17
Pharmacotherapy of Heart Failure
This chapter will be most useful after having a basic understanding of the material in Chapter 28, Pharmacotherapy of Heart Failure in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. In particular, the reader is directed to the following table:
• Table 28-3, Vasodilator Drugs Used to Treat Heart Failure, which shows drugs used as vasodilators to treat heart failure including their mechanism of action and their effects on preload and afterload
LEARNING OBJECTIVES
 Know the stages of heart failure and the treatments that are recommended at each stage.
Know the stages of heart failure and the treatments that are recommended at each stage.
 Understand the rationale for the use of drugs that prevent and slow the progression of heart failure.
Understand the rationale for the use of drugs that prevent and slow the progression of heart failure.
 Understand the mechanism of action of inotropic drugs and how they are used to maintain left ventricular function.
Understand the mechanism of action of inotropic drugs and how they are used to maintain left ventricular function.
 Identify the major side effects and adverse drug reactions of the drugs used to treat heart failure.
Identify the major side effects and adverse drug reactions of the drugs used to treat heart failure.
DRUGS IN THIS CHAPTER
• Bisoprolol (ZEBETA)
• Candesartan (ATACAND)
• Captopril (CAPOTEN, others)
• Carvedilol (COREG, others)
• Digoxin (LANOXIN, others)
• Dobutamine (DOBUTREX, others)
• Dopamine
• Enalapril (VASOTEC, others)
• Eplerenone (INSPRA, others)
• Furosemide (LASIX, others)
• Hydralazine (APRESOLINE)
• Hydralazine and isosorbide dinitrate (BIDIL)
• Inamrinone (INOCOR)
• Isosorbide dinitrate (ISORDIL, SORBITRATE, others)
• Labetalol (NORMODYNE, TRANDATE, others)
• Lisinopril (PRINIVIL, ZESTRIL, others)
• Losartan (COZAAR)
• Metoprolol (LOPRESSOR, TOPROL XL, others)
• Milrinone (PRIMACOR IV)
• Minoxidil (LONITEN)
• Nesiritide (NATRECOR)
• Nitroglycerin (trinitroglycerin, NITROSTAT, NITRO-BID, others)
• Nitroprusside (NITROPRESS, others)
• Spironolactone (ALDACTONE)
• Thiazide diuretics (many, see Chapter 15)
• Valsartan (DIOVAN)
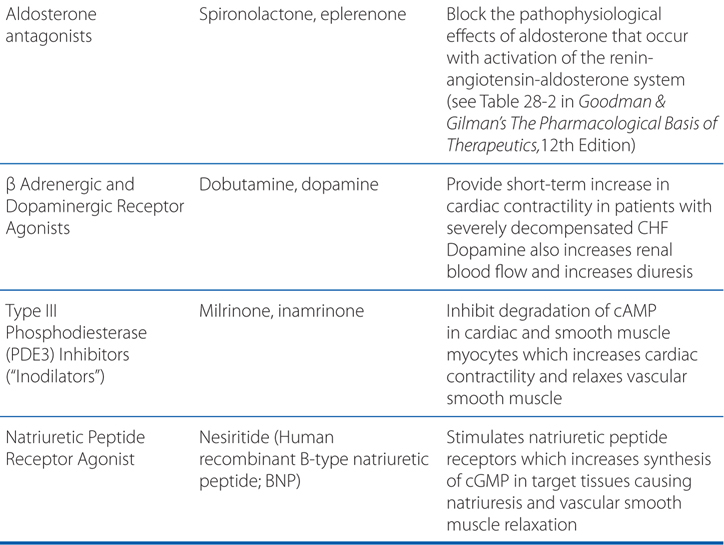
MECHANISMS OF ACTIONS OF DRUGS USED TO TREAT HEART FAILURE (SEE FIGURE 17-1)
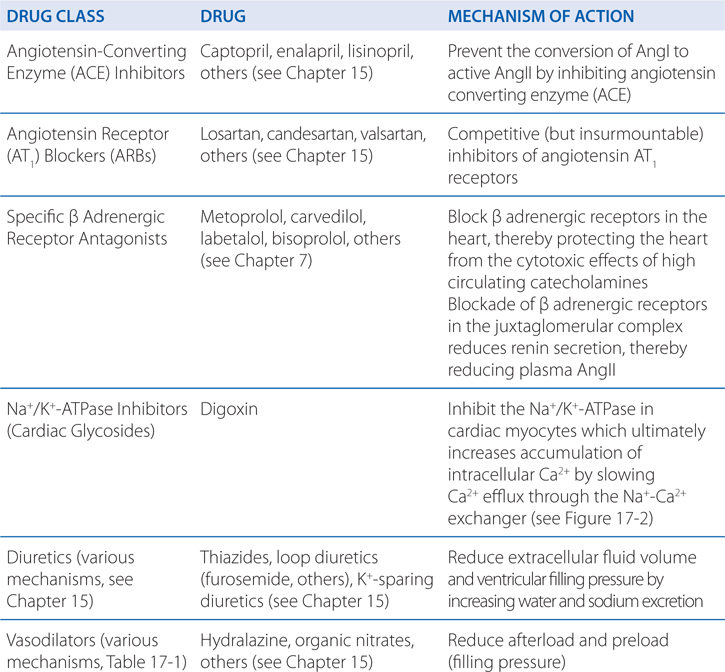
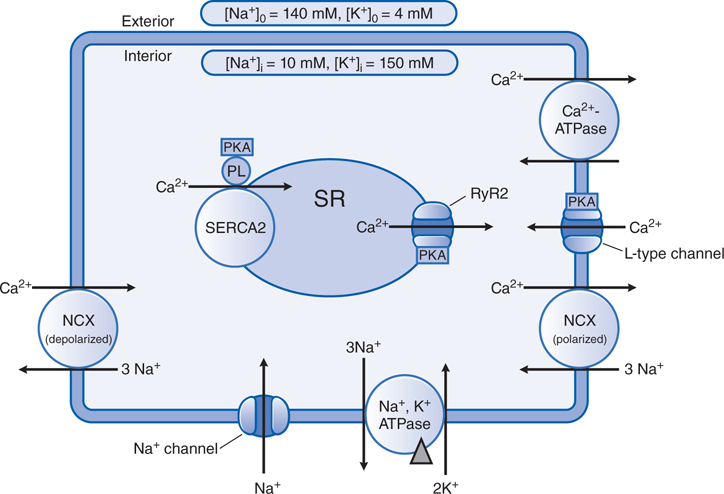
FIGURE 17-2 Sarcolemmal exchange of Na+ and Ca2+ during cell depolarization and repolarization. Na+ and Ca2+ enter the cardiac myocyte via the Na+ channel and the L-type Ca2+ channel during each cycle of membrane depolarization, triggering the release, through the ryanodine receptor (RyR), of larger amounts of Ca2+ from internal stores in the sarcoplasmic reticulum (SR). The resulting increase in intracellular Ca2+ interacts with troponin C and activates interactions between actin and myosin that result in sarcomere shortening. The electrochemical gradient for Na+ across the sarcolemma is maintained by active transport of Na+ out of the cell by the sarcolemmal Na+,K+-ATPase. The bulk of cytosolic Ca2+ is pumped back into the SR by a Ca2+-ATPase, SERCA2. The remainder is removed from the cell by either a sarcolemmal Ca2+-ATPase or a high-capacity Na+-Ca2+ exchanger, NCX. NCX exchanges 3 Na+ for every Ca2+, using the electrochemical potential of Na+ to drive Ca2+ extrusion. The direction of Na+-Ca2+ exchange may reverse briefly during depolarization, when the electrical gradient across the sarcolemma is transiently reversed. β Adrenergic agonists and PDE inhibitors, by increasing intracellular cyclic AMP levels, activate PKA, which phosphorylates phospholamban (PL), the α subunit of the L-type Ca2+ channel, and regulatory components of the RyR, as well as TnI, the inhibitory subunit of troponin (not shown). As a result, the probabilities of opening of the L-type Ca2+ channel and the RyR2 Ca2+ channel are doubled; SERCA2 is uninhibited and accumulates Ca2+ into the SR faster, more avidly, and to a higher concentration; and relaxation occurs at slightly higher [Ca2+]i due to slightly reduced sensitivity of the troponin complex to Ca2+. The net effect of these phosphorylations is a positive inotropic effect: a faster rate of tension development to a higher level of tension, followed by a faster rate of relaxation.  indicates site of cardiac glycoside binding. See the text in Chapter 28, Pharmacotherapy of Heart Failure in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition for the mechanism of positive inotropic effect of cardiac glycosides.
indicates site of cardiac glycoside binding. See the text in Chapter 28, Pharmacotherapy of Heart Failure in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition for the mechanism of positive inotropic effect of cardiac glycosides.
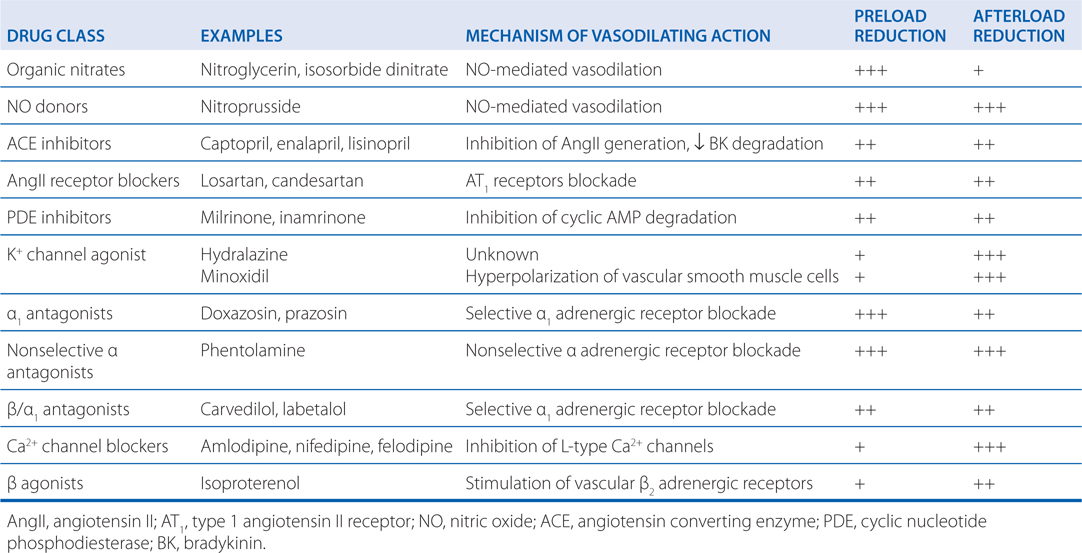
TABLE 17-1 Vasodilator Drugs Used to Treat Heart Failure
CHARACTERISTICS AND CAUSES OF HEART FAILURE
• Congestive heart failure (CHF) is a complex clinical syndrome characterized by:
▶ Impaired ventricular performance caused by the inability of the left ventricle to adequately fill (diastolic dysfunction) or empty (systolic dysfunction)
▶ Exercise intolerance
▶ A high incidence of ventricular arrhythmias
▶ Shortened life expectancy
• There is no single definitive diagnostic test for CHF
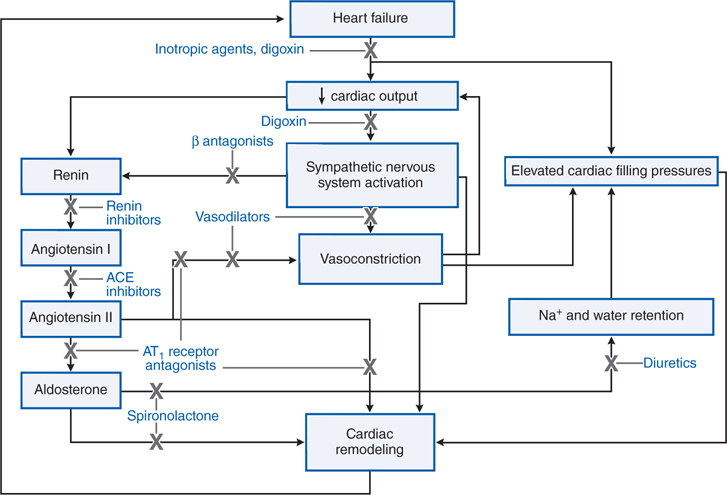
• Pathophysiological mechanisms that lead to congestive heart failure include activation of the sympathetic nervous system and renin-angiotensin-aldosterone axis (see Figure 17-1)
FIGURE 17-1 Pathophysiologic mechanisms of heart failure and major sites of drug action. Congestive heart failure is accompanied by compensatory neurohormonal responses, including activation of the sympathetic nervous and renin–angiotensin–aldosterone axis. Increased ventricular afterload, due to systemic vasoconstriction and chamber dilation, causes depression in systolic function. In addition, increased afterload and the direct effects of angiotensin and norepinephrine on the ventricular myocardium cause pathologic remodeling characterized by progressive chamber dilation and loss of contractile function. Key congestive heart failure medications and their targets of action are presented. ACE, angiotensin-converting enzyme; AT1 receptor, type 1 angiotensin receptor.
• Many diseases can lead to heart failure, with the most common in the United States being:
▶ Coronary artery disease
▶ Hypertension
▶ Diabetes mellitus
▶ Drug abuse
SYMPTOMS OF HEART FAILURE
• Fatigue
• Shortness of breath
• Rapid heart rate
• Fluid retention resulting in peripheral and pulmonary edema (congestion)
COMORBIDITIES COMMON IN HEART FAILURE
• Coronary artery disease (CAD)
• Atrial fibrillation (AF)
• Myocardial infarction (MI)
• Sudden cardiac death
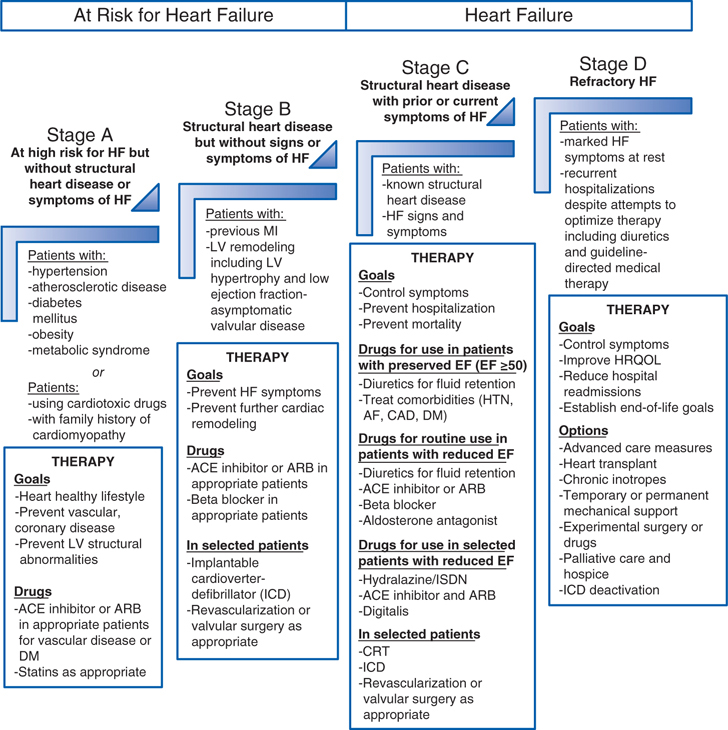
RATIONALE FOR PHARMACOLOGICAL THERAPY OF HEART FAILURE (See Figure 17-3)
FIGURE 17-3 Stages in the development of HF and recommended therapy by stage. ACE indicates angiotensin-converting enzyme; AF, atrial fibrillation; ARB, angiotensin-receptor blocker; CAD, coronary artery disease; CRT, cardiac resynchronization therapy; DM, diabetes mellitus; EF, ejection fraction; GDMT, guideline-directed medical therapy; HF, heart failure; HRQOL, health-related quality of life; HTN, hypertension; ICD, implantable cardioverter-defibrillator; LV, left ventricular; and MI, myocardial infarction. Preserved EF is defined as an EF ≥ 50%. Reduced EF is defined as an EF ≤ 40%. (Modified from Yancy CW et al. Circulation. 2013;128:e240-e327.)
• The goal of therapy for patients who are at risk of developing heart failure (Stages A and B) is to slow or stop the progression of the disease, decrease morbidity and mortality, and improve quality of life through the use of inhibitors of the renin-angiotensin-aldosterone system (ACE inhibitors and ARBs) and β adrenergic receptor blockers.
• ACE inhibitors, ARBs, and β blockers are also used in patients who have structural disease with symptoms of heart failure (Stages C and D), but additional therapies are added to treat symptoms of edema (diuretics), improve hemodynamics (inotropes and vasodilators), and facilitate natriuresis (dopamine and nesiritide).
A 64-year-old man who suffered a myocardial infarction at the age of 56 complains of difficulty sleeping because he wakes up feeling out of breath. Chest sounds reveal crackles and rales. He has difficulty walking more than 150 feet before having to stop to catch his breath. He is taking a β adrenergic blocker (metoprolol) and an ACE inhibitor (captopril). He also takes ibuprofen every day to relieve pain in his knees.
a. What Stage of heart failure is this patient in?
This patient is in Stage C (structural disease with current symptoms, see Figure 17-3). His prior myocardial infarction caused structural damage to his heart which is now impairing left ventricular function enough to cause symptoms of heart failure.
b. What is causing this patient’s symptoms?
This patient has developed pulmonary edema (congestion) because he is retaining Na+ and water due to activation of the renin-angiotensin-aldosterone axis. The patient has difficulty breathing at night when lying down because the pulmonary edema worsens and impairs ventilation and gas exchange. Heart failure patients with pulmonary congestion often sleep more comfortably if their head and upper body are elevated with a couple of pillows. The symptoms of exercise intolerance and shortness of breath are also the result of the patient’s heart failure.
c. Why is he taking a β blocker and an ACE inhibitor?
β Blocker therapy is recommended in patients who have had a myocardial infarction (see Chapter 16) because it reduces mortality. Certain β blockers are also recommended in many heart failure patients who can tolerate them because it blocks the deleterious effects of catecholamines and may lower the risk of arrhythmias. ACE inhibitors are recommended in patients with Stage B and C heart failure to slow disease progression by inhibiting the effects of angiotensin II.
d. What drugs, if any, should be added, changed, or withdrawn?
To relieve the symptoms of edema, diuretics are typically added to the medications of patients in Stage C heart failure. The patient should also be counseled to reduce sodium intake since that will also contribute to fluid retention. NSAIDs such as ibuprofen may also contribute to sodium and fluid retention and should be avoided, if possible. There is evidence that NSAIDs such as ibuprofen may increase the risk of cardiovascular events such as stroke in patients who have had an MI.
You are counseling a 34-year-old woman who is moderately overweight, and has mild hypertension and type II diabetes. Her father had his first myocardial infarction when he was 45 and died of a subsequent myocardial infarction when he was 52.
a. Is this patient at risk to develop heart failure and what can she do to lower her risks?
This woman has several risk factors for developing heart failure, including obesity, hypertension, diabetes, and her family history of cardiovascular disease. She may also have dyslipidemia. She is in Stage A of heart failure (high risk of developing heart failure but no symptoms). She has no control over her genetics, but she can reduce her risk of developing heart failure by controlling her weight, blood pressure, and diabetes.
b. What medications are recommended for this patient?
This patient may be able to reduce all of her controllable risks by adopting a healthier life-style (ie, regular exercise and adopting a healthier diet). If lifestyle modifications do not fully control her diabetes and hypertension, antidiabetic (see Chapter 30) and antihypertensive therapies (see Chapter 15) are recommended. The antihypertensives that would be most appropriate in this patient are ACE inhibitors or AT1 blockers (see Chapter 15). If she has dyslipidemia that is not controlled by diet and exercise, a lipid-lowering drug is recommended (see Chapter 20).
You are reviewing the medications of a 67-year-old man who has recently developed mild pulmonary congestion and peripheral edema. He has a history of mild heart failure, hypertension, and he occasionally suffers from angina. The drugs he is prescribed to take on a daily basis are aspirin, furosemide, lisinopril, lovastatin, metoprolol, and verapamil. He is also on a low-salt diet.
a. What are the possible reasons for the pulmonary congestion and peripheral edema?
Despite being on an ACE inhibitor (lisinopril), a β blocker (metoprolol), and a loop diuretic (furosemide), this patient is decompensating and retaining fluid. It’s possible the patient’s heart failure is worsening, or the patient is not adhering to the low-salt diet or is not taking his diuretic as prescribed.
b. What can be done to relieve this patient’s symptoms?
It is important to first eliminate any possible causes of the edema or worsening of heart failure. One drug that might be worsening the patient’s heart failure is verapamil, a calcium channel blocker that can lower left ventricular function. It should be possible to adequately control the patient’s hypertension using lisinopril, metoprolol, and furosemide. If a calcium channel blocker is needed to control the patient’s angina, a dihydropyridine calcium channel blocker (see Chapter 15) with minimal effects on left ventricular function is recommended. It is also important to determine whether the patient is adhering to a low-salt diet and is taking his diuretic and other drugs as prescribed.
BIDIL AND THE AFRICAN-AMERICAN HEART FAILURE TRIAL
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree