Vena Cava Filter Placement
John E. Rectenwald
Venkataramu N. Krishnamurthy
Introduction
Venous thromboembolic disease occurs in an estimated 400,000 to 600,000 U.S. residents each year, resulting in 50,000 to 200,000 deaths. Although treatment with anticoagulation remains the mainstay of therapy, clinical situations arise when anticoagulation is contraindicated or inadequate. In these instances, vena cava filters are used to prevent pulmonary embolism (PE).
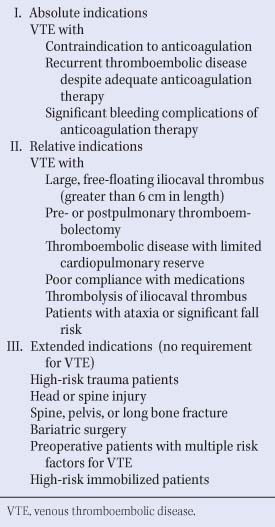
The primary reason for placement of an inferior vena cava (IVC) filter is for the prevention of a potentially fatal PE. Table 1 shows the absolute, relative, and expanded indications for vena cava filter placement. Patients with absolute and relative indications have existing thromboembolic disease with a contraindication to anticoagulation or a complication or failure of anticoagulation. Those with extended indications are typically those without overt thromboembolic disease, but are considered to be high risk for deep vein thrombosis (DVT) and possess a relative contraindication to anticoagulation. In this group of patients, it is particularly important that the potential risks and benefits be assessed on an individual basis. Further, it is important to remember that placement of a vena cava filter does nothing to treat or prevent development of further DVT or subsequent
postthrombotic syndrome. These patients should still be anticoagulated at the earliest opportunity for treatment of their DVT or PE when safe to do so.
postthrombotic syndrome. These patients should still be anticoagulated at the earliest opportunity for treatment of their DVT or PE when safe to do so.
Table 1 Indications for Vena Cava Filter Placement | |
|---|---|
|
Types of Available Vena Cava Filters
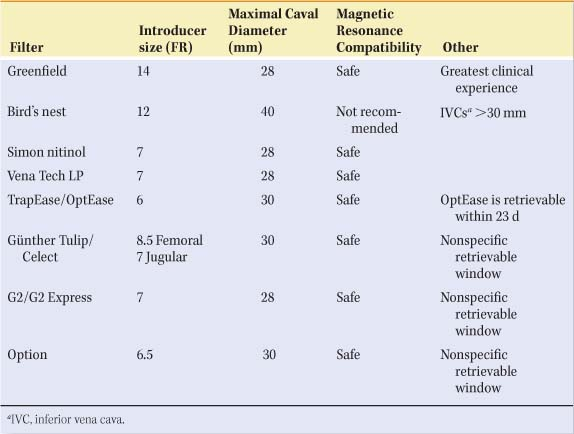
The first widely used inferior cava filter, introduced in 1972, was the stainless-steel Greenfield filter. The original 24 French device consisted of a cone of six stainless-steel wires terminating in tethering hooks that anchored the device in the IVC. This design allowed two-thirds filling of the filter cone with only a 50% reduction of the filter’s cross-sectional area, thereby allowing blood flow around the thrombus and the fibrinolytic system to lyse the clot. It was initially inserted by venotomy, with the first percutaneous placement reported in 1984. Since then, the Greenfield filter has been improved and several generations of additional vena cava filters have been developed, culminating in the current trend toward development of retrievable filters. The characteristics of an ideal filter are listed in Table 2. However, at present no ideal filter exists. Each of the currently available IVC filters has their advantages and disadvantages. Table 3 depicts some of the features of available filters in use today including profile, maximum caval diameter, magnetic resonance compatibility, and retrieval window.
Table 2 Characteristics of an Ideal Vena Cava Filter | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Preprocedure Evaluation
After determining that a patient is an appropriate candidate and has the appropriate indications for a vena cava filter, pre-operative preparation includes physical examination to determine potential access sites, as well as venous duplex of bilateral lower extremity veins to assess for DVT. The right common femoral vein is the preferred access site as it presents a straighter course to the infrarenal IVC with minimized potential filter tilt; however, in the presence of a right-sided iliofemoral DVT, an alternate side would be chosen, typically the left common femoral vein or the right internal jugular vein. Routine laboratory analyses are obtained with particular attention to the patient’s coagulation status and creatinine level. There are very few contraindications to vena cava filter placement (Table 4). Special situations requiring thoughtful placement of IVC filters include pediatric and pregnant patients, multiple uncertain effects, as well as the durability of IVC filters. These patients may benefit from placement of retrievable filters if filter placement cannot be avoided.
Table 3 Characteristics of Available Vena Cava Filters | |
|---|---|
|
Table 4 Contraindications to Inferior Vena Cava Filter Placement | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Inferior Vena Cava Filter Placement Technique
The common femoral vein is localized fluoroscopically using the femoral head as a landmark. The groin is then anesthetized. Percutaneous cannulation of the right common femoral vein is then performed and a wire (Bentson wire or J-wire) is advanced into the IVC under continuous fluoroscopic visualization. A short 5 French sheath is advanced into the common femoral vein using Seldinger’s technique. An iliocavagram is performed with a marker pigtail catheter to rule out iliac and vena cava thrombus and anomalous venous anatomy, to determine the diameter of the infrarenal IVC, and to define the location of the renal veins (Fig. 1). Additionally, the length between the iliac bifurcation and the renal veins is noted. If there is any ambiguity about the location of the renal veins on venacavagram, the renal veins may be selected with a C2 Cobra catheter and selectively injected (Fig. 2). Most available filters are 60 mm in length or shorter, except the bird’s nest filter, which is 80 mm long. Distal IVC thrombus necessitates jugular access. Caval diameter less than 28 mm is acceptable for any of the filters in use today. The Günther Tulip/Celect, the TrapEase/OptEase, and the Option filters can be used in IVC diameters up to 30 mm. The bird’s nest filter may be used in “megacavas” with diameters up to 40 mm. For an IVC diameter more than 40 mm (or >30 mm to avoid a bird’s nest filter), one may consider placement of bilateral common iliac vein filters or placement of a suprarenal IVC filter if the suprarenal cava diameter is of an appropriate diameter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree