FIGURE 19-1A A 12-lead electrocardiogram (25 mm/sec) depicting ventricular bigeminy with an inferior axis and LBBB morphology premature ventricular contractions (PVCs). Notice a QS morphology in lead V1 with notching on the downward deflection with precordial early transition in lead V3 that suggests PVCs originating in the commissure between the left and right aortic cusps.
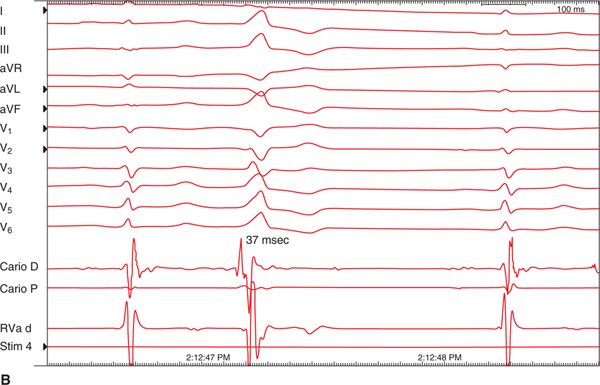
FIGURE 19-1B Activation mapping of the same patient using a bipolar catheter. Notice intracardiac electrograms revealing the earliest activation (ie, 37 msec) preceding the QRS complex (PVC) at the commissure between the right and the left aortic cusp.
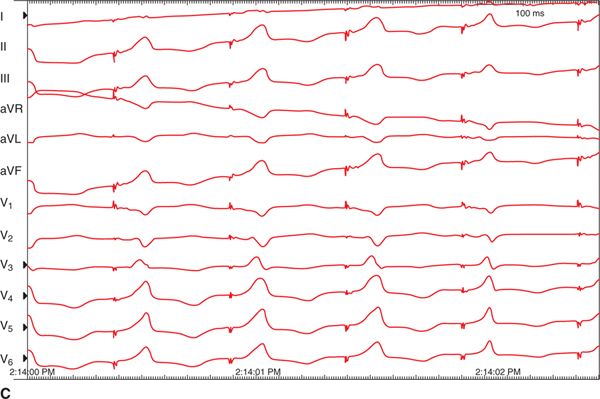
FIGURE 19-1C Pace-mapping demonstrating identical PVC morphology at the commissure between the right and the left aortic cusp.
EPIDEMIOLOGY
Ventricular tachycardia (VT) originating from the left ventricular outflow track (LVOT) particularly from the aortic cusp is part of the large family of the so-called “idiopathic ventricular arrhythmias” (IVT), which occur mostly in structurally normal hearts. Aortic cusp VT is rare, given that RVOT VT accounts for almost 80% to 85% of IVTs, whereas it accounts for only 30% of LVOT VTs.1 It has no gender preference; it might occur at any age and mostly on exertion given its catecholamine-induced nature, but it can also occur at rest. Although, thought to have a benign course, patients with frequent premature ventricular contractions (PVCs) or episodes of VT might develop tachycardia-induced cardiomyopathy and sudden cardiac death. The first case series reporting, patients with VT arising from the aortic sinus of Valsalva was published in 2001. This included 12 patients with LBBB and inferior axis VT with characteristic ECG findings with previously failed ablation, all of whom were successfully ablated from the aortic root.2
ANATOMY OF THE AORTIC ROOT
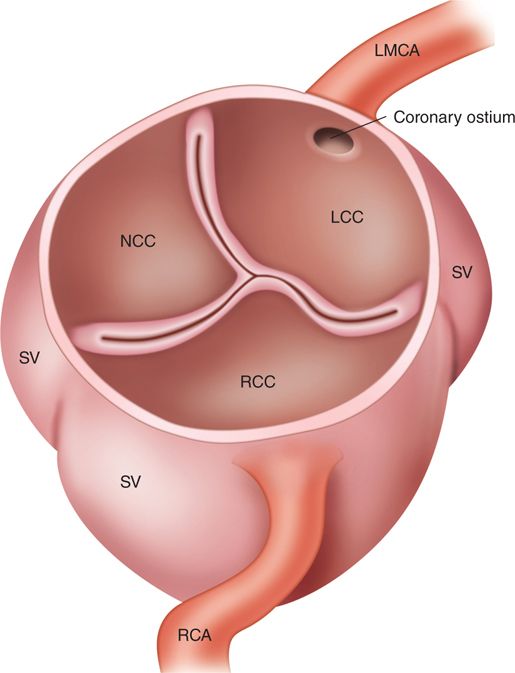
The aortic valve is the “heart” of the heart. Almost every single structure is directly related to this valve including all four chambers and the rest of the cardiac valves. Its area is approximately 3 to 4 cm2. Generally, it has three leaflets attached to the aortic annulus but in 1% to 2% of the population the aortic valve might be unicuspid, bicuspid, or quadricuspid. Right above these semilunar (crescent-shape) leaflets are the Valsalva sinuses (VS), which are small dilatation of the ascending aorta. Two of them (ie, left and right) give rise to the left main coronary artery (LMCA) and right coronary artery (RCA) from their superior aspects. They are mainly made up of connective tissue with some muscular bundles from the ventricle. The coronary ostia diameters are 2 to 5 mm for RCA and 4 to 7 mm for LMCA.
The aortic root is an anterior cardiac structure, but it is anatomically posterior and somewhat rightward related to the RVOT. The left aortic sinus is in close contact with left atrium, pulmonary artery, and aortomitral continuity. The right sinus is posterior to the RVOT and close proximity to the tricuspid valve, and the noncoronary sinus is anterior to the lower portion of the interatrial septum, which is of critical importance when performing transseptal punctures (Figure 19-2).
FIGURE 19-2 Aortic root with a transverse section at the level of the sinotubular junction depicting each of the three aortic sinuses of Valsalva (SV), the left coronary cusp (LCC), the right coronary cusp (RCC), and the noncoronary cusp (NCC). The left main coronary artery (LMCA) and the right coronary artery (RCA) are also noted.
ETIOLOGY AND PHYSIOPATHOLOGY
The origin of this type of VT is mostly located at the bottom of any of the sinuses of Valsalva, most commonly from the left followed by the right and rarely from the noncoronary cusps (NCC). Pathology reports have shown that this arrhythmia arises from sleeves of myocardium in the cusps, which are most likely extensions of ventricular muscle into the base of the aortic cusps.3 The lack of muscular tissue in the NCC renders it without a substrate for arrhythmia formation. Another hypothesis is that in patients with idiopathic dilated cardiomyopathy the basal left ventricular scar may extend into to the aortic sinus of Valsalva, providing the substrate for aortic cusp VT.4
Accumulating evidence has suggested that this arrhythmia is related to cAMP-mediated triggered activity with an increase of intracellular calcium, which causes early or delayed after-depolarizations. Consequently, similarly to RVOT VT and other forms of LVOT VT, aortic cusp VT is sensitive to substances (ie, adenosine, acetylcholine, β-blockers) that directly interact with adenylyl cyclase by inhibiting the production of cAMP through G proteins.5 Likewise, verapamil might also terminate this arrhythmia by direct blocking of calcium receptors and in turn diminishing the available calcium to the sarcoplasmic reticulum.
DIAGNOSIS
Clinical Presentation
• Broad spectrum from monomorphic premature ventricular contractions (PVCs) to repetitive nonsustained VT (NSVT) or paroxysmal sustained monomorphic VT (SMVT).
• Programmed stimulation during EPS can induce and terminate it, especially in patients presenting with SMVT.
Diagnostic Tests
• ECG at rest, signal average electrocardiogram (SAECG), and microvolt T-wave alternans (TWA) are usually unremarkable.
• Exercise testing might induce VT in the vast majority of patients who present with SMVT but only a small percentage of patients with NSVT or PVCs.6
• Based on its mechanism of action (ie, cAMP-triggered activity), this arrhythmia can be initiated and terminated by programmed stimulation with either atrial or ventricular rapid pacing during EPS, sometimes requiring isoproterenol infusion.
• Entrainment is not feasible due to lack of a reentry loop.
• Adenosine, verapamil, and vasovagal maneuvers usually terminate this arrhythmia.
• For those patients presenting with frequent PVCs, 24-hour Holter monitoring should be considered to assess PVC burden.
Electrocardiography
The 12-lead ECG during episodes of VT is of paramount importance since it might narrow the differential diagnosis and guide the approach of VT ablation. Specific ECG patterns have been recognized in order to localize the exact place where the studied VT is originating. The PVC/VT usually has a LBBB morphology and inferior axis (positive deflection in inferior leads). The main and most helpful criterion to differentiate among the large variety of VT coming from the “ventricular outlet track” is the QRS transition zone in the precordial leads, in which QRS complex becomes positive. The basic approach is as follows:
• The more anterior the VT source is, the later the transition in the precordial leads is going to be (ie, leads V4-V5).
• Conversely, the more posterior the structure, the earlier the transition zone will be (ie, V1-V2).
• Consequently, RVOT-VT and LVOT-VT usually have transition zones in V4-V5 and V1-V2, respectively. There are more specific criteria in order to further localize each arrhythmia in each outlet track.
RVOT
• Transition zone V3 or later + QRS duration <140 msec favors the septum.
• Transition zone V4 or later + QRS >140 msec favors the free wall.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree