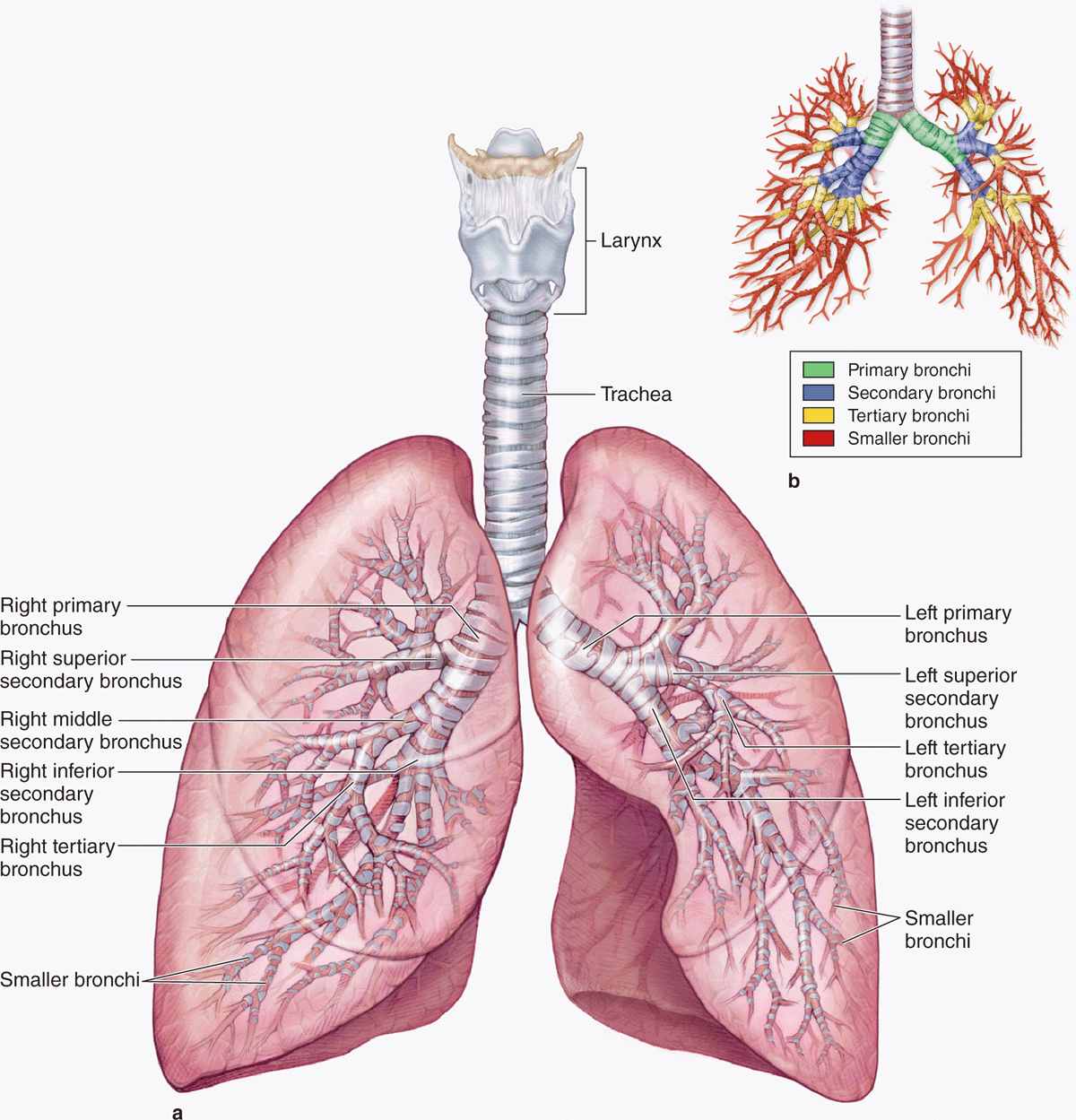
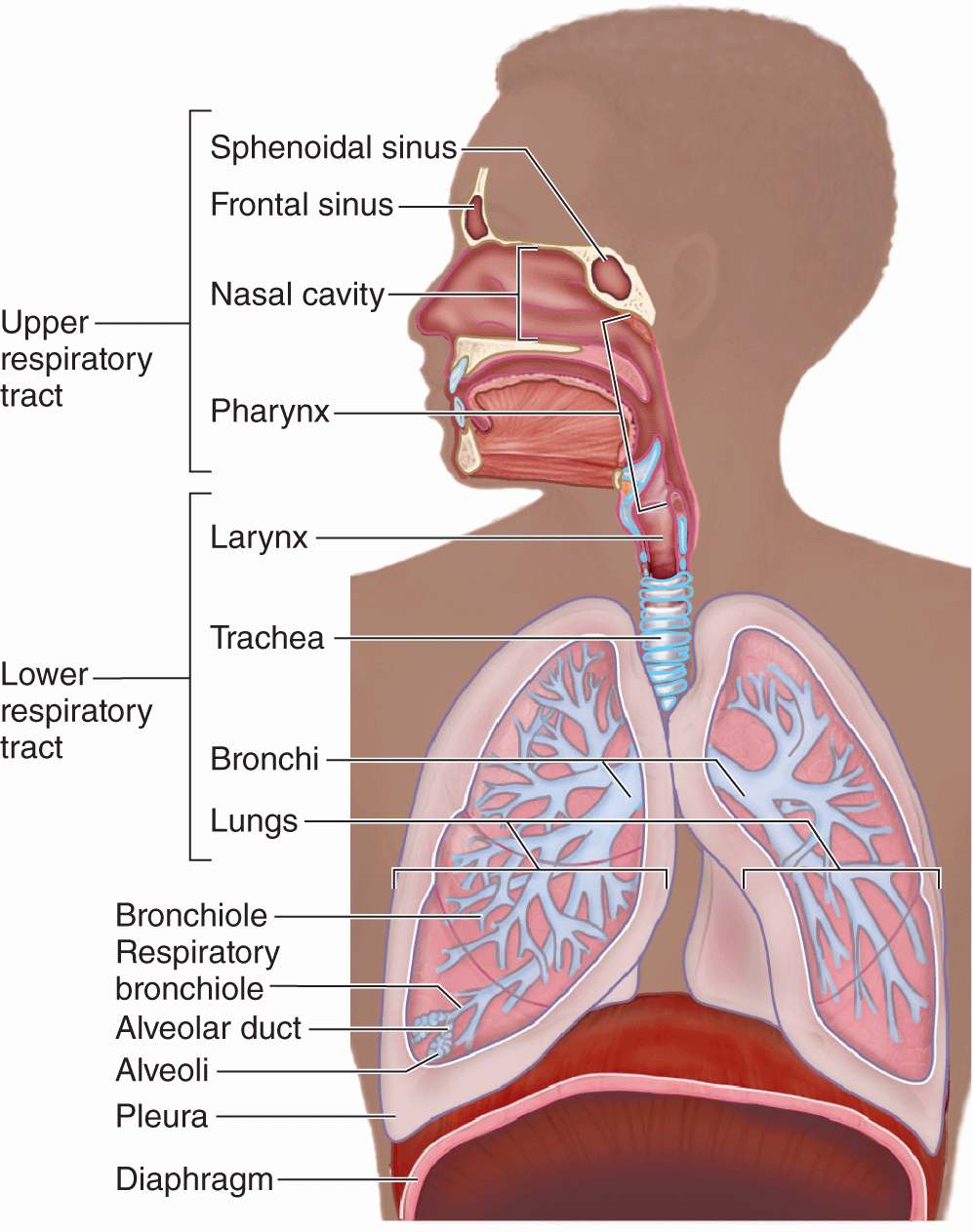
The respiratory system provides for exchange of O2 and CO2 to and from the blood. Respiratory organs include the lungs and a branching system of bronchial tubes that link the sites of gas exchange with the external environment. Air is moved through the lungs by a ventilating mechanism, consisting of the thoracic cage, intercostal muscles, diaphragm, and elastic components of the lung tissue. The system is divided anatomically into structures of the upper and lower respiratory tracts (Figure 17–1). Functionally, the system has two components:
FIGURE 17–1 Anatomy of the respiratory system.
 The conducting portion, which consists of the nasal cavities, nasopharynx, larynx, trachea, bronchi (Gr. bronchos, windpipe), bronchioles, and terminal bronchioles
The conducting portion, which consists of the nasal cavities, nasopharynx, larynx, trachea, bronchi (Gr. bronchos, windpipe), bronchioles, and terminal bronchioles
 The respiratory portion, where the system’s main function of gas exchange occurs, consisting of respiratory bronchioles, alveolar ducts, and alveoli
The respiratory portion, where the system’s main function of gas exchange occurs, consisting of respiratory bronchioles, alveolar ducts, and alveoli
Alveoli, the cellular sites of the exchange of O2 and CO2 between inspired air and blood, are saclike structures that make up most of the lungs.
The conducting portion cleans and humidifies the inspired air and provides a conduit through which air moves to and from the lungs. To ensure an uninterrupted supply of air, a combination of cartilage, elastic and collagen fibers, and smooth muscle provides the conducting portion with rigid structural support and the necessary flexibility and extensibility.
NASAL CAVITIES
The left and right nasal cavity each has two components: the external, dilated vestibule and the internal nasal cavity. Skin of the nose enters the nares (nostrils) partway into the vestibule and has sweat glands, sebaceous glands, and coarse, moist vibrissae (hairs) that filter out particulate material from the inspired air. Within the vestibule, the epithelium loses its keratinized nature and undergoes a transition to typical pseudostratified columnar epithelium before entering the nasal cavities.
The nasal cavities lie within the skull as two cavernous chambers separated by the osseous nasal septum. Extending from each lateral wall are three bony shelflike projections (Figure 17–1) called conchae, or turbinates. The mucosa covering these and other parts of the nasal cavity walls has a lamina propria with important roles in conditioning inhaled air. A complex vasculature with loops of capillaries near the epithelial surface carries blood in a general direction counter to the flow of inspired air and releases heat to warm that air while it is humidified by water released from small seromucous glands. The thin layer of mucus produced by these glands and the goblet cells also serves to trap particulate and gaseous air impurities that are then removed. Immunoglobulin A (IgA) from plasma cells in the lamina propria is also present in nasal secretions.
The middle and inferior conchae are covered with respiratory epithelium; the roof of the nasal cavities and the superior conchae are covered with specialized olfactory epithelium.
Respiratory Epithelium
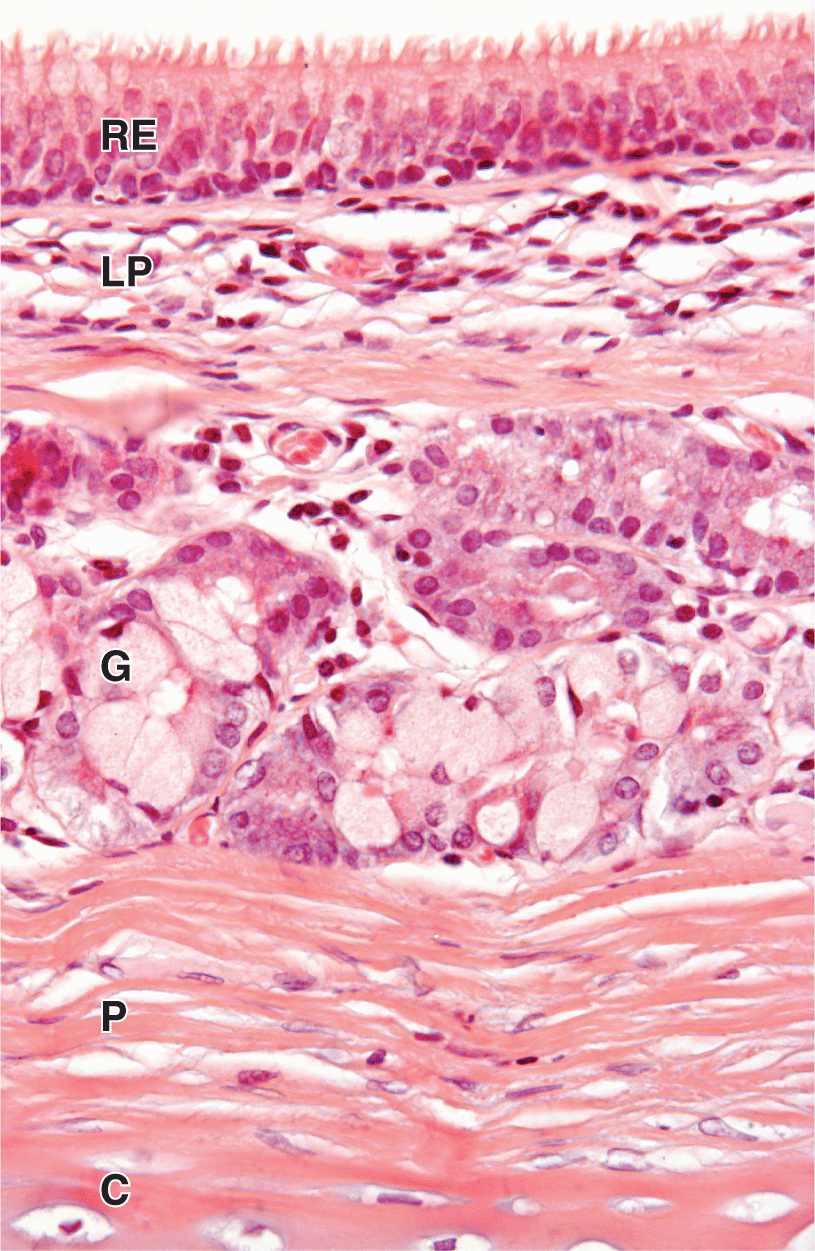
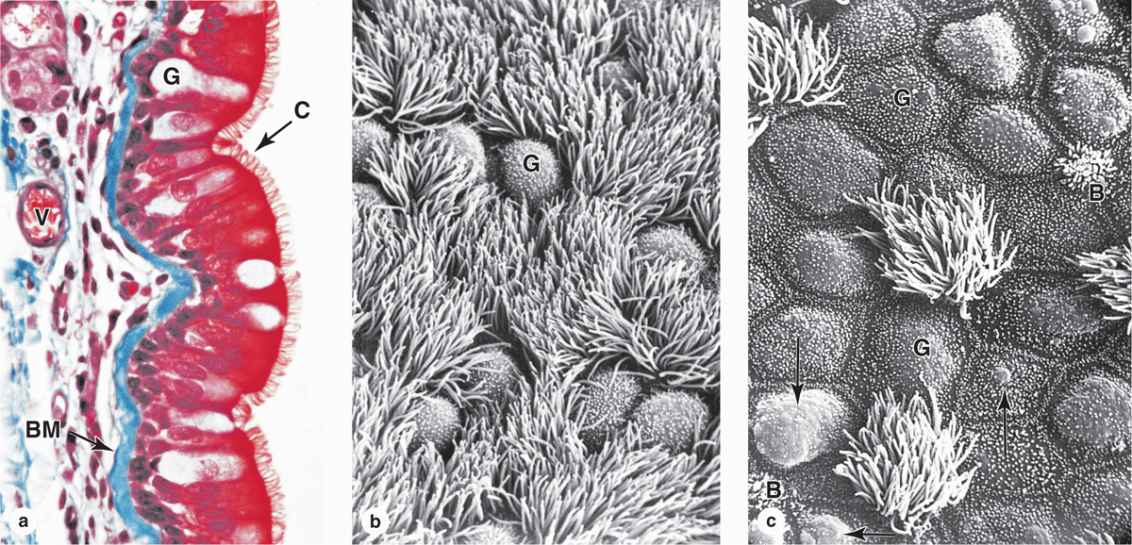
Most of the nasal cavities and the respiratory system’s conducting portion is lined with mucosa having ciliated pseudostratified columnar epithelium, described with epithelia in Chapter 4 and commonly known as respiratory epithelium (Figure 17–2). This epithelium has five major cell types, all of which contact an unusually thick basement membrane:
 Ciliated columnar cells are the most abundant, each with 250-300 cilia on its apical surface (Figure 17–2).
Ciliated columnar cells are the most abundant, each with 250-300 cilia on its apical surface (Figure 17–2).
 Goblet cells are also numerous and predominate in some areas (Figure 17–2), with basal nuclei and apical domains filled with granules of mucin glycoproteins.
Goblet cells are also numerous and predominate in some areas (Figure 17–2), with basal nuclei and apical domains filled with granules of mucin glycoproteins.
 Brush cells are a much less numerous, columnar cell type, in which a small apical surface bears sparse, blunt microvilli (Figure 17-2c). Brush cells are chemosensory receptors resembling gustatory cells, with similar signal transduction components and synaptic contact with afferent nerve endings on their basal surfaces.
Brush cells are a much less numerous, columnar cell type, in which a small apical surface bears sparse, blunt microvilli (Figure 17-2c). Brush cells are chemosensory receptors resembling gustatory cells, with similar signal transduction components and synaptic contact with afferent nerve endings on their basal surfaces.
 Small granule cells (or Kulchitsky cells) are difficult to distinguish in routine preparations, but possess numerous dense core granules 100 to 300 nm in diameter. Like enteroendocrine cells of the gut, they are part of the diffuse neuroendocrine system (DNES; see Chapter 20). Like brush cells, they represent only about 3% of the cells in respiratory epithelium.
Small granule cells (or Kulchitsky cells) are difficult to distinguish in routine preparations, but possess numerous dense core granules 100 to 300 nm in diameter. Like enteroendocrine cells of the gut, they are part of the diffuse neuroendocrine system (DNES; see Chapter 20). Like brush cells, they represent only about 3% of the cells in respiratory epithelium.
 Basal cells are mitotically active stem and progenitor cells that give rise to the other epithelial cell types.
Basal cells are mitotically active stem and progenitor cells that give rise to the other epithelial cell types.
FIGURE 17–2 Respiratory epithelium.
Olfactory Epithelium
The olfactory chemoreceptors for the sense of smell are located in the olfactory epithelium, a specialized region of the mucous membrane covering the superior conchae at the roof of the nasal cavity. In adult humans, it is about 10 cm2 in area and up to 100 Ām in thickness. This thick, pseudostratified columnar epithelium has three major cell types (Figure 17–3):
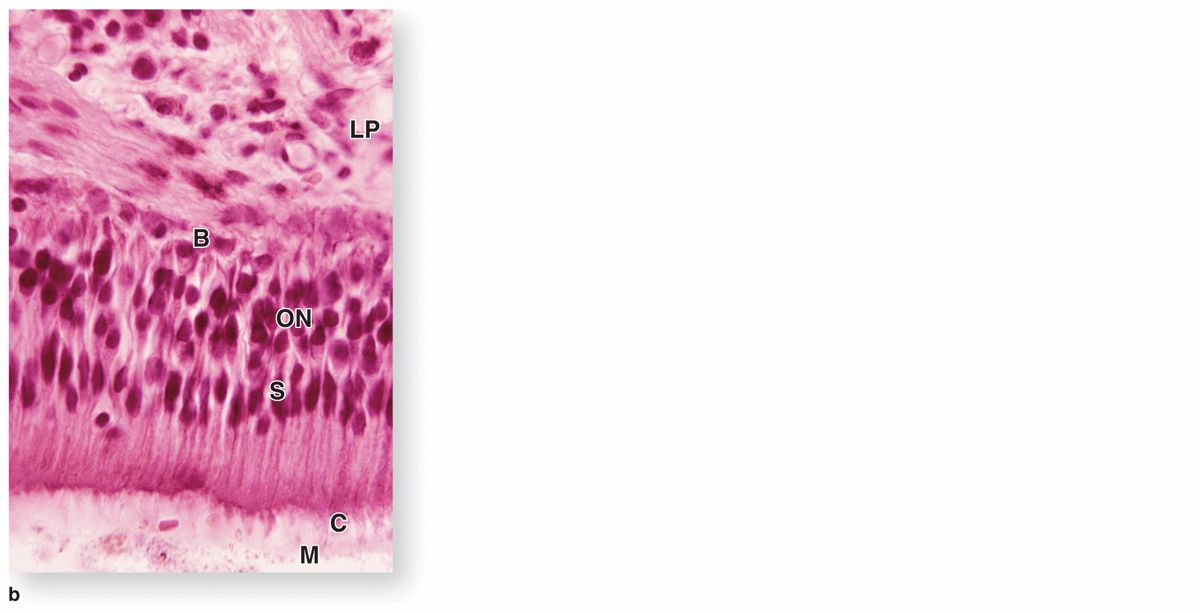
FIGURE 17–3 Olfactory mucosa.
 Olfactory neurons are bipolar neurons present throughout this epithelium. Their nuclei form an irregular row near the middle of this thick epithelium. The apical (luminal) pole of each olfactory cell is its dendrite end and has a knoblike swelling with about a dozen basal bodies. From the basal bodies emerge long cilia with nonmotile axonemes but considerable surface areas for membrane chemoreceptors. These receptors respond to odoriferous substances by generating an action potential along the axons extending from the basal ends of these neurons. The axons leave the epithelium and unite in the lamina propria as very small nerves that then pass to the brain through foramina in the cribriform plate of the ethmoid bone (Figure 17–3). There they form the olfactory nerve, cranial nerve I, and eventually synapse with other neurons in the olfactory bulb.
Olfactory neurons are bipolar neurons present throughout this epithelium. Their nuclei form an irregular row near the middle of this thick epithelium. The apical (luminal) pole of each olfactory cell is its dendrite end and has a knoblike swelling with about a dozen basal bodies. From the basal bodies emerge long cilia with nonmotile axonemes but considerable surface areas for membrane chemoreceptors. These receptors respond to odoriferous substances by generating an action potential along the axons extending from the basal ends of these neurons. The axons leave the epithelium and unite in the lamina propria as very small nerves that then pass to the brain through foramina in the cribriform plate of the ethmoid bone (Figure 17–3). There they form the olfactory nerve, cranial nerve I, and eventually synapse with other neurons in the olfactory bulb.
 Supporting cells are columnar, with broad, cylindrical apexes containing the nuclei and narrower bases. On their free surface are microvilli submerged in a fluid layer. Well-developed junctional complexes bind the supporting cells to the olfactory cells. The supportive role of these cells is not well understood, but they express abundant ion channels that help maintain a microenvironment conducive to olfactory function and survival.
Supporting cells are columnar, with broad, cylindrical apexes containing the nuclei and narrower bases. On their free surface are microvilli submerged in a fluid layer. Well-developed junctional complexes bind the supporting cells to the olfactory cells. The supportive role of these cells is not well understood, but they express abundant ion channels that help maintain a microenvironment conducive to olfactory function and survival.
 Basal cells are small, spherical or cone-shaped cells near the basal lamina. These are the stem cells for the other two types, replacing the olfactory neurons every 2 to 3 months and support cells less frequently.
Basal cells are small, spherical or cone-shaped cells near the basal lamina. These are the stem cells for the other two types, replacing the olfactory neurons every 2 to 3 months and support cells less frequently.
The lamina propria of the olfactory epithelium possesses large serous glands, the olfactory glands (of Bowman), which produce a constant flow of fluid surrounding the olfactory cilia and facilitating the access of new odoriferous substances.
Paranasal Sinuses
The paranasal sinuses are bilateral cavities in the frontal, maxillary, ethmoid, and sphenoid bones of the skull (Figure 17–1). They are lined with a thinner respiratory epithelium with fewer goblet cells. The lamina propria contains only a few small glands and is continuous with the underlying periosteum. The paranasal sinuses communicate with the nasal cavities through small openings; mucus produced there is moved into the nasal passages by the activity of the ciliated epithelial cells.
NASOPHARYNX
The nasal cavities open posteriorly into the nasopharynx, which is the first part of the pharynx and continuous caudally with the oropharynx, the posterior part of the oral cavity leading to the larynx (Figure 17–1). The nasopharynx is lined with respiratory epithelium, and its mucosa contains the medial pharyngeal tonsil and the bilateral openings of the auditory tubes connected to each middle ear cavity.
LARYNX
The larynx is a short (4 cm × 4 cm) passage for air between the pharynx and the trachea (Figure 7–1). Its rigid wall is reinforced by hyaline cartilage (in the thyroid, cricoid, and the inferior arytenoid cartilages) and smaller elastic cartilages (in the epiglottis, cuneiform, corniculate, and the superior arytenoid cartilages), all of which are connected by ligaments. In addition to maintaining an open airway, movements of these cartilages by skeletal muscles participate in sound production during phonation.
The epiglottis, a flattened structure projecting from the upper rim of the larynx, serves to prevent swallowed food or fluid from entering that passage. Its upper, or lingual, surface has stratified squamous epithelium; at variable points on its laryngeal surface this epithelium undergoes a transition to ciliated pseudostratified columnar (respiratory) epithelium. Mixed mucous and serous glands are found in the lamina propria beneath the epithelium.
Below the epiglottis and laryngeal vestibule, the mucosa projects into the lumen bilaterally with two pairs of folds separated by a narrow space or ventricle (Figure 17–4). The upper pair, the immovable vestibular folds, is partly covered with typical respiratory epithelium overlying numerous seromucous glands and occasional lymphoid nodules. The lower pair of folds, the vocal folds (or cords), have features important for phonation or sound production:
FIGURE 17–4 Larynx.
 They are covered with stratified squamous epithelium that protects the mucosa from abrasion and desiccation from rapid air movement.
They are covered with stratified squamous epithelium that protects the mucosa from abrasion and desiccation from rapid air movement.
 A dense regular bundle of elastic connective tissue, the vocal ligament, supports the free edge of each vocal fold.
A dense regular bundle of elastic connective tissue, the vocal ligament, supports the free edge of each vocal fold.
 Deep to the mucosa of each vocal fold are large bundles of striated fibers that comprise the vocalis muscle.
Deep to the mucosa of each vocal fold are large bundles of striated fibers that comprise the vocalis muscle.
During phonation the vocalis muscles draw the paired vocal folds together (adduction), narrowing the intervening luminal space, the rima glottidis, and air expelled from the lungs causes the adducted vocal folds to vibrate and produce sound.
The pitch and other qualities of the sound are altered by changing the tension on the vocal folds, the width of the rima glottidis, the volume of air expelled, etc. The vestibular folds and ventricles, along with other structures and spaces higher in the respiratory tract, contribute to the resonance of sound produced in the larynx. Speech is produced when sounds made in the larynx are modified by movements of the pharynx, tongue, and lips. The larynx is larger in males than in females after puberty, causing men’s voices to be typically deeper than women’s voices.
TRACHEA
The trachea, 10 to 12 cm long in adults, is lined with typical respiratory mucosa in which the lamina propria contains numerous seromucous glands producing watery mucus (Figure 17–5). A series with about a dozen C-shaped rings of hyaline cartilage in the submucosa reinforces the wall and keeps the tracheal lumen open (Figure 17–6). The open ends of the cartilage rings are on the posterior surface, against the esophagus, and are bridged by a bundle of smooth muscle called the trachealis muscle and a sheet of fibroelastic tissue attached to the perichondrium. The entire organ is surrounded by adventitia.
FIGURE 17–5 Trachea.
FIGURE 17–6 Bronchial tree.
The trachealis muscle relaxes during swallowing to facilitate the passage of food by allowing the esophagus to bulge into the lumen of the trachea, with the elastic layer preventing excessive distention of the lumen. The muscle strongly contracts in the cough reflex to narrow the tracheal lumen and provide for increased velocity of the expelled air and better loosening of material in the air passage.
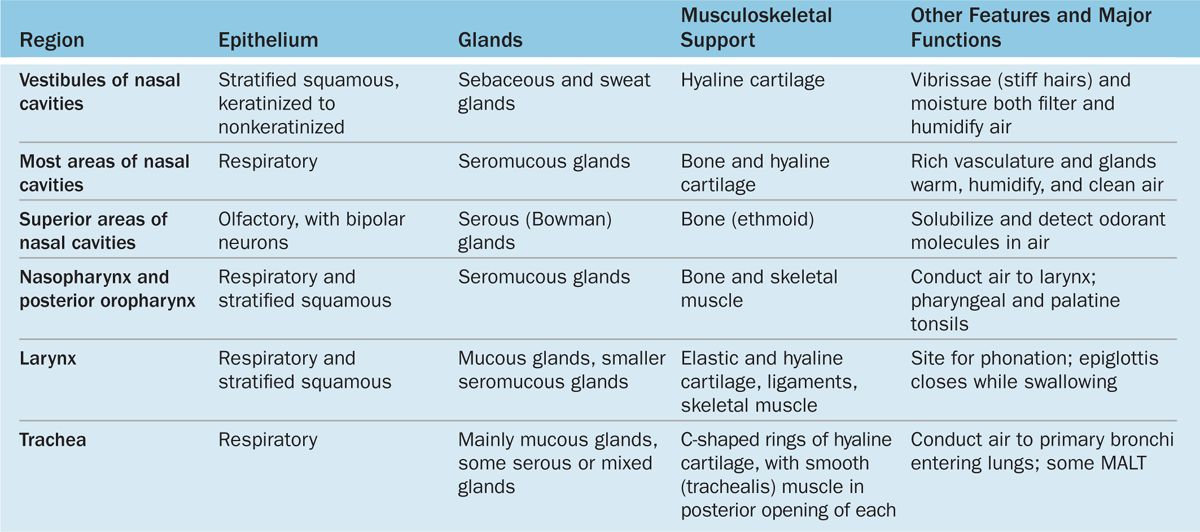
Major features of all upper respiratory tract structures are summarized in Table 17–1.
TABLE 17–1 Histologic features of the upper respiratory tract, larynx, and trachea.
 MEDICAL APPLICATION
MEDICAL APPLICATION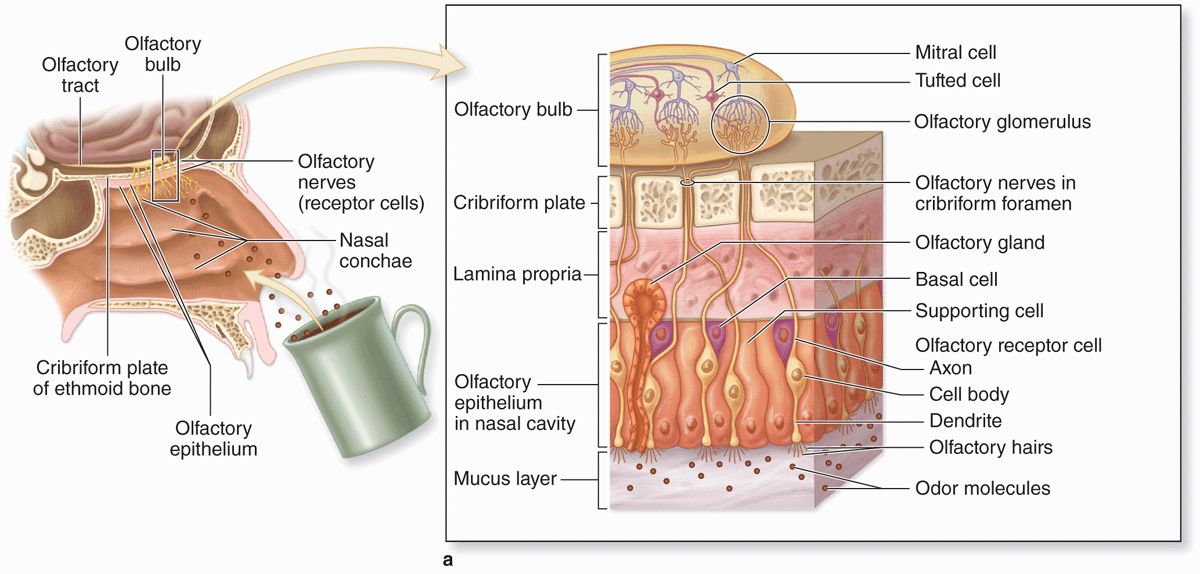
 MEDICAL APPLICATION
MEDICAL APPLICATION MEDICAL APPLICATION
MEDICAL APPLICATION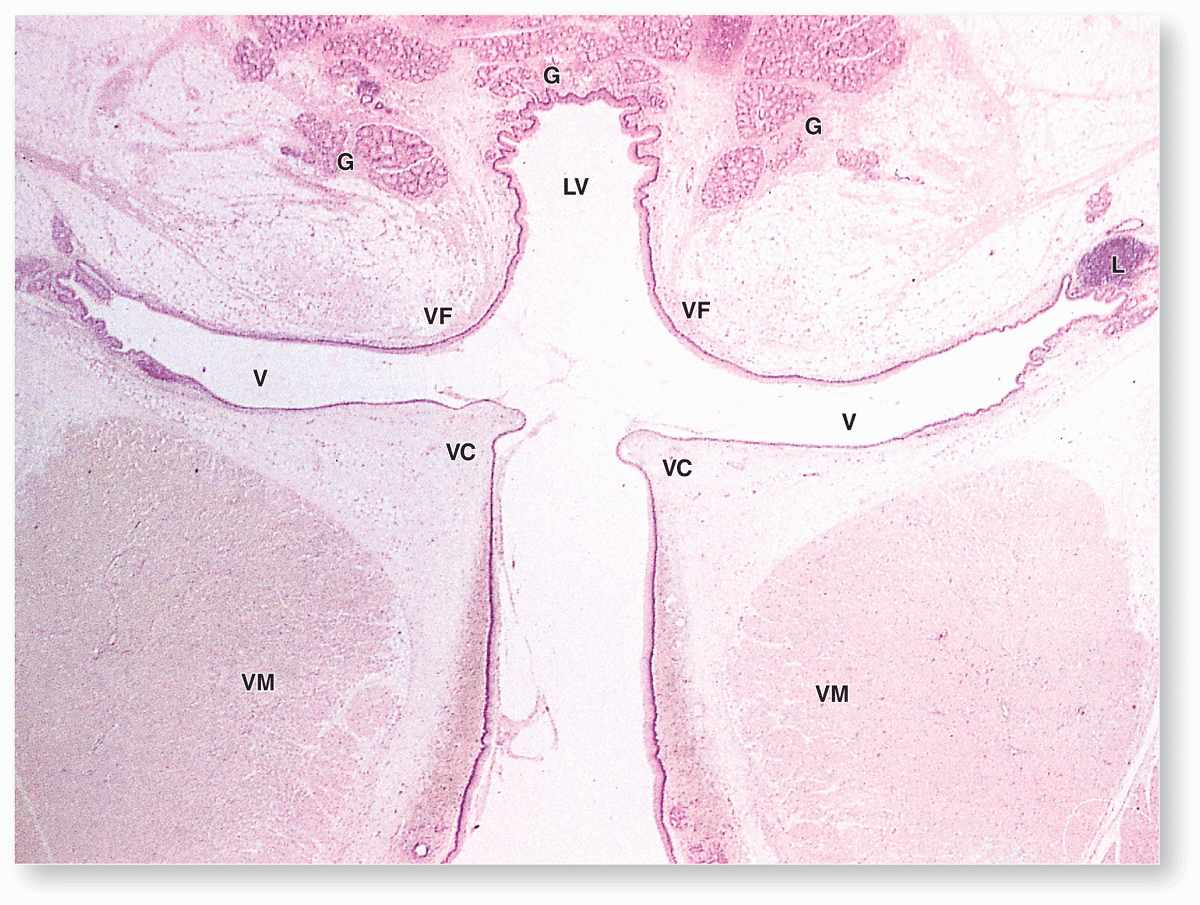
 MEDICAL APPLICATION
MEDICAL APPLICATION