FIGURE 46-1 Summary of the most common forms of neurally mediated reflex syncope. In each case the basis of the faint may be “vasodepressor” or “cardioinhibitory” or both (“mixed”).
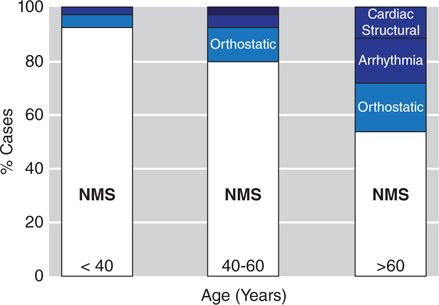
Neural reflex faints (particularly the vasovagal faint) not only comprise the vast majority of syncope events in younger, otherwise healthy patients but also remain a major contributing cause of syncope in older individuals (Figure 46-2).3,4 However, due to a higher prevalence of heart and vascular disease in older individuals, establishing the diagnosis may be difficult. In any case, no matter the patient’s age, it is the “reflex” nature of the faint, most often detected by the patient’s symptoms documented during a carefully obtained medical history, that most effectively distinguishes neural-reflex faints from other causes of collapse.
FIGURE 46-2 Bar graph depicting approximate frequency of various causes of syncope by age. Note that neurally mediated syncope (NMS, white) remains a common cause in all age groups. Orthostatic syncope increases with advancing age (light blue). (Modified with permission from Parry SW, Tan MP: An approach to the evaluation and management of syncope in adults, BMJ 2010 Feb 27;340(7744): 468-473.)
NOMENCLATURE
In neurally mediated reflex syncope, systemic hypotension with consequent cerebral hypoperfusion may be caused by either vasodilation or severe bradycardia acting alone, or as is more often the case, both working together.1 When vasodilatation is the primary cause of symptomatic hypotension, the faint is termed “vasodepressor” and is the result of some degree of diminished arterial resistance, but an even greater component of increased venous capacitance (particularly in the splanchnic bed) with consequent diminished venous return to the heart. If bradycardia is the principal cause of hypotension, then the faint is termed “cardioinhibitory,” and is due to the occurrence of a predominantly vagally-mediated slow heart rate (often prolonged asystolic pauses [Figure 46-3]) of sufficient severity to compromise cardiac output and cerebral blood flow. Most often both mechanisms are present, and the pathophysiology of the syncope is said to be “mixed.”1,2
FIGURE 46-3 Sinus arrest suggestive of a cardioinhibitory syncope in a young patient with typical vasovagal symptoms. However, it should be recognized that a vasodepressor mechanism may also be present but cannot be confirmed in the absence of documenting the presence of hypotension during cardiac pacing to overcome the bradycardia.
Given the pathophysiology described above, “vasodepressor” syncope is best considered a subset of the vasovagal reaction in which systemic hypotension is primarily due to vaso- and venodilatation; in the vasodepressor faint, cardioinhibition is either nonexistent or modest. The physiology of the “vasodepressor” faint was investigated in the classic study by Weissler et al in 1957.5 These investigators pointed out that muscarinic blockade and correction of bradycardia (by atropine) had little impact on susceptibility to syncope. Thus a “vasodepressor” faint should be considered a physiologic unique entity (albeit often found in a “mixed” form with a cardioinhibitory feature) and should not be simply employed as another term for vasovagal syncope or “neural reflex faint.” However, and rather unfortunately, the term “vasodepressor” often continues to be misused; this erroneous usage is confusing and should be abandoned.
CLINICAL EVALUATION
Initially, the medical history of the patient described here was interpreted to suggest that this patient was experiencing both “immediate” and subsequently the more classic “delayed” form of orthostatic hypotension. However, her age and absence of evident triggers (eg, drugs, neurologic disease) made orthostatic syncope unlikely. Furthermore, her symptom complex (ie, palpitations, sweating, feeling cold, pallor, and later, fatigue) were more compatible with a neurally mediated reflex vasovagal reaction triggered by abrupt movement to upright posture. Consequently, an autonomic study using noninvasive ECG and hemodynamic monitoring (Finometer, Finapres Medical Systems, Arnhem, The Netherlands) was undertaken. In brief, after a 10-minute period of being quietly seated in a chair, “active” standing resulted in evidence for immediate orthostatic hypotension (Figure 46-4A). The test was repeated in both the drug-free state and after sublingual nitroglycerin (0.4 mg) pretreatment; both resulted in her experiencing typical symptoms of “dizziness” and brief visual disturbance associated with an immediate but transient fall of systemic blood pressure but without substantial bradycardia. The observation strongly favored a predominantly “vasodepressor” response. The patient indicated that the sequence of events was typical of her spontaneous attacks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree