Classified as main duct, combined, or branch duct type
Clinical Issues
•
20-50% of resected cystic pancreatic tumors

Incidence increasing due to increased incidental detection on imaging for other reasons
•
Most patients are asymptomatic

Symptoms associated with intermittent pancreatic ductal obstruction by tenacious mucin &/or low-grade pancreatitis
•
Average age at presentation: Mid 60s
•
Prognosis better than conventional ductal adenocarcinoma

Noninvasive tumors: 5-year survival rate: > 75%

Invasive tumors: 5-year survival rate: 34-62%
–
Significantly better than pancreatic ductal adenocarcinoma

Invasive components may be very focal, requiring submission of entire lesion
•
Surgical resection treatment of choice

Vast majority surgically resectable
Macroscopic
•
Most common in pancreatic head
•
Often involve only portion of pancreatic duct but may be multifocal or involve entire duct
TERMINOLOGY
Abbreviations
•
Intraductal papillary mucinous neoplasm (IPMN)
Definitions
•
Grossly visible, mucin-producing epithelial neoplasm present within main pancreatic duct &/or its branches
•
Subclassification based on duct(s) involved

Main duct type
–
Mucinous epithelium confined to main pancreatic duct

Combined type
–
Mucinous epithelium involving both main duct and branch ducts

Branch duct type
–
Mucinous epithelium confined to branch ducts
ETIOLOGY/PATHOGENESIS
Molecular Features
•
DPC4/SMAD4 loss uncommon, in contrast to high-grade PanIN and invasive ductal adenocarcinoma
•
Overexpression of EGFR and ERBB2 common
•
KRAS mutations common except for oncocytic type
•
Loss of p16 increases with grade of dysplasia
Risk Factors
•
Family history of pancreatic ductal adenocarcinoma (associated with branch duct IPMN)
CLINICAL ISSUES
Epidemiology
•
Incidence

20-50% of resected cystic pancreatic tumors
–
Incidence increasing due to increased incidental detection on imaging for other reasons
–
Prevalence in general population estimated to be as high as 13.5% based on imaging studies
•
Age

Range: 25-94 years
•
Sex

Slightly more common in men but varies according to ethnicity
Presentation
•
Most patients asymptomatic
•
Symptomatic patients usually present with vague complaints related to duct obstruction/low-grade pancreatitis

Abdominal &/or back pain

Anorexia

Weight loss
•
Symptoms often present for months to years before diagnosis established
Endoscopic Findings
•
Mucin extravasation from patulous ampulla of Vater in ∼ 25% of cases, essentially diagnostic of intestinal-type IPMN
Treatment
•
Surgical resection is treatment of choice

80-98% of IPMNs are surgically resectable
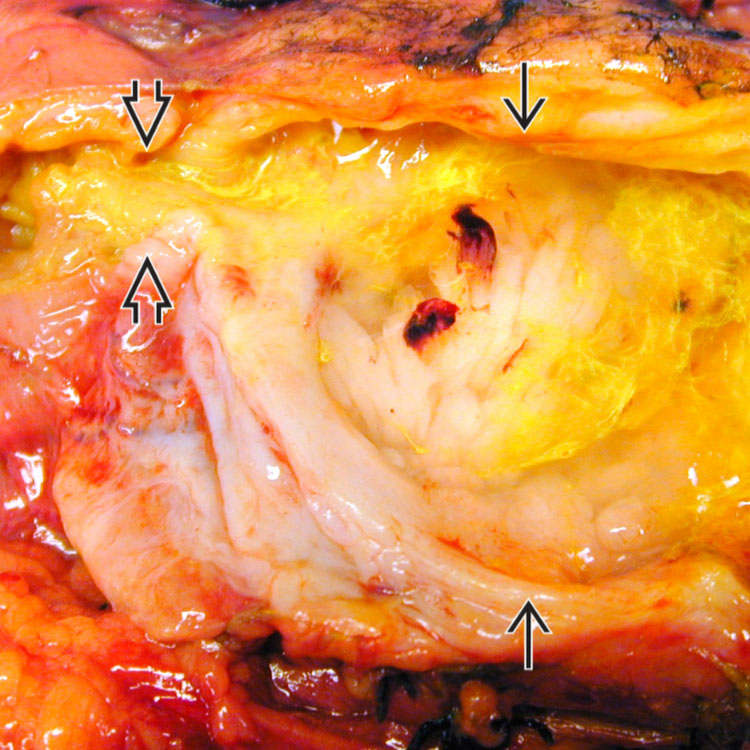
 contains nodular mucosa and abundant mucin (stained with yellow dye). The ampullary orifice is indicated
contains nodular mucosa and abundant mucin (stained with yellow dye). The ampullary orifice is indicated  . A dilated patulous ampulla with extruded mucin is a typical appearance of this tumor on endoscopy.
. A dilated patulous ampulla with extruded mucin is a typical appearance of this tumor on endoscopy.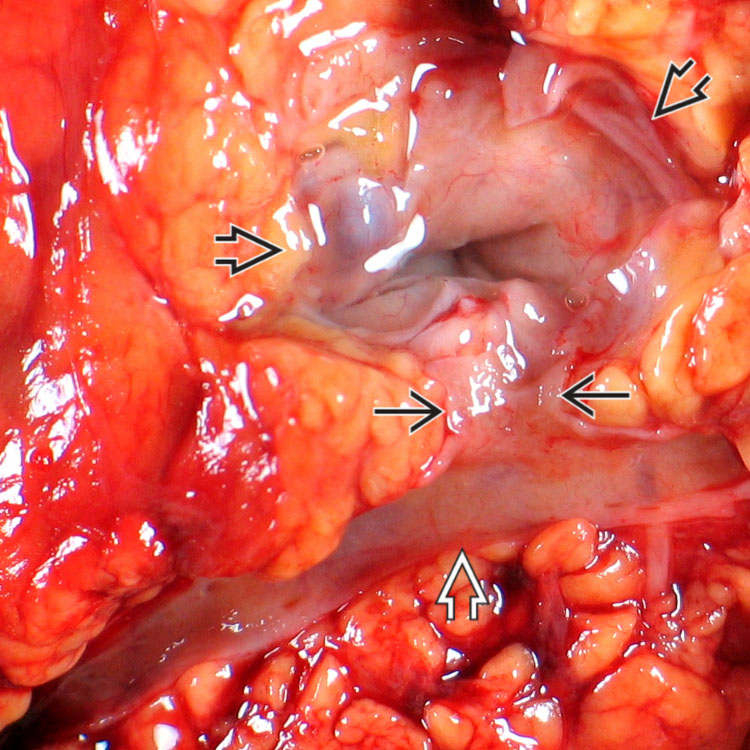
 connected to the main pancreatic duct
connected to the main pancreatic duct  via a dilated branch duct
via a dilated branch duct  .
.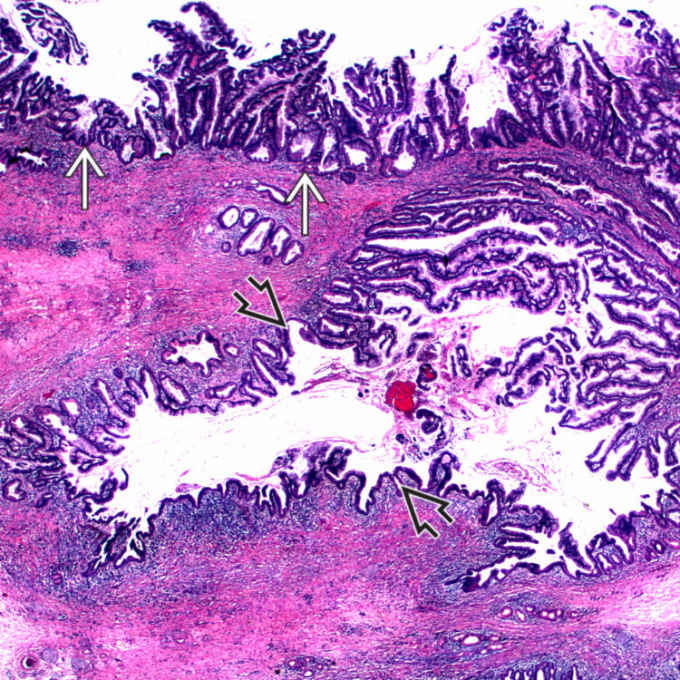
 and a large branch duct
and a large branch duct  . The stroma is dense and fibrotic.
. The stroma is dense and fibrotic.
















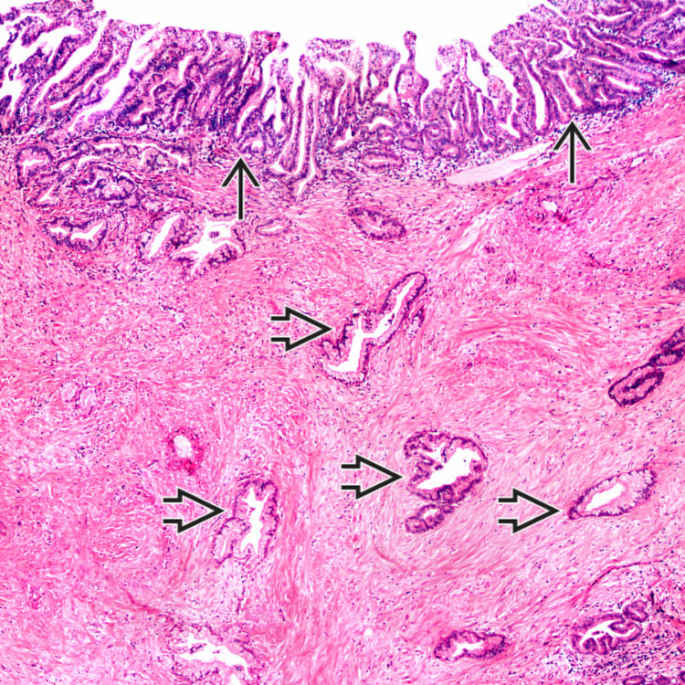
 . The infiltrating neoplastic glands
. The infiltrating neoplastic glands  are of pancreatobiliary type.
are of pancreatobiliary type.










