Chapter 5 PULMONARY DISEASES
Introduction
The lungs are part of the respiratory system. As such they have a critical role in the exchange of gases—the inhalation of oxygen (O2) and expiration of carbon dioxide (CO2). Pulmonary diseases are a major cause of human morbidity and mortality as evidenced by the following clinical and epidemiologic facts:
 Respiratory infections, usually localized to the upper respiratory passages, account for most of the so-called common diseases of children and adults of all ages.
Respiratory infections, usually localized to the upper respiratory passages, account for most of the so-called common diseases of children and adults of all ages.
 The respiratory system is essential for sustaining life, and thus respiratory failure is one of the major causes of death in humans.
The respiratory system is essential for sustaining life, and thus respiratory failure is one of the major causes of death in humans.
 Lungs are in contact with the external world and thus rather susceptible to deleterious exogenous influences. Most notably, lungs inhale living airborne pathogens, such as bacteria, viruses, and fungi. Organic and inorganic particles and fumes inhaled in the air also may adversely affect the lungs.
Lungs are in contact with the external world and thus rather susceptible to deleterious exogenous influences. Most notably, lungs inhale living airborne pathogens, such as bacteria, viruses, and fungi. Organic and inorganic particles and fumes inhaled in the air also may adversely affect the lungs.
 The lungs are major “shock-organs” in humans and show pathologic changes in almost all forms of shock and terminal conditions preceding death.
The lungs are major “shock-organs” in humans and show pathologic changes in almost all forms of shock and terminal conditions preceding death.
 Changes in the lungs are seen during heart failure and in many metabolic and circulatory disorders affecting other vital organs such as the brain, liver, and kidneys. Pulmonary edema and acute respiratory distress syndrome (ARDS) are common findings in multiple organ failure.
Changes in the lungs are seen during heart failure and in many metabolic and circulatory disorders affecting other vital organs such as the brain, liver, and kidneys. Pulmonary edema and acute respiratory distress syndrome (ARDS) are common findings in multiple organ failure.
 The lungs are affected by exogenous carcinogens and are the primary target for the carcinogens contained in tobacco smoke. Lung cancer is still the foremost cause of cancer-related death in both men and women.
The lungs are affected by exogenous carcinogens and are the primary target for the carcinogens contained in tobacco smoke. Lung cancer is still the foremost cause of cancer-related death in both men and women.
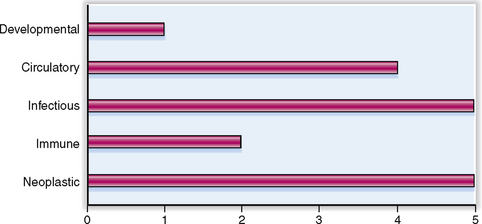
Lung diseases can be classified according to their etiology. The relative clinical significance of various pulmonary diseases is presented graphically in Figure 5-1.
Anatomy and Physiology
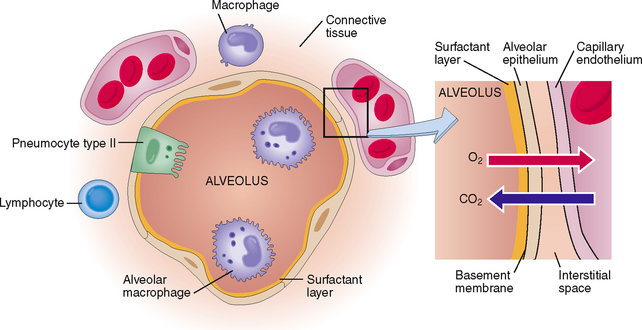
Alveolus (“acinus”) Small saclike part of the lungs forming the smallest respiratory unit of the lungs. It is lined by two cell types: pulmonary pneumocytes type I, which form the air–blood interface, and pneumocytes type II, which secrete surfactant.
Bronchioli Small bronchi that lack cartilage. They are interposed between the bronchi with the alveolar ducts and alveoli and further classified as terminal or respiratory bronchioli.
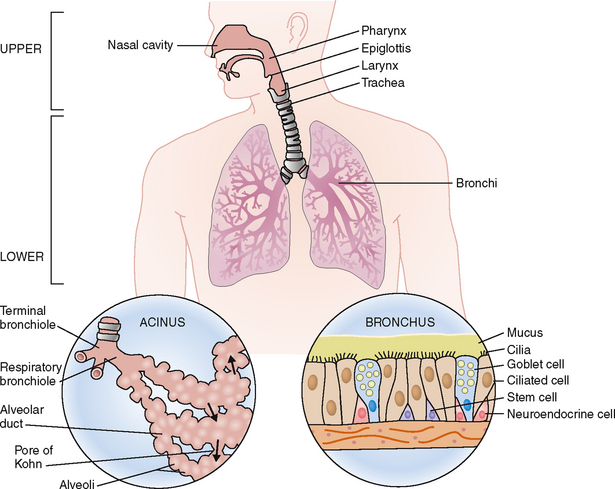
Bronchus Tubular part of the airways inside the lungs arranged into a branching tree of progressively smaller and smaller ducts connecting the trachea on the proximal side and bronchioli and alveoli on the distal side. Bronchi are lined with respiratory epithelium composed of ciliated and nonciliated cylindrical cells, mucus-secreting cells, and neuroendocrine cells. Their walls contain cartilage and smooth muscle cells.
Compliance Measure of the ability of the lungs to expand in response to increased pressure by the inhaled air.
Diffusion Movement of molecules across a gradient from areas of high concentration to ones of low concentration, until equilibrium is achieved.
Elasticity Ability of a material to return to its normal shape after a force has changed its shape. The elasticity of lungs is measured as a change of pressure in response to changes of the volume of intrapulmonary air.
Larynx Part of the respiratory tract between the pharynx and the trachea, which also acts as voice-generating organ.
Mucus Gel-like substance covering the surface of mucous membranes of air spaces, such as the nose, trachea, and bronchi.
Pharynx Part of the respiratory and alimentary systems connecting the nose with the larynx and the mouth with the esophagus.
Pleura External covering of the lungs composed of a mesothelial layer and underlying connective tissue. The visceral pleura covering the lungs is continuous with the parietal pleura covering the inside of the thoracic cage. The pleural cavity is the space between the visceral and parietal pleura. Normally it contains a few milliliters of serous fluid lubricating the pleural surfaces and allowing them to glide one over another during respiration.
Pulmonary surfactant Complex semiliquid surface-tension–generating material covering the surface of the alveoli. It is essential for keeping the alveoli open during inhalation. The deficiency of surfactant is the cause of neonatal respiratory distress syndrome and hyaline membrane formation in the lungs of premature babies.
Respiration (breathing) Process that includes external and internal respiration. External respiration refers to inhalation of air into the lungs and expiration of air out of the respiratory system, as well the gas exchange between inhaled air and the blood in the lungs. Inhalation provides oxygen, and expiration allows the elimination of carbon dioxide out of the body. Internal respiration refers to cellular processes allowing the transfer of oxygen from red blood cells through the capillary wall into the tissues and intracellular utilization of oxygen.
Trachea Air-conducting tube connecting the larynx with the bronchi.
Ventilation Movement of air in and out of the lungs.
Ventilation/perfusion rate (![]() /
/![]() ) Ratio of the overall alveolar ventilation to the overall pulmonary blood flow expressed in liters per minute, normally 0.8.
) Ratio of the overall alveolar ventilation to the overall pulmonary blood flow expressed in liters per minute, normally 0.8.
Clinical and Laboratory Findings and Procedures
Acidosis Decreased blood pH resulting from an abnormal accumulation of acids or a loss of bases from the body fluids. May be classified as respiratory or metabolic.
Alkalosis Increased blood pH resulting from an abnormal accumulation of bases or a loss of acids from body fluids. May be classified as respiratory or metabolic.
Allergy Generic term for many forms of hypersensitivity to foreign substances capable of inducing an immune response. Such substances are called allergens or immunogens.
Anoxia Condition in which the tissues do not receive oxygen. If partial, it is called hypoxia.
Cheyne-Stokes respiration Abnormal respiration characterized by periods of apnea and rapid breathing. Typically apnea lasts 10 to 30 seconds and is followed by a period of rapid and deepening respiratory movements, followed again by slowing down of respiration and apnea.
Cough Process resulting in the forceful expulsion of air from the respiratory tract. It may by mediated by a reflex or a voluntary expiratory effort.
Dyspnea (“shortness of breath”) Sense of difficulty with breathing.
Expectoration Process that results in removal of mucus or tracheobronchial contents during coughing and spitting.
Forced vital capacity Maximum volume of gases that can be exhaled from the lungs as fast as possible over a specified short period of time.
Functional residual capacity Volume of air that remains in the lungs after a normal expiration. It can be calculated by adding the expiratory reserve volume and the residual volume.
Hyperinflation Excessive expansion of the pulmonary air spaces that occurs due to air trapping in asthma or because of the loss of alveolar walls in emphysema.
Hyperpnea Increased depth of respiratory movements without an increased number of respirations.
Hyperventilation Increased alveolar air exchange leading to increased exhalation of carbon dioxide and hypocapnia.
Inspiratory capacity Volume of air that can be inhaled after a normal exhalation. It can be calculated by adding the tidal volume to the inspiratory reserve volume.
Intubation Passage of a tubular instrument into the air spaces, typically through the nose or the larynx. It is used to facilitate or maintain the air flow into the lungs or administer inhalational anesthetics.
Kussmaul respiration Form of abnormal breathing characterized by increased depth and rate. It is typically encountered in acidosis, especially lactic acidosis of diabetes.
Rales (“crackles”) Abnormal sounds heard over the regions of the thorax by auscultation during inspiration. These sounds result from the accumulation of fluid or exudates in the alveoli.
Shunting Process during which a stream of blood or air is diverted from its normal flow through expanded normal, newly formed or pathological passages.
Pulmonary Diseases
Acute respiratory distress syndrome (“shock lung”) Clinical syndrome caused by numerous exogenous and endogenous insults leading to diffuse alveolar-capillary unit damage (DAD). Most often caused by shock, airborne or blood-borne infections, chemical or physical injury of the lungs, or systemic metabolic disorders.
Asthma Inflammatory disease characterized by reversible obstruction of the air passages due to bronchospasm and oversecretion of mucus.
Atelectasis Process in which the lungs become airless and the alveolar spaces collapse.
Bronchiectasis Chronic lung disease characterized by irreversible dilatation of bronchi and bronchioli caused by inflammation, obstruction, or fibrosis, or various destructive changes in the peribronchial lung parenchyma.
Bronchitis Inflammation of bronchi that may be acute or chronic. It may be caused by viral or bacterial infection or chronic irritation, as seen in smokers. Clinically it presents with cough and expectoration of mucus or mucopurulent exudate.
Chronic obstructive pulmonary disease (COPD) Chronic lung disease caused by chronic bronchitis or emphysema or both. It is most often caused by smoking. Clinically it manifests as progressive dyspnea and signs of obstructive lung disease leading to respiratory insufficiency.
Emphysema Chronic condition caused by destruction of alveolar septa and dilatation of terminal air spaces. It occurs in several pathologic forms (e.g., centriacinar or panacinar), and clinically it manifests as chronic obstructive pulmonary disease. It may be a consequence of congenital α1-antitrypsin deficiency.
Empyema Localized accumulation of pus in the pleural cavity.
Hypersensitivity pneumonitis Group of lung diseases caused by a cellular immune reaction to exogenous organic allergens inhaled into the alveoli. These diseases are often related to the workplace and are known as farmer’s lung, pigeon breeder’s lung, and air conditioner lungs, among others.
Kartagener’s syndrome Congenital ciliary dismotility disorder characterized by recurrent respiratory infections (sinusitis and bronchiectasis), situs inversus, and infertility in males (sperm immotility).
Lung cancer Group of malignant tumors originating from the bronchi or terminal bronchioli and pleura. Most often caused by smoking. Microscopically, lung cancer can be classified as squamous cell carcinoma, adenocarcinoma, or large- or small-cell undifferentiated carcinoma. Clinically these tumors are divided for practical purposed into two groups: small-cell carcinoma and nonsmall-cell carcinoma, including all the other microscopic variants.
Mesothelioma Malignant tumor of the pleura, often related to asbestos exposure.
Pleural effusion Accumulation of fluid in the pleural cavity. It may represent a transudate, as occurs in chronic heart failure, or generalized anasarca; or it may be an exudate, as is seen in infectious pleuritis. Tumors also cause pleural effusion (“malignant pleural effusion”).
Pleuritis Inflammation of the pleura. It may be a complication of pneumonia or it may begin as a primary infection.
Pneumoconioses Group of chronic lung diseases caused by inhalation of inorganic and organic particles, chemical fumes, and vapors. Typical entities included under this heading are coal worker’s pneumoconiosis, silicosis, asbestosis, and conditions such as farmer’s lung, bagassosis, byssinosis, and various occupational lung disease caused by vapor inhalation.
Pneumonia Inflammation of the lungs. It can be acute or chronic and involve predominantly either the alveoli (“alveolar pneumonia”) or alveolar septa (“interstitial pneumonia”). Pneumonia may be patchy (“lobular pneumonia” or “bronchopneumonia”) or diffuse (“lobar pneumonia”).
Pneumothorax Accumulation of air in the pleural cavity.
Pulmonary hypertension Increased pressure in the pulmonary circulation, typically reaching 25% of the systemic blood pressure. It may be primary, of unknown origin, or secondary, due to left heart failure and chronic lung disease or pulmonary emboli.
Restrictive lung disease Group of pathogenetically unrelated diseases characterized by reduced volume of terminal air spaces or an inability of the lungs to expand adequately during inspiration. Restrictive lung disease can be distinguished from obstructive lung disease by functional testing. This group of disease includes several forms of chronic interstitial pneumonia of unknown origin, dust-induced pneumoconioses, drug- and radiation-induced lung diseases, hypersensitivity pneumonias, and diseases of presumed immune origin such as sarcoidosis.
Sarcoidosis Systemic disease of unknown origin, characterized by the formation of noncaseating granulomas in the lungs, thoracic lymph nodes, and many other organs.
Usual interstitial pneumonia (UIP, idiopathic pulmonary fibrosis) Chronic restrictive lung disease causing irregular destruction of lung parenchyma associated with chronic alveolitis and patchy interstitial fibrosis (“honeycomb lungs”). In most instances the cause of UIP is unknown. The disease is incurable.
Normal Structure and Function
ANATOMY AND HISTOLOGY
The respiratory system is arbitrarily divided into two parts: (1) the upper respiratory system, comprising the nose, pharynx, and larynx, and (2) the lower respiratory system, comprising the tracheobronchial tree and the lungs (Fig. 5-2). In this chapter we concentrate on the lower respiratory tract, its functions, and diseases.
The respiratory tract is lined with specialized epithelia and encased by specialized support structures.
Because the nasal air spaces and the tracheobronchial tree need to be kept patent, their walls contain cartilage. Bony structures in the nasal air passages have the same protective functions. In the tracheobronchial tree the air spaces contain smooth muscle cells, which are thought to regulate the contraction or dilatation of these air spaces designed for conductance and distribution of air in the lungs.
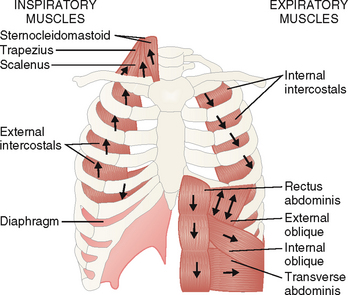
Lungs are enclosed in the thoracic cage, which protects them from external injury but also contributes to their rhythmic expansion and reduction in size.
The thoracic cage consists of bones and striated muscles (Fig. 5-3). It has two principal functions:
 Protection. The sternum, ribs and vertebrae, clavicle, and scapula protect the lungs from external injury by providing a mechanical shield. The muscles of the chest and the back provide additional protection.
Protection. The sternum, ribs and vertebrae, clavicle, and scapula protect the lungs from external injury by providing a mechanical shield. The muscles of the chest and the back provide additional protection.
 Respiration. The striated muscles of the anterior and posterior surface of the chest wall, some neck and anterior abdominal wall muscles, and the diaphragm participate in the respiratory movements. These muscles could be divided into two groups: (1) inspiratory muscles, such as sternocleiodmastoid, trapezius and scalenus muscles, and the diaphragm, and (2) the expiratory muscles, such as the intercostals and the muscles of the anterior abdominal wall.
Respiration. The striated muscles of the anterior and posterior surface of the chest wall, some neck and anterior abdominal wall muscles, and the diaphragm participate in the respiratory movements. These muscles could be divided into two groups: (1) inspiratory muscles, such as sternocleiodmastoid, trapezius and scalenus muscles, and the diaphragm, and (2) the expiratory muscles, such as the intercostals and the muscles of the anterior abdominal wall.
The lungs receive venous blood, which is oxygenated in the lungs and distributed through the arterial circulation.
The lungs receive the venous blood from the right heart, which in turn is the main confluence of the superior and inferior venae cavae. The blood enters the lungs through the pulmonary artery, which branches into progressively smaller branches. Ultimately the blood enters into capillaries, which are found in the alveolar septa, thus forming the alveolar-capillary units (Fig. 5-4). The red blood cells of the venous blood release CO2, which enters the alveolar spaces and is exhaled into the outside air. Oxygen inhaled from the air crosses the alveolar membrane that is formed from the attenuated cytoplasm of type I pneumocytes. Thereafter it passes through the capillary membranes, enters the blood, and binds to the hemoglobin of red blood cells. The oxygenated blood leaves the alveolar-capillary units and enters the pulmonary venules, from which it reaches the pulmonary veins, the left heart, and ultimately the arterial circulation.
Several cellular systems protect the lungs from airborne pathogens, allergens, and harmful particulate material.
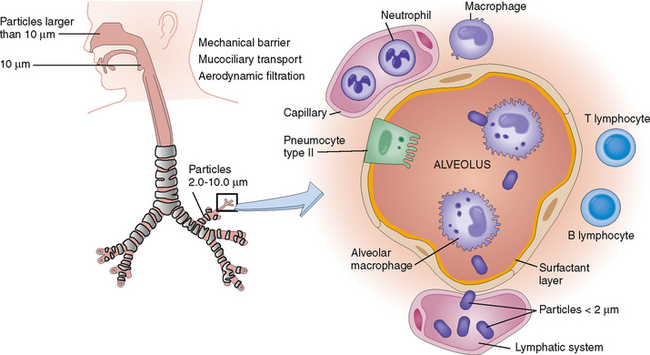
The air inhaled through the nose or the mouth contains potentially noxious agents, including viruses, bacteria, and various organic and inorganic particles. The most important protective mechanisms (Fig. 5-5) are as follows:
Mucociliary clearance. The mucus produced by the goblet cells in the nasal mucosa or the tracheobronchial epithelium covers the entire surface of the air-conducting tubular part of the respiratory system. The bronchi also contain mucous glands. The mucus they secrete consists of glycosaminoglycans, glycoproteins, and complex carbohydrates. The mucus can bind living pathogens and other particulate matter. Bactericidal substances in the mucus, such as properdin, or immunoglobulin A, act on bacteria. Mucus also contains macrophages, which phagocytose or kill bacteria. These bacteria and other particulate matter are moved up the tracheobronchial tree through the ciliary movement of the columnar cells in the tracheobronchial epithelium. This mucociliary escalator system will, under normal circumstances, eliminate most of the particles that measure 2 to 10 μm in diameter, but particles that are smaller than 2 μm may reach the alveoli. Such particles are usually taken up by alveolar macrophages and either are expectorated or enter into the interstitial spaces and ultimately are carried by the lymph into the local lymph nodes.
PHYSIOLOGY
Ventilation is a process during which the air moves in and out of the lungs.
VE = f × VT
In normal adults the VT is approximately 500 mL/min, and in children 3 to 5 mL/kg/min.
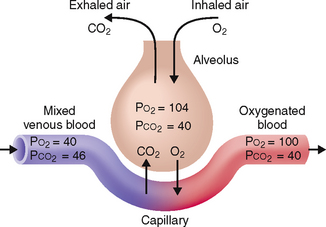
Partial pressure of gases is the key determinant of external and internal respiration.
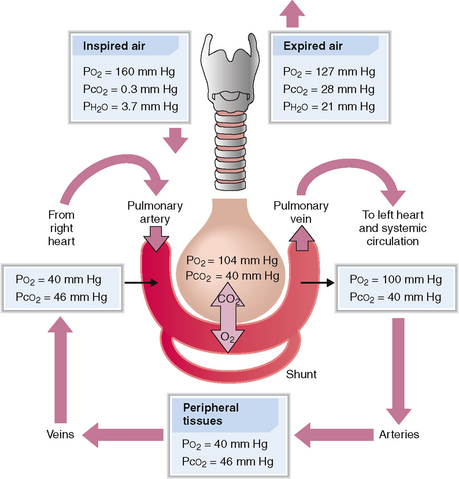
External respiration takes place in the lungs. During this process the O2 from the inhaled air is transferred to the blood and the CO2 diffuses from blood into the air. Internal respiration refers to cellular processes that allow the transfer of O2 from red blood cells through the capillary wall into the tissues and thereby for use within the cell. Both processes depend on the partial pressures of O2 and CO2 (Fig. 5-6). Note in Figure 5-6 that the consumption of O2 leads to major fluctuations in the partial pressure of O2, which drops from 100 mm Hg in the arterial blood to 40 mm Hg in venous blood. In contrast, the fluctuations of CO2 are much smaller, from 40 mm Hg in arterial blood to 46 mm Hg in venous blood.
Transfer of gases in the alveolar-capillary unit occurs by simple diffusion.
The transition of O2 from air into the blood and CO2 from blood to the air occurs through diffusion across the alveolar lining and the basement membranes of the alveolar capillaries (Fig. 5-7). This process is governed by Fick’s law as stated here:
where Vgas = volume of gas transferred per unit of time
D = diffusion coefficient of the gas
A = surface area of the diffusion membrane
P1 – P2 = partial pressure of gas on each side of the diffusion membrane, which in the lungs includes two pressure gradients: one across the alveolar wall and the other across the capillary basement membrane
Oxygen pressure in inspired dry air is higher than in the humidified air in the trachea or the alveoli or the oxygenated arterial blood leaving the lungs.
Assuming that the air contains 21% O2, at sea level the oxygen pressure in dry inhaled air is 160 mm Hg (760 × 0.21 = 160). This air is humidified during its passage through the nose and trachea, which brings down the oxygen pressure to 150 mm Hg (see Fig. 5-7). As the air passes into the alveoli, the oxygen pressure drops to 100 mm Hg. This is in part due to the fact that oxygen diffuses rather rapidly into the blood and is also diluted with CO2 diffusing from the venous blood into the alveoli.
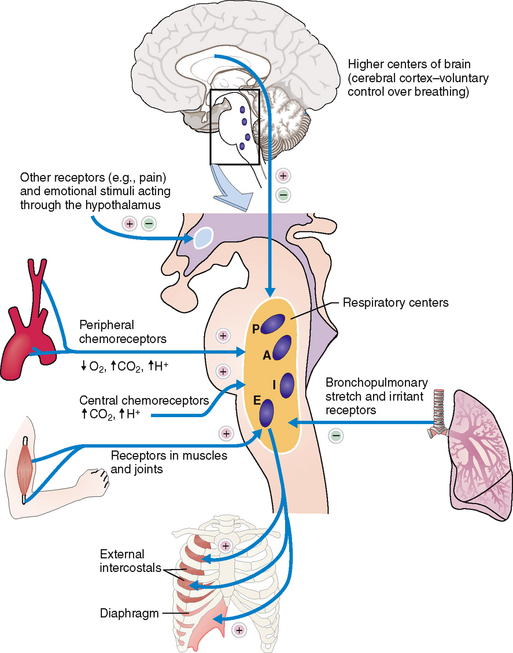
Breathing is an involuntary action that is under the control of the respiratory center in the brainstem.
Breathing is a vital function that is tightly controlled by the central nervous system, which receives impulses from the periphery and then sends efferent signals to the periphery (Fig. 5-8). The key anatomic foci of the respiratory control sensory and effector system are as follows:
 Respiratory control centers in the medulla and the pons
Respiratory control centers in the medulla and the pons
 Central and peripheral chemoreceptors
Central and peripheral chemoreceptors
 Mechanoreceptors in the lungs, muscle, and joints
Mechanoreceptors in the lungs, muscle, and joints
Chemoreceptors. Chemoreceptors can be classified as central or peripheral.
 Central chemoreceptors located in the brainstem act directly on the inspiratory center. They respond to changes in the pH of the cerebrospinal fluid; its acidity stimulates inspiration, whereas the increased pH slows down the respiratory movements.
Central chemoreceptors located in the brainstem act directly on the inspiratory center. They respond to changes in the pH of the cerebrospinal fluid; its acidity stimulates inspiration, whereas the increased pH slows down the respiratory movements.
 Chemoreceptors in the carotid and aortic bodies respond to the Paæ{2, Pa{2, and pH, sending stimuli to the inspiratory center. Reduced P{2, decreased Pæ{2, and decreased pH increase the rate of respiration.
Chemoreceptors in the carotid and aortic bodies respond to the Paæ{2, Pa{2, and pH, sending stimuli to the inspiratory center. Reduced P{2, decreased Pæ{2, and decreased pH increase the rate of respiration.
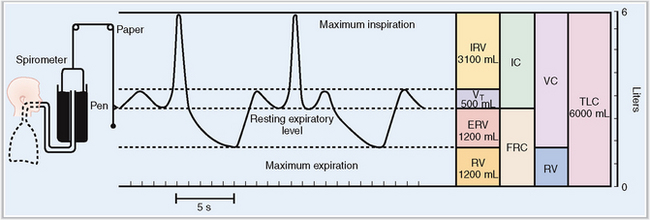
The volume of air entering and leaving the lungs during inspiration and expiration can be measured objectively under controlled circumstances.
Normal breathing occurs in a cycle that includes four phases: rest, inspiration, a rest phase, and expiration. By measuring the volume of air entering the lungs during inspiration and leaving it during expiration the critical aspects of respiratory capacity can be defined as illustrated in Figure 5-9. By convention these static lung volumes are defined as follows:
 Tidal volume (VT)—the amount of air entering and leaving the lung with each breath in a person who is breathing normally. In adults it measures approximately 500 mL.
Tidal volume (VT)—the amount of air entering and leaving the lung with each breath in a person who is breathing normally. In adults it measures approximately 500 mL.
 Functional residual capacity (FRC)—the amount of air remaining in the lungs after expiration in a person who is breathing normally. FRC cannot be measured by routine spirometry, but can be measured by the helium dilution method, the nitrogen washout technique, or whole-body plethysmography.
Functional residual capacity (FRC)—the amount of air remaining in the lungs after expiration in a person who is breathing normally. FRC cannot be measured by routine spirometry, but can be measured by the helium dilution method, the nitrogen washout technique, or whole-body plethysmography.
 Expiratory reserve volume (ERV)—the amount of air that can be exhaled from the lungs by forceful expiration.
Expiratory reserve volume (ERV)—the amount of air that can be exhaled from the lungs by forceful expiration.
 Residual volume (RV)—the amount of air remaining in the lungs after forceful expiration. RV is calculated by subtracting ERV from FRC (RV = FRC − ERV). In young adults it accounts for 20% of the total lung capacity. It increases by 1% per year and in older individuals it accounts for more than 60% of the total lung capacity.
Residual volume (RV)—the amount of air remaining in the lungs after forceful expiration. RV is calculated by subtracting ERV from FRC (RV = FRC − ERV). In young adults it accounts for 20% of the total lung capacity. It increases by 1% per year and in older individuals it accounts for more than 60% of the total lung capacity.
 Inspiratory reserve volume (IRV)—the amount of air that can be forcefully inhaled in addition to the VT.
Inspiratory reserve volume (IRV)—the amount of air that can be forcefully inhaled in addition to the VT.
 Inspiratory capacity (IC)—the amount of air that can be inhaled into the lungs in addition to the air accounting for the FRC (IC = VT + IRV).
Inspiratory capacity (IC)—the amount of air that can be inhaled into the lungs in addition to the air accounting for the FRC (IC = VT + IRV).
 Vital capacity (VC)—the amount of air expelled from the lungs during forceful expiration.
Vital capacity (VC)—the amount of air expelled from the lungs during forceful expiration.
 Total lung capacity (TLC)—the total amount of air inside the lungs and the bronchial tree after maximal inspiration.
Total lung capacity (TLC)—the total amount of air inside the lungs and the bronchial tree after maximal inspiration.
 Forced vital capacity (FVC)—the amount of air that can be expelled from the lungs if a person is told to exhale as fast as possible. Normally FVC does not differ from VC. However, FVC can be prolonged due to air trapping that occurs in persons who have emphysema.
Forced vital capacity (FVC)—the amount of air that can be expelled from the lungs if a person is told to exhale as fast as possible. Normally FVC does not differ from VC. However, FVC can be prolonged due to air trapping that occurs in persons who have emphysema.
 Forced expiratory volume (FEV1)—the amount of air that can be expired in 1 second following maximal inspiration. FEV1 in healthy young adults is normally 80% of the forced vital capacity (FEV1/FVC = 0.8), but with aging FEV1 is reduced to 65% to 70%. FEV1/FVC is effort-dependent and is influenced by increased expiratory effort. In obstructive lung diseases FEV1 is reduced (FEV1/FVC < 70%). In restrictive lung diseases, both FEV1 and FVC are reduced (FEV1/FVC > 70%).
Forced expiratory volume (FEV1)—the amount of air that can be expired in 1 second following maximal inspiration. FEV1 in healthy young adults is normally 80% of the forced vital capacity (FEV1/FVC = 0.8), but with aging FEV1 is reduced to 65% to 70%. FEV1/FVC is effort-dependent and is influenced by increased expiratory effort. In obstructive lung diseases FEV1 is reduced (FEV1/FVC < 70%). In restrictive lung diseases, both FEV1 and FVC are reduced (FEV1/FVC > 70%).
 Forced expiratory flow rate (FEF25–75%)—the rate of air flow over the middle (25% to 75%) half of the FVC. It is also called maximal midexpiratory flow rate and is considered to be the most sensitive parameter for identifying early obstruction. It reflects the status of small airways and it is effort-independent.
Forced expiratory flow rate (FEF25–75%)—the rate of air flow over the middle (25% to 75%) half of the FVC. It is also called maximal midexpiratory flow rate and is considered to be the most sensitive parameter for identifying early obstruction. It reflects the status of small airways and it is effort-independent.
Clinical and Laboratory Evaluation of Pulmonary Diseases
The evaluation of patients who may have lung diseases includes a complete history and physical examination, with special emphasis on symptoms that may be related to respiratory problems. In addition chest radiographs, laboratory test data, and acid–base balance must be reviewed. Spirometry and testing of respiratory function may be indicated. Bronchoscopy, thoracentesis, and fine-needle or tissue biopsy are required in certain conditions.
FAMILY AND PERSONAL HISTORY
A family history and a personal history are essential for identifying some of the major risk factors for lung diseases. Examples of such associations that can be discovered by carefully interviewing the patient or his family are given in Table 5-1.
Table 5-1 Risk Factors for Lung Diseases
| TYPE OF RISK FACTOR | SPECIFIC DISEASES–RISK FACTOR ASSOCIATIONS |
| Hereditary factors | |
| Social and work-related factors | |
| Infections | |
| Medical and surgical procedures | |
| Drugs/toxins | Drug-induced lung diseases: Numerous drugs can cause lung diseases |
| External mechanical factors |
AAT, α1-antitrypsin; AIDS, acquired immunodeficiency syndrome; ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease; URD, upper respiratory disease.
SIGNS AND SYMPTOMS OF LUNG DISEASES
The most important signs and symptoms of lung diseases are as follows:
Dyspnea is a sensation of breathlessness out of proportion to the level of physical activity.
As discussed in Chapter 4, dyspnea can be classified as cardiac or noncardiac, acute or chronic. The most important causes of dyspnea are listed in Table 5-2.
| TYPE OF DYSPNEA | PATHOGENESIS | CLINICAL CONDITIONS |
| Pulmonary dyspnea | Obstruction of airways | |
| Alveolar filling | ||
| Interstitial lung disease | ||
| Pulmonary artery obstruction | ||
| Pleural disease | ||
| Cardiac dyspnea | Left heart failure | Myocardial infarction |
| Pericardial disease | Pericardial tamponade | |
| Endocardial defect | Chronic endocarditis | |
| Other forms of dyspnea | Loss of RBC/Hb/O2 transport | |
| Hypoperfusion of lungs | Multiple organ failure (shock) | |
| Psychogenic | Anxiety, panic attack | |
| Neuromuscular diseases | Myopathy/muscular dystrophy | |
| Thoracic deformities | Kyphoscoliosis |
RBC/Hb/O2, red blood cell/hemoglobin/oxygen.
Patients also can describe the time of onset and the duration of shortness of breath. The timing of dyspnea provides important diagnostic clues, as listed in Table 5-3.
Table 5-3 Classification of Dyspnea by Type of Onset
ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease.
Data from Warrell DA, Cox TM, Firth JD (eds): Oxford Textbook of Medicine, 4th ed. Oxford, Oxford University Press, 2003.
Cough involves a reflex that can be triggered by a wide variety of stimuli.
 Deep inspiration leads to increased air content of the chest.
Deep inspiration leads to increased air content of the chest.
 Closure of the glottis concomitant with an expiratory effort results in increased intrathoracic pressure.
Closure of the glottis concomitant with an expiratory effort results in increased intrathoracic pressure.
 Opening of the glottis while the expiratory muscles contract propels the air under high pressure into the oropharynx and into the atmosphere.
Opening of the glottis while the expiratory muscles contract propels the air under high pressure into the oropharynx and into the atmosphere.
Cough may be clinically classified as acute, lasting a few days or a week or two, or chronic if it last more than 3 weeks. It may be accompanied by bleeding or sputum production (productive cough). Some irritants that cause cough may also cause bronchospasm, and in such cases cough is associated with wheezing (e.g., in asthma). Cough may be the only complaint, but often it is just one of the symptoms of a complex disease such as asthma or bronchopneumonia. The most important causes of cough are listed in Table 5-4.
ACE, angiotensin-converting enzyme; COPD, chronic obstructive pulmonary disease; GERD, gastroesophageal reflux disease.
Hemoptysis may present as mild, in the form of blood-stained sputum, or massive and life-threatening.
Hemoptysis is defined as expectoration of blood from the respiratory tract. Most often it originates from the bronchial arterial circulation, but it may have other sources as well. Remember that the bronchial arteries are part of the greater arterial system, and the blood in these arteries circulates under much higher pressure than the blood in the pulmonary venous or arterial circulation, which are low-pressure systems. Hence, if these vessels rupture, the bleeding occurs under much higher pressure than if it stemmed from pulmonary arteries and veins. However, if the pressure inside the pulmonary circulation rises, as in pulmonary hypertension, bleeding may occur from other vessels as well. Tumors may cause bleeding by eroding into any blood vessel. Autoimmune diseases, such as Wegener’s granulomatosis or Goodpasture’s syndrome, may cause vascular lesions, leading to a rupture of various blood vessels from small capillaries to larger arteries and veins. The most important causes of hemoptysis are listed in Table 5-5.
Table 5-5 Sources and Causes of Hemoptysis
| SITE | LESION/CAUSE | DISEASES |
| Bronchi | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|