Vena Cava Resection during Hepatectomy
Aijun Li Mengchao Wu
DEFINITION
Hepatic neoplasms involving the inferior vena cava (IVC) have usually been considered unresectable because of the high surgical risk of massive bleeding and air embolism. However, aggressive surgical approaches for hepatic tumors involving the IVC have recently been reported to have been performed safely and have been shown to alter the natural history of the disease.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28
DIFFERENTIAL DIAGNOSIS
Intrahepatic cholangiocarcinoma(ICC)29
Hepatocellular carcinoma (HCC)
Renal cell carcinoma
Metastatic disease
MEDICAL HISTORY AND PHYSICAL EXAM
By far, the most frequent indication for IVC resection en bloc with hepatectomy is HCC. As cirrhosis is the major risk for HCC and also the major risk factor for postoperative liver failure, great attention must be paid to history, symptoms, and signs associated with underlying liver disease. In general, hepatectomy that also requires IVC resection is only performed in patients without intrinsic liver disease.
History
Hepatitis
Alcohol consumption
Symptoms
Fatigue
Encephalopathy
Rapid weight gain
Signs
Ascites
Asterixis
Abdominal or thoracic telangiectasia
Cachexia
Morbid obesity (steatohepatitis)
Extensive pedal edema (IVC compression)
A thorough evaluation of potential pulmonary and cardiovascular disease must be performed. Patients with significant comorbidities are not candidates for major hepatectomy with en bloc IVC resection.
IMAGING AND OTHER LABORATORY STUDIES
Ultrasonography (US). US is often the initial diagnostic imaging modality employed but is inadequate to fully evaluate hepatic lesions and IVC involvement.
Contrast-enhanced computed tomography (CT). In addition to providing information regarding the number, size, and location of lesions, CT is an effective tool to estimate the remnant liver volume (RLV).
Magnetic resonance imaging (MRI) examination. MRI is valuable for characterizing lesions and defining vasculature. It is particularly helpful in diagnosing the extent of tumor thrombus (TT) within the IVC. Magnetic resonance angiography (MRA) is useful for identifying the major hepatic veins and the IVC and clarifying their relations to any tumor masses.
Each of these modalities may reveal IVC compression or TT within IVC.
Patients that are suspected of having malignant invasion of the IVC wall on preoperative radiologic studies should also have echocardiography to assess for extension into the right heart. Such extension is not prohibitive of resection but mandates an operative approach that provides access to the chest, thus increasing morbidity while hope for a surgical cure is fleeting.
In addition to routine laboratories, all patients must undergo a careful preoperative assessment of liver function and potential underlying disease.
Liver function tests
Hepatitis serologies
Coagulation studies
Platelet count
SURGICAL MANAGEMENT
Preoperative Planning
Preoperative ipsilateral portal vein embolization to create hypertrophy of the planned liver remnant may prevent postoperative hepatic failure after extended major hepatectomy.
Low-volume resuscitation minimizes blood loss but exaggerates potential hemodynamic instability with clamping of the IVC.
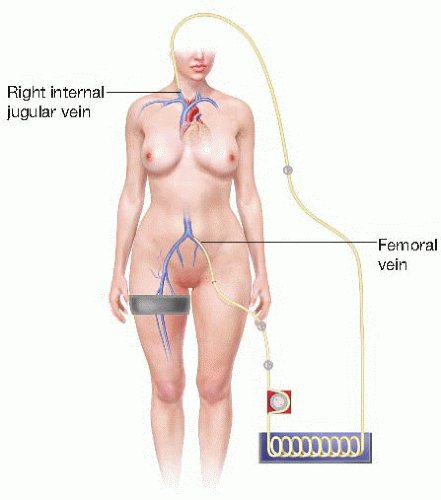
Venovenous bypass (VVB) with total hepatic vascular exclusion (THVE) facilitates resection of primary and metastatic hepatic neoplasms that invade the vena cava.21,22 Given the prior pearl, be prepared to use VVB when IVC invasion is suspected (FIG 1). Preoperative communication and coordination with perfusion and anesthesia teammates is vital to success in this regard.
Anatomic Considerations
Characteristics of the posterior hepatic IVC. The posterior hepatic IVC extends from the renal veins to the confluence of the right atrium (RA). This is further divided anatomically into the inner segment of the pericardium (intrapericardial IVC), the suprahepatic IVC below the diaphragm, the retrohepatic IVC, and the lower segment of the subhepatic renal vein. The IVC is thick-walled, tenacious, elastic, and not particularly susceptible to invasion. The hepatic veins are thin-walled but rapidly develop thicker walls as they insert into the IVC. Thus, the proximal portions of the hepatic veins are at greatest risk for injury during the operation.
Such injury invariably results in intraoperative hemorrhage and/or air embolism.
Characteristics of tumors that involve the IVC. Most liver cancers near the IVC originate from hepatic segments 1, 4, 5, and/or 8, or in the paracaval portion of the caudate (referred to by some as segment 9).
Caudate tumors: Anatomically, the hepatic caudate lobe is divided into the left hepatic caudate lobe (Spigelian lobe, caudate lobe proper, segment 1) and right hepatic caudate lobe (dorsal sector). The right hepatic caudate lobe can be further divided into the paracaval portion (segment 9) and the caudate process (segment 10).23, 24, 25, 26 Caudal tumors may either extend anteriorly and thus invade the portal vein and/or the bile duct, resulting in obstructive jaundice, or extend posteriorly and thus invade the IVC. Generally, about one-fourth of caudate tumors involve the IVC.27,28
Tumors arising near the root of the hepatic veins: These tumors typically compress the anterior IVC between the mid and right hepatic veins or between the mid and left hepatic veins. Because the hepatic veins have no valves, are thin-walled, and fixed in the hepatic parenchyma, they are unable to retract upon injury and air embolism is liable to occur. To avoid air embolism and massive hemorrhage, the operative strategy should plan to isolate the hepatic veins extrahepatically and occlude them in advance.17, 18, 19 The risk in resecting tumors that are near the confluence of the hepatic veins with the IVC is not rupturing the IVC but injuring the thin wall of the hepatic veins.
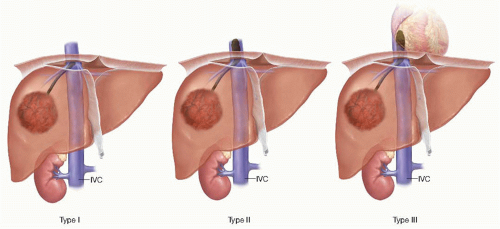
Characteristics of inferior vena cava tumor thrombus (IVCTT): IVCTT often spreads from the hepatic veins or hepatic short veins.30, 31, 32, 33 IVCTT is clinically classified into three types (FIG 2): (1) the posterior liver type (type I), where TT is located in the IVC behind the liver and below the surface of the diaphragm; (2) the superior liver type (type II), where TT extends into the IVC above the surface of the diaphragm but outside the atrium; and (3) the intracardiac type, where TT surpasses the surface of the diaphragm and enters the RA. The operative plan for patients with IVCTT completely depends on this classification of the IVCTT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree