FIGURE 13-1 Initial rhythm recorded on the external defibrillator by the emergency squad. Coarse ventricular fibrillation is demonstrated on the ECG strip, which was converted to sinus rhythm by an external 200J shock.
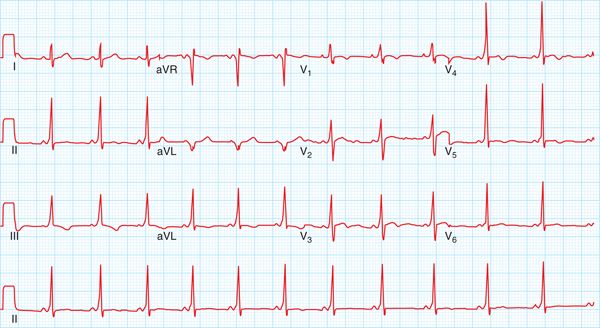
FIGURE 13-2 The12-lead ECG recorded in the emergency department. The WPW pattern is clearly seen on the ECG. The positive delta wave in lead V1 and negative delta wave in lead aVL are indicative of a left lateral accessory pathway location.
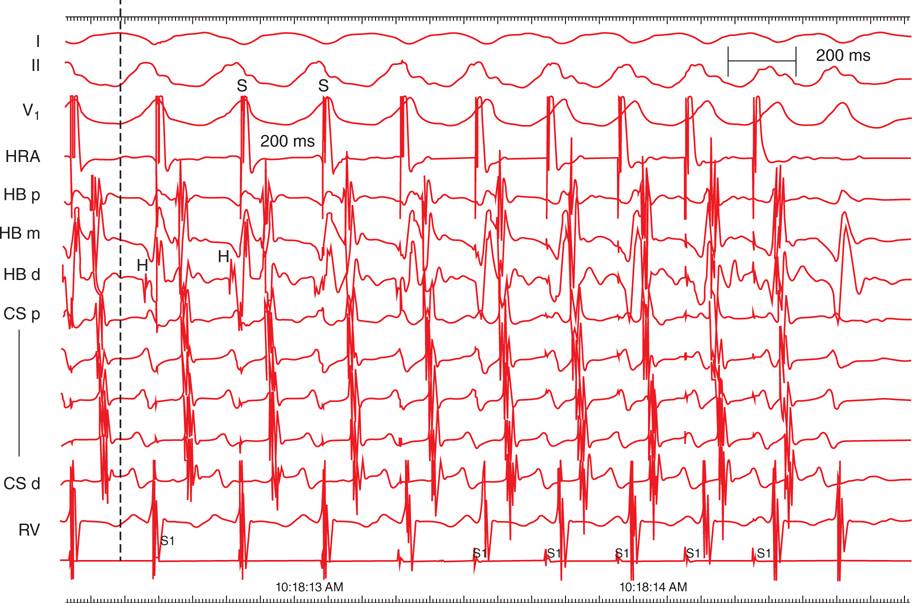
FIGURE 13-3 Tracings from the electrophysiologic study during atrial pacing with an infusion of isoproterenol at 8 μg/min. Shown are recordings from surface leads I, II, and V1 and intracardiac recordings from the high right atrium (HRA), His bundle proximal, mid, and distal locations (HB p, HB m, and HB d), coronary sinus proximal to distal locations (CS p to CS d), and right ventricular apex (RV). Atrial pacing stimuli (S) are delivered throughout the tracing at a cycle length of 200 ms (300 bpm). A His bundle recording (H) is detected at the beginning of the tracing indicating that initially there was conduction down both the normal AV conduction system and accessory pathway. The HV interval measured from the onset of the first complete QRS complex (dotted line) is –70 ms. There is 1:1 conduction from the atrium to the ventricle across the accessory pathway at 300 bpm during the isoproterenol infusion. This confirms that this is a high-risk accessory pathway and can account for the episode of aborted sudden death.
EPIDEMIOLOGY
The prevalence of the Wolff-Parkinson-White (WPW) ECG pattern, which indicates the presence of an accessory pathway causing ventricular preexcitation, is estimated to be on the order of 0.1% to 0.3%.1,2
Although there is a clear association between the presence of ventricular preexcitation and sudden cardiac death (SCD), the overall risk of sudden death in this patient population is relatively small.
The incidence of SCD in asymptomatic patients with a WPW ECG pattern is low and estimated to be <0.5% per patient-year.3
However, the prevalence of aborted SCD in large series of patients with WPW syndrome referred to an electrophysiology center for treatment of symptomatic arrhythmias is on the order of 1% to 2%, and in approximately 50% of these patients the aborted SCD event was their first arrhythmia symptom.4,5
ETIOLOGY AND PATHOPHYSIOLOGY
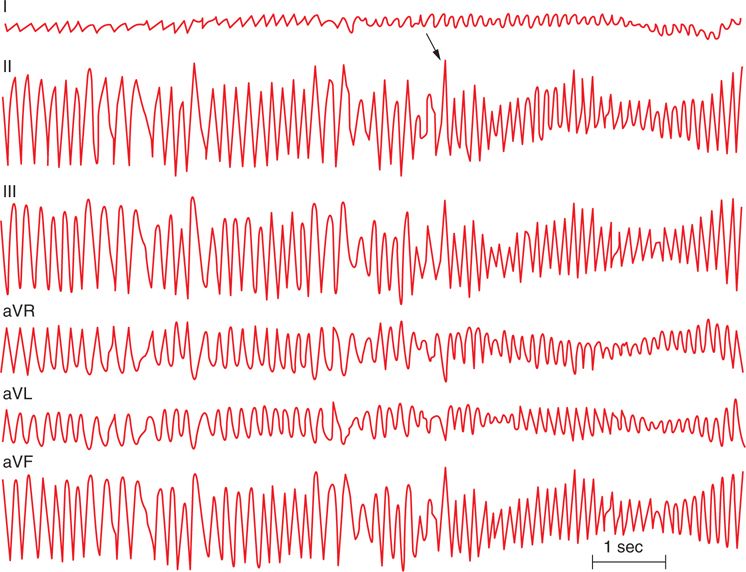
The mechanism of SCD in WPW patients is most often due to the presence of atrial fibrillation, which conducts rapidly across an accessory pathway and triggers ventricular fibrillation (Figure 13-4).
FIGURE 13-4 Atrial fibrillation degenerating to ventricular fibrillation. The initial portion of the image shows atrial fibrillation conducting across and accessory pathway at rates of over 300 bpm. The arrow points to where the rhythm degenerates to ventricular fibrillation.
In the majority of patients with an accessory pathway, the occurrence of atrial fibrillation is triggered by an episode of paroxysmal supraventricular tachycardia (PSVT) due to AV reentrant tachycardia.
Like patients without WPW, patients with WPW can have atrial fibrillation triggered for reasons other than an episode of PSVT. Regardless of the cause of atrial fibrillation, as long as there is rapid conduction across the accessory pathway, the arrhythmia can degenerate into ventricular fibrillation and result in a cardiac arrest.
A number of clinical predictors for the occurrence of SCD in patients with WPW have been described and include male gender, young age, older age, septal accessory pathway location, left lateral accessory pathway location, presence of multiple accessory pathways, history of syncope, and the presence of symptomatic tachycardia. These clinical predictors are very weak and nonspecific, and due to the small numbers of patients in most series the studies often have conflicting data.4,5
Patients with baseline intermittent preexcitation on their ECG or telemetry monitors are felt to be at low risk for SCD since this generally indicates that their accessory pathway cannot conduct at rapid rates.
The use of noninvasive testing with stress testing and pharmacologic agents has been advocated for risk stratification of patients with persistent WPW pattern on their ECG. Patients with abrupt
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree