58 Wounds
A wound can be thought of as any break in the integrity of the skin (Enoch and Leaper, 2005), although when this is due to minor trauma it might be termed a cut or an abrasion. Such wounds tend to heal fairly quickly by the process of regeneration of tissue and cells and generally do not pose any long-term problems. However, the time it takes for a wound to heal will depend on a number of factors related to the nature of the wound, the individual and environment. Many of these factors will be dealt with at different points throughout this chapter.
Structure of the skin
The functions of the skin and factors that affect skin condition are listed in Table 58.1. How these roles link to wounds and wound healing will be explored in more detail later.
Table 58.1 Functions of the skin and factors affecting skin condition
| Functions of the skin | Factors affecting skin condition |
|---|---|
| Protective covering | Dryness |
| Moisture retention | Age |
| Sensation | Environment |
| Regulation of body temperature | Nutrition |
| Release of waste | Hydration |
| Absorption of nutrients, that is Vitamin D |
Wound healing
In adults, a scar is the normal end product of most injuries, with occasionally excessive scarring, that is hypertrophic or keloid complicating matters. However, wound healing can also be scarless, such as in fetal skin or the oral mucosa (Desai, 1997a; Wysocki, 2007). This type of healing presents an interesting concept and may offer some significant developments in the future. There are also many individuals for whom healing is delayed, and includes wounds often referred to as ‘chronic’ or ‘non-healing’. Other terminology is used in clinical practice to describe how wounds heal and includes:
Essentially, healing by primary intention (Fig. 58.1) describes where the wound edges are opposed, that is brought together by sutures, staples or glue and wound healing occurs mainly by connective tissue formation. Delayed primary healing is used where there may be a risk of contamination or infection, that is if the patient has undergone emergency abdominal surgery. In this instance, some of the layers of tissue are stitched, and the sutures are placed in readiness for the remainder of the wound to be closed after 48 h when the risk of infection is less. In contrast, secondary healing (Fig. 58.2) describes a situation where the wound is left open to heal by the normal processes. This type of healing is relevant to many of the types of wounds that will be discussed later.
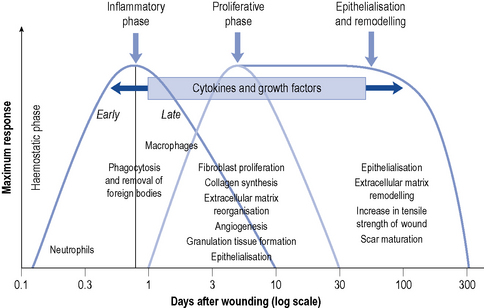
Any injury to the skin will result in a sequence of events aimed at repairing the defect. Figure 58.3 shows the process of wound healing and is divided into four phases:
These signs are normal and should not be considered as indicating the presence of infection.
The presence of a functional blood vessel network is fundamental for wound healing to progress. Angiogenesis, the formation of blood vessels, is required to supply oxygen to the wound environment and it is through the migration of capillaries through the provisional matrix that the vasculature is re-established. Endothelial cells migrate and proliferate to eventually join the existing blood supply to the injured area. Once this has occurred, granulation tissue can form to begin to repair the defect. The provisional tissue laid down (Fig. 58.2) is made up of fibrin, fibronectin, collagen and glycosaminoglycans. Through the action of fibroblasts, collagen is produced and the continued presence of macrophages ensures the wound is kept ‘clean’. Collagen production is essential for healing to progress and in particular Types I, III and IV are required.
Around the same time, it may also be possible to see signs of epithelialisation occurring (Fig. 58.2). Keratinocytes, the cell associated with this process, are initiated hours after injury; they migrate from the edge of a wound over the provisional matrix laid down or they dissect through it. Hair follicles can act as islands of regenerating epithelium in some areas. The wound bed can be easily damaged during the proliferative phase, with simple things like incorrect dressing choice causing significant damage. Moist wound healing (MWH) principles (Winter, 1962) are encouraged to support the normal physiological process of healing.
Factors affecting wound healing
Generally, wound healing should progress as described above; however, a number of factors that affect healing have been identified (Grey and Harding, 2008). A summary of these is provided in Table 58.2, some of which include:
Table 58.2 Intrinsic and extrinsic factors affecting wound healing
| Intrinsic factors systemic local | Extrinsic factors | |
|---|---|---|
| Age | Blood supply | Nutrition |
| Uraemia | Changes in oxygen tension | Smoking |
| Jaundice | Vessel trauma | Radiotherapy |
| Diabetes | Abnormal scarring | Infection |
| Anaemia | Haematoma | Drugs |
| Hormones | Local infection | Iatrogenic influences |
| Malignant disease | Wound dressings | |
Age
Younger patients appear to have an increased rate of healing, and there are differences in fetal healing that mean the regeneration process is superior with little or no inflammation or scarring (Desai, 1997b). In comparison, wound repair in the elderly is slower (Ashcroft et al., 2002), and management may be more challenging because of concurrent disease processes. This is a particular problem in the proliferative and remodelling phases where tissue appears to be more friable and fragile. The overall effects of age on wound healing appear to be:
Diabetes
Diabetes poses many problems for patients with wounds and management is often challenging because of concurrent peripheral neuropathy (PN), peripheral arterial disease (PAD), neuro-ischaemia and infection (Table 58.3).
Table 58.3 Complications of diabetes
| Peripheral neuropathy | Causes damage to nerves that leads to a lack of the protective pain sensation, but the blood supply remains good. Very common and can lead to foot deformities and abnormal walking patterns. Neuropathy should be considered in terms of sensory, autonomic and motor changes. The foot is usually warm, numb and dry with palpable foot pulses |
| Peripheral arterial disease | Often develops as a result of atherosclerosis but develops at a faster rate in diabetic patients. Can affect the large (macro) and small (micro) vessels leading to decreased blood flow to the legs and feet, which can ultimately lead to minor or major amputations. The foot is often cool, clammy with absent or reduced foot pulses |
| Neuro-ischaemia | A combination of peripheral neuropathy and peripheral arterial disease |
| Infection | More common in diabetic patients, probably because they have an associated defective immunity. The neutrophil and lymphocyte response is slow (partly due to vascular problems); therefore, the inflammatory and subsequent phases are impaired. Hence, these patients have an increased tendency to develop infections |
Infection
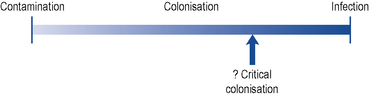
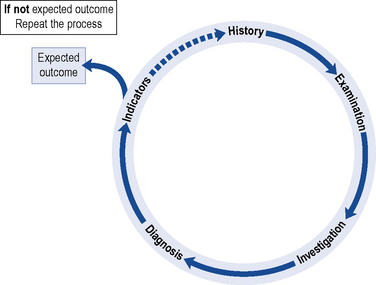
Bacterial invasion of wounds is very common. In fact, any break in the skin integrity places the wound at risk of local contamination or infection and if untreated can lead to systemic infection. The spectrum of infection from colonisation through to infection is demonstrated in Fig. 58.4. The difficulty may be in recognising when such circumstances are present. The normal inflammatory signs were discussed earlier, and these should be borne in mind when examining a patient’s wound. However, there are additional local signs that may be present in wounds healing by primary or secondary intention (Fig. 58.5) that suggest an infective process; these include:
In recent years, there has been increased recognition that bacteria have the ability to build up colonies that present a challenge in terms of the management of bacterial load. Known as biofilms, they have the ability to resist removal and have been implicated in delayed healing of a number of wound types. The removal of dead and devitalised tissue from the wound bed seems to have some effect in preventing the growth of biofilms (Wolcott and Rhoads, 2008); however, this method is not suitable for all wounds; hence, other approaches are being sought.
Nutrition
The nutritional requirements for wound healing have been the subject of debate with limited evidence as to the exact dietary components for individual wound types. In general, if the patient has a balanced diet, this should be sufficient for the normal processes to take place. However, a diet that is lacking in vital nutrients can lead to delayed wound healing and wound breakdown. In the extreme, the patient can become malnourished with surgical patients most at risk of protein energy malnutrition (PEM). Box 58.1 outlines the nutritional factors that should be considered in the assessment of individuals, many of which have been incorporated in nutritional risk assessment tools. Individuals at most risk of nutritional deficiencies are those affected by:
Box 58.1 Nutritional assessment and treatment options
Specialist nutritional assessment
Anthropometric measurements such as:
Body Mass Index (BMI), % weight loss, haemoglobin, skin fold thickness, grip strength, serum albumin
Smoking
Smoking is known to be detrimental to health generally, and in addition the effect of nicotine and carbon monoxide on skin and muscles is well documented (Møller et al., 2002). These substances reduce the oxygen levels in the tissues and can lead to the formation of thrombi. A good blood supply and adequate vascularisation is important for normal wound healing. There has been debate about the period of time patients should abstain from smoking to reduce relevant, potential complications. This has been suggested to vary from 4 (Sorensen et al., 2003) to 8 weeks (Møller et al., 2002). However, the role of nicotine replacement interventions in further reducing complications is less clear.
Drugs
There are certain drugs that are suggested to have an effect on the healing process. These include NSAIDs, corticosteroids and immunosuppressive agents (Grey and Harding, 2008), which affect the inflammatory response, collagen synthesis and mitosis, respectively. Whilst drugs do not generally cause wounds, there have been recent reports that nicorandil, used for the treatment of angina, may cause peri-anal wounds that resolve on cessation of the medication (Baker et al., 2007).
Diabetic foot ulcers
Epidemiology
It was estimated that there were 1.4 million people diagnosed as diabetic in 2002 with these figures expected to double by 2010 (Cradock and Shaw, 2002). The cost of treating individuals with diabetes accounts for at least 9% of the acute healthcare costs in the UK. These costs, however, do not take into account the personal cost to the individual, such as a reduction in the ability to work and time they may need to take off work (Waters and Holloway, 2009). Diabetic foot problems are the most common cause for admission, and patients admitted to hospital for in-patient care are often hospitalised for 4–6 weeks, which obviously increases the financial costs considerably.
One of the major risks to patients with diabetic foot disease is that of amputation, which could be minor, that is mid-foot to toe; or major, that is mid-foot and above. National Service Frameworks for diabetes (Department of Health, 2001) have emerged to address this and, in turn, have been built upon (Department of Health, 2007a,b). Of concern is that up to 85% of amputations are preceded by foot ulcers. Therefore, if the incidence of foot ulcers can be reduced, this might lead to a reduction in amputations.
Aetiology
Individuals with diabetes are at risk of a number of systemic complications (see Chapter 44).
The two main causes of foot ulceration in patients with diabetes are:
PN causes damage to the nerves that leads to a lack of the protective pain sensation and is present in 75% of patients with diabetes. In this group of individuals, the blood supply to the extremities remains good, but the foot becomes insensate and can subsequently become deformed. This leads to an abnormal walking pattern and potentially tissue breakdown from abnormal pressures placed upon the foot. The characteristics of the diabetic foot are set out in Table 58.4. Unfortunately, the early systemic changes associated with the onset of diabetes may be present for up to 12 years before a diagnosis is made, by which time damage has already begun to occur and is often irreversible.
Table 58.4 Clinical features of a diabetic foot with neuropathy or arterial disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree