<
Source: Adapted from Facts about the official “do not use” list of abbreviations. Joint Commission on Accreditation of Healthcare Organizations. Available at: www.jointcommission.org/facts_about_the_official_/. Accessed October 23, 2011.
The ROS is a summary of the pharmacist–patient interview. It is a series of questions focused on a head-to-toe review of the body that may be related to the symptoms described by the patient.10
Objective
The objective section of the SOAP note includes data that can be measured objectively. Information from the physical examination, diagnostics tests, laboratory tests, and computerized medication profiles are considered objective data. Vital signs (blood pressure, heart rate, respiratory rate, and temperature), weight, and height are also included in the objective section. Significant physical exam findings (e.g., decreased S2 or aortic stenosis, crackles in the airways), diagnostic tests or measurements (e.g., oxygen saturation, electrocardiogram, and/or computerized tomography results), and pertinent laboratory measurements (e.g., complete blood count, lipid panel, international normalized ratio, and/or serum drug concentrations) are also recorded in this section. The date and time (if pertinent to assessment) should be included with the objective data.
Usually only pertinent data are included in the objective section. The pertinent data confirm the presence or absence of disease, control of disease, and/or data necessary for assessment of medication use (e.g., drug levels or renal and hepatic function). For example, normal electrolyte laboratory values do not need to be included unless the values are vital to the assessment of a particular problem. In contrast, including a normal blood glucose or A1c reading documents the rationale for the assessment of glycemic control in a patient with diabetes. Inclusion of more than the most recent objective data will depend on whether the information is pertinent to the assessment and plan for that particular patient encounter. For example, reporting more than one blood pressure reading can be essential to assess if blood pressure control has changed. However, inclusion of 6 months’ worth of blood pressure readings is typically excessive.
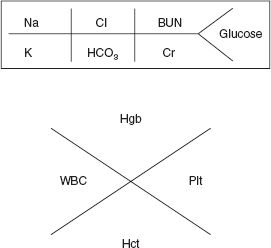
The objective data should not be written in paragraph or phrase format. Rather, it should be a list of objective data that includes the name (or appropriate medical abbreviation) of the objective data, the date, and the value. For laboratory values, units do not always need to be included unless they differ from the usual units (for that particular institution) of if they could be misunderstood without inclusion (e.g., see the consult note example later in this chapter in Box 3.3). Often, a shortcut version for the complete blood count and chemistry panel values is written in SOAP notes (Figure 3.1). Laboratory values may also be placed in a table format. As previously discussed, if the medication list is derived from a computerized medication record, then it is typically included in the objective section. Each medication entry should include the name, strength, route of administration, directions, and frequency of use.
FIGURE 3.1 Shortcut version of common laboratory values.
Abbreviations: BUN, blood urea nitrogen; Cl, chloride; Cr, creatinine; Hgb, hemoglobin; Hct, hematocrit; HCO3, bicarbonate; K, potassium; Na, sodium; Plt, platelets; WBC, white blood cells.
Assessment
The assessment section of the SOAP note summarizes the pharmacist’s evaluation of the collected subjective and objective information. The assessment guides the proposed therapeutic plan for the patient. The pharmacist is responsible for systematically assessing each medication in the current regimen for its appropriateness, efficacy, safety, and adherence.12 The assessment portion of the SOAP note arranges the patient’s identified health- or drug-related problems in order of decreasing priority, documenting the most important or acute problem first. It is also important to consider the reason for pharmacist referral, because this is often the first problem to be addressed with the patient.
Each identified problem, addressed separately, has an accompanying therapy goal that the pharmacist, in collaboration with the patient and referring provider, seeks to achieve. As appropriate, the goals of therapy should follow national or local (e.g., institutional) guidelines and follow the principles of evidence-based medicine. Clearly documenting the goal(s) of therapy allows for continuity of care with progression toward achievement of that goal. In addition to stating the therapeutic goal for each identified problem, the pharmacist classifies each problem’s current status. Terms to use include controlled/uncontrolled, stable/unstable, improved/unimproved, resolved/worsening, or subtherapeutic/supratherapeutic. Of note, some terms are more appropriate for use in follow-up notes rather than in an initial note. Describing the current status of the problem assists in further assessment and development of the plan.
The assessment also includes documentation of an actual or potential etiology of the problem. Consider subjective or objective information, the physiological process of the problem, or psychosocial factors as potential etiologies. Subjective data, such as patient-reported medication nonadherence, impact the status of the problem and need to be included as a potential etiology in the pharmacist’s assessment. Objective evidence, including, but not limited to, laboratory tests, diagnostic exams, self-monitoring results (e.g., home blood pressure or glucose readings), or hospitalizations, may support physiological changes of the identified problem. Psychosocial factors that may impact the identified problem include, but are not limited to, lifestyle choices, cultural influences, education, and financial status. Collectively, a variety of information supports each problem’s assessment and provides the framework for the pharmacist’s plan of action and recommendations.
When assessing problems during a follow-up encounter, consider changes that may have taken place since the previous encounter. This includes any changes in therapy, objective data, and/or psychosocial factors. Clearly documenting changes and including a timeline, if possible, assists in the completeness of an assessment.
Plan
After integrating subjective and objective information with the disease-related and patient-specific factors in the assessment portion, the pharmacist must propose a patient-specific plan for each identified problem. The plan will include a complete and specific documentation of all pharmacological and nonpharmacological recommendations, monitoring, patient education, referrals, and follow-up. In some cases, providing an alternative plan may be appropriate, particularly if a patient is likely to follow up with another healthcare provider.
Pharmacological and nonpharmacological recommendations include continuing, stopping, increasing, or decreasing current therapy and/or beginning a new therapy. This portion of the plan specifies the recommended drug, dose, route of administration, frequency, instructions for use, and duration, if applicable. Documentation of the evidence-based rationale for each change should be provided, because this strengthens the recommendation and may impact its acceptance by prescribers. Of note, in some practice settings, pharmacists may not make medication changes without first discussing it with the patient’s referring prescriber. In these settings, pharmacists should use verbs such as recommend or consider when proposing elements of the plan.
For all recommendations involving drug therapy, identification of appropriate monitoring parameters, including self-monitoring, laboratory tests, and exams/procedures, ensures safety and efficacy. The monitoring plan should include instructions on monitoring indicators and a timeline for such evaluation, which enables the pharmacist, prescriber, and patient to track progress toward the therapeutic goal. Ultimately, future patient encounters, assessments, and plans will be based on the monitoring of the previous plans/recommendations.
Patient education includes everything from drug information (use, side effects, interactions, etc.) to self-monitoring instructions, disease state or lifestyle information, goal setting, and medication adherence. The pharmacist must document patient-specific instructions and include a statement regarding the patient’s understanding of provided education/instruction and overall agreement with the plan.
The plan should also contain specific information on patient follow-up and referrals. It is important to include and provide the patient with information on when, where, with whom, and what is to be assessed during follow-up. Documentation for a referral includes who the patient is to see and the reason for the referral.
Although the assessment and plan sections are often written separately as two different sections, some pharmacists prefer to combine the sections under each identified problem. Nonetheless, the assessment and plan sections are the crux of written documentation for the patient encounter. They are the main points to communicate with the patient and referring prescriber. In addition, other healthcare professionals (e.g., nurses) will review these sections and may incorporate their recommendations into the delivery of patient care.
Types of SOAP Notes
Although a full SOAP note provides the most comprehensive information about a patient encounter, abbreviated SOAP notes are appropriate in some settings or certain types of encounters. Full SOAP notes are comprehensive patient notes and include all of the elements discussed previously, including an assessment and plan for all problems (see Box 3.1). This type of note is most often used for an initial visit.
For follow-up visits, an abbreviated SOAP note is often used to avoid repeating information already documented in the patient chart (see Box 3.2). For example, in the outpatient setting, an abbreviated note may only include any new, relevant, subjective information from the patient; recent laboratory or diagnostic test results; and changes in medications and/or adherence. A new assessment and plan, even if the plan includes continuing a previous plan, should always be documented. An abbreviated SOAP note is also used in the inpatient setting to update the patient’s status on days following admission. The most important components included in abbreviated SOAP notes are the CC and/or reason for follow-up, the HPI (if it differs from last encounter), an updated medication list, any new or updated objective information (e.g., vital signs, laboratory values), and the updated assessment and plan. All other subjective and objective components (e.g., PMH, FH) only need to be included if relevant to the follow-up encounter or if they have changed since the initial encounter.7
BOX 3.1 An Appropriately Composed Full SOAP Note
SUBJECTIVE
CC: “I’m here for my appointment regarding my blood pressure.”
HPI: JG, a 59 yo female, presents for an initial pharmacist hypertension management appointment. Pt reports “feeling fine” today. Shares that she was diagnosed with hypertension 8 years ago after a hospitalization for a “blood pressure emergency.” Pt brings BP medication bottles (lisinopril, chlorthalidone, amlodipine, and metoprolol succinate) to appointment. Confirms taking the above BP medications this morning; however, reports missing 3 days of medication over the past week since she rushed out of the house to get the bus to work. Denies checking BP at home. Pt shares that smoking “keeps her calm,” and she is not interested in quitting at this time. Reports rinsing mouth after using fluticasone/salmeterol 2 times a day. States last used albuterol 1 week ago after spending the afternoon gardening. Denies nighttime asthma symptoms.
PMH: Hypertension × 8 years; asthma; lower back pain
SH: (+) smoking since 25 yo (~5 cigarettes per day); (−) alcohol; (−) illicit drugs; (+) exercise (90 minutes aerobic exercise per week); well-balanced diet that includes lean meats, vegetables, fiber, fruits, and dairy products; works part-time as an office administrator; divorced; lives with boyfriend. Insurance: self-pay.
Allergies: NKDA
Medications:
lisinopril 20 mg 1 tablet PO daily
amlodipine 10 mg 1 tablet PO daily
chlorthalidone 25 mg 1 tablet PO daily
metoprolol succinate 25 mg 1 tablet PO daily
fluticasone/salmeterol diskus 250 mcg/50 mcg 1 puff BID
albuterol MDI 1 puff Q4H prn
Nature Made multivitamin 1 tablet PO daily
Denies use of CAM.
Immunizations: influenza (last October), pneumococcal (at age 52), Tdap (6 years ago)
OBJECTIVE
Vitals (today): BP 166/96; HR 70 bpm; Wt: 91 kg; Ht: 5 ft 3 in
Labs (3/5/12): All within normal limits, except K1 (3.3 mEq/L); CrCl 98 mL/min
Diagnostic tests: PFTs (pending receipt from primary care doctor)
ROS:
Appearance: Well-groomed, well-nourished, well-developed
Chest: CTAB
Cardio: RRR
ASSESSMENT
1. Hypertension: BP today is not controlled to goal of <140/90 per JNC 7 guidelines. All BP medications filled within the last 30 days. Elevated BP likely due to medication nonadherence, as pt missing 3 days of medication this week and likely also in previous weeks. Pt is a current smoker, which will cause BP elevations.
2. Tobacco use: Pt currently smoking ~5 cigarettes per day. Goal is smoking cessation. Pt in precontemplation stage and not ready to quit smoking at this time.
3. Asthma: Symptoms controlled with appropriate adherence to and use of maintenance inhaler. Goals are to control asthma symptoms (no nighttime symptoms), prevent asthma exacerbations, and infrequent use of albuterol inhaler per ERP-3 guidelines; pt meeting goals.
PLAN
1. Hypertension: Pt agreed to begin using pillbox and decided that keeping it near the refrigerator will help her remember to take the medications with breakfast. Assisted pt in filling pillbox. Follow up PharmD appt in 4 weeks for BP check.
2. Tobacco use: Encouraged smoking cessation. Will assess patient’s readiness to quit and provide ongoing education on the benefits of smoking cessation at next appointment.
3. Asthma: Encouraged continued adherence to maintenance inhaler. Educated patient on rinsing mouth with water and spitting out after each dose to avoid thrush. Recommend continuing current therapy. Will reassess as needed.

Julie Miller, PharmD
4/8/12
SUBJECTIVE
CC: “I’m here for my follow-up appointment.”
HPI: JG, a 59 yo HF, presents for her pharmacist hypertension management follow-up appointment. Pt shares that she only forgot her BP medications 1 time since her last appt. Shares that if in a rush, she will take her pillbox with her and take her medications when she gets to work. Brings her pillbox with her today. Pt offers that she’s thinking more about quitting smoking before she turns 60.
Allergies: NKDA
Medications:
lisinopril 20 mg 1 tablet PO daily
amlodipine 10 mg 1 tablet PO daily
chlorthalidone 25 mg 1 tablet PO daily
metoprolol succinate 25 mg 1 tablet PO daily
fluticasone/salmeterol 250 mcg/50 mcg 1 puff BID
albuterol MDI 1 puff Q4H prn
Nature Made multivitamin 1 tablet PO daily
Denies use of CAM.
OBJECTIVE
Vitals (today): BP 134/82; HR 66 bpm; Wt: 91 kg; Ht: 5 ft 3 in
Labs (3/5/12): WNL, except K+ is low at 3.3 mEq/L; CrCl 98 mL/min
Immunizations: up to date
ROS: unremarkable
ASSESSMENT/PLAN
1. Hypertension: BP today is 134/82, which has decreased from BP reading (166/96) taken 4 weeks ago. BP today is controlled to goal of <140/90 per JNC 7 guidelines. Improvement in BP due to improved medication adherence. Pillbox appropriately filled. Encouraged ongoing BP medication adherence. Recommend continuing current therapy. Follow-up PharmD appt in 4 weeks for BP check.
2. Tobacco use: Pt currently smoking ~5 cigarettes per day. Goal is smoking cessation. Pt thinking about quitting. Encouraged smoking cessation. Educated pt on benefits of smoking cessation. Counseled pt on available NRT options; pt did not have any questions. Pt thankful for information but wants to continue thinking about quitting. Will assess readiness to quit at follow-up.

Julie Miller, PharmD
5/2/12