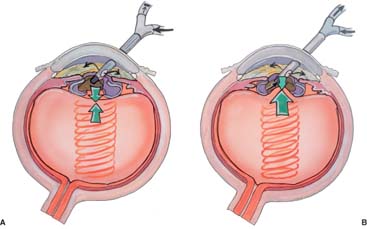
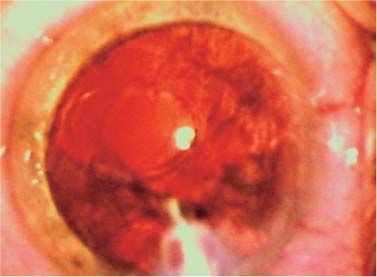
Chapter 19 Vitreous loss during phacoemulsification is a vexing and frustrating complication. Of those problems associated with cataract surgery it is the most distressing. The management of related intraoperative problems is best known and understood. The postoperative sequelae are commonly known. All surgeons perform cataract surgery employing methods to prevent vitreous loss from ever occurring. Nevertheless, despite our vastly improved technical expertise, our sophisticated equipment, and our heightened awareness that vitreous loss can strike at any moment, it continues to haunt us on a regular basis. Depending on the patient population, the instance of posterior capsule vitreous loss is reported to vary from 0.8 to 1.25%.1–4 Young patients with soft cataracts and strong capsules typically have a lower rate. Elderly patients, especially those who present with very dense cataracts, have a higher rate. With age and increasing cataract density come increasingly fragile capsules and zonules. The gel-like consistency of the vitreous is due to the arrangement of long, thin, nonbranching collagen fibrils suspended in a network of glycosaminoglycan (GAG) chains. The major contributing molecular component of vitreous is a complex of GAG and hyaluronan (hyaluronic acid; HA).5 This arrangement of small-diameter fibrils, widely separated by highly hydrated GAG/HA chains, permits the transmission of light to the retina with a minimum of scattering. The vitreous base is a three-dimensional zone. The vitreous body is densely adherent 1.5 to 2 mm anterior to the ora serrata and from 1 to 3 mm posterior depending on age. It also extends several millimeters into the vitreous body itself. Disturbance of this region may lead to rhegmatogenous retinal breaks. The vitreous also has a papillary adherence to the optic nerve. It is loosely adherent to the macula forming the vitreomacular complex. Vitreous fibrils appear to be continuous and unbroken from the anterior peripheral vitreous to the posterior vitreous. Significant traction on the anterior vitreous fibrils may eventually cause posterior traction.6 Vitreous loss can lead to complications including cystoid macular edema and retinal detachment. These complications can be reduced by minimizing the amount of trauma inflicted on an eye at the time of vitreous loss and during vitrectomy. Therefore, our understanding of the pathophysiology of vitreous loss, and its correction, is a necessary focus to minimize trauma to the posterior segment. The first point to remember is that vitreous is supposed to be in the posterior segment! So, unless we have good cause, there is no reason to remove it. When vitreous escapes from its natural habitat it can wreak havoc, so we must chase it down and direct it back to its home. It is not necessary to invade its home turf and continue to seek its extinction as we might some aggressive weed. Containment is the key to atraumatic vitreous surgery; obliteration is unnecessarily aggressive and will lead to problems. Naturally, the best strategy for containing the vitreous is to keep it behind the posterior capsule by preventing vitreous loss in the first place. Assuming that this is ultimately impossible in some cases, the next best strategy is to minimize the potential vitreous lost following capsule rupture. Phacoemulsification is performed, for all practical purposes, in a closed system. There are two incisions, each one approximately the correct size for the instruments being used. There is a small amount of fluid leakage at each of these incisions, but not a lot. Fluid comes into the eye by means of a gravitational feed from the infusion bottle. Flow from the bottle continues until the intraocular pressure equals the gravitational pressure in the bottle. At this point, all flow stops. When the phacoemulsification system aspirates fluid and material from the eye, the intraocular pressure lowers. A passive flow of fluid from the irrigation bottle begins to restore the original pressure. If the irrigation and the aspiration levels are approximately equal, a constant-state intraocular pressure will be maintained. The constant-state intraocular pressure reduces the possibility of vitreous coming forward. Theoretically, if the posterior capsule opens, the positive pressure in the anterior chamber will hold the vitreous back. The vitreous can come forward only if the aspiration system continues attracting vitreous up, into the anterior chamber, or if the aspiration reduces the intraocular pressure faster than the irrigation can restore it. In the absence of an adequate anterior chamber intraocular pressure, the vitreous will move forward. If aspiration is stopped when the posterior capsule opens, the intraocular pressure in the anterior chamber will remain stable and equal to the infusion pressure. This will hold the vitreous back, preventing vitreous loss (Fig. 19–1). Although the above description is the ideal situation, it is frequently unobtainable because the posterior capsule opens invisibly. The capsular tear may be hidden behind the nucleus, or some fluffy cortex, and cannot be seen until further material has been removed, exposing the rent in the capsule. Cortical strands or capsular folds that may have a similar linear appearance to a tear may mask a tear in the capsule when one develops. However, if aspiration is terminated immediately after identification of the capsular tear, the amount of vitreous that can come forward is significantly restricted. This is due to maintenance of the closed chamber. All of the incisions are plugged with instruments! Vitreous can go no further than the anterior chamber. There is no way for it to escape from the eye. The potential for massive vitreous loss is essentially nonexistent (Fig. 19–2). FIGURE 19–1 (A) When the posterior capsule opens, the pressure in the anterior chamber holds the vitreous back, preventing vitreous prolapse. (B) Vitreous can come forward only if the pressure in the anterior chamber is low, as when aspiration continues. (Note dark arrow on aspiration line indicating continued aspiration and phacoemulsification.) Frequently, however, the opening in the posterior capsule cannot be recognized because cataract material blocks the surgeon’s view. Continued aspiration permits vitreous to move forward and into the anterior chamber. Next, when an opening in the posterior capsule is recognized, the phaco tip should not be removed from the eye. The machine should be continued in position 1, irrigation. This maintains a positive pressure in the anterior chamber and restricts vitreous movement. Without aspiration, vitreous cannot be aspirated from its usual location. The second instrument should be removed from the eye and replaced immediately with a viscoelastic cannula tip. The anterior chamber is then generously filled with viscoelastic. This will hold the vitreous back. The phacoemulsification tip can thereupon be removed from the eye. The viscoelastic maintains a powerful anterior chamber pressure that prevents escape of the vitreous through the rent and its tendency to follow the phaco tip out of the eye (see Chapter 29, Fig. 29–3). The posterior capsule is also of assistance to restrain vitreous movement. Vitreous can come forward only through the breach in the capsule. Therefore, a small opening will permit less vitreous prolapse than a large opening. The capsule is essentially a diaphragm within which is a defect, a site for vitreous transit. If the eye is not pressurized prior to the removal of the phaco tip, anterior chamber and intraocular pressure will drop, and increased amounts of vitreous will come forward. In addition, the violent passage of vitreous through the rent can extend it. This permits the remaining vitreous to pass more easily and may destabilize the remaining capsular support for later intraocular lens fixation.
VITRECTOMY FOLLOWING
VITREOUS LOSS
ANATOMY
BASIC PRINCIPLES
THE INFUSION/ASPIRATION BALANCE
CAPSULAR TEARS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree