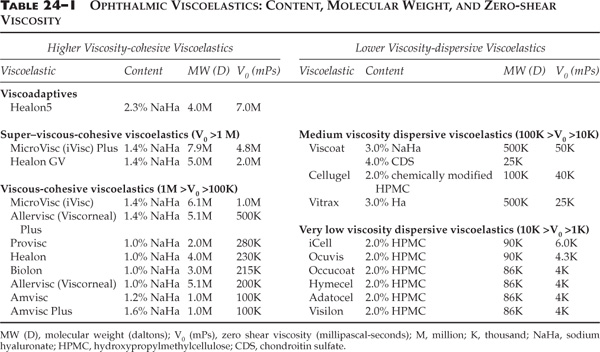
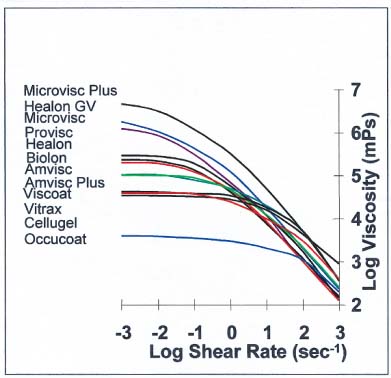
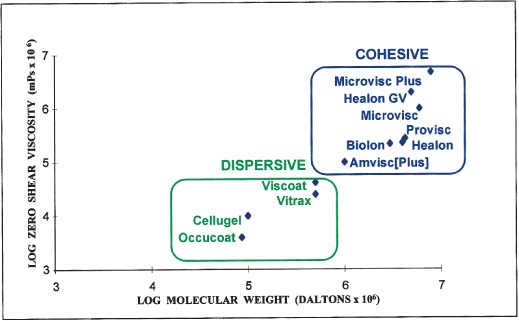
Chapter 24 Two distinct methodologies for the use of ophthalmic viscosurgical devices (OVDs)1 (viscoelastics) in dealing with problems in cataract surgery have been developed recently. They both considerably enhance our ability to manage previously difficult cases. These are the dispersive-cohesive viscoelastic soft shell technique, and a new viscoadaptive OVD, Healon5. This chapter discusses these two viscoelastic strategies sequentially. It is the author’s belief that presenting the strategies in this way gives the reader a clearer understanding of how to approach specific problems that are likely to occur in the operating room. The soft shell technique was developed prior to the advent of Healon5. Because Healon5 use represents a new and different viscoelastic technique, the discussion in the soft shell section below refers to viscoelastics prior to Healon5. The Healon5 section, which follows the soft shell discussion, outlines methods for management of similar problems with HealonTable 24–1). Each possesses different chemical and physical rheologic properties.2 The question of which is the best viscoelastic for cataract surgery has led the author to investigate those rheologic properties that are most important in anterior segment surgery. In this investigation no general consensus on the ideal viscoelastic has emerged. This is confirmed by the essentially unchanged market share distribution of vastly different viscoelastics over the past decade. The lack of consensus among surgeons on what viscoelastic properties are best suggests that different viscoelastic properties may be useful to ophthalmic surgeons in different surgical situations. Therefore, rather than looking for the “best” viscoelastic, it might be best to analyze their different properties in an effort to develop a new surgical approach that uses both cohesive and dispersive viscoelastics sequentially to avoid mixing them. Thus, the surgeon fully takes advantage of the positive attributes of each type of viscoelastic while minimizing drawbacks. A viscoelastic preparation intended for intraocular use must be an isotonic, pH balanced, aqueous solution. The acceptable range of physical properties is governed by the molecular nature, chain length, and concentration of the rheologically active polymer constituent. In an effort to devise criteria for a surgically useful classification system, it is essential to identify the rheologic parameters that best apply to the viscoelastic in relationship to its behavior in surgery. Currently the two most useful parameters for such a classification are (1) zero-shear viscosity (V0), and (2) cohesive or dispersive behavior (relative degree of cohesion).3,4 Zero-shear viscosity correlates with both the molecular weight of the rheologically active viscoelastic component and its concentration. It can be used to establish a ranking of ophthalmic viscoelastics for the purpose of classification (Table 24–1 and Fig. 24–1). Long-chain ophthalmic visco-elastic molecules tend to entangle in solution, causing them to aggregate. They are therefore referred to as cohesive. As zero-shear viscosity declines below 100,000 mPs (millipascal-seconds), molecular chain entanglement becomes a far less significant factor. (The unit mPas was previously centipoise or cps, where 1 mPas = 1 cps, the dynamic viscosity of water.) Consequently, less viscous viscoelastics tend to be easily broken up, and are accordingly referred to as dispersive. Because cohesion of all currently marketed viscoelastics correlates with zero shear viscosity, as well as with the molecular weight of the rheologically active constituent (but not in a simple, linear relationship), the degree of cohesion falls neatly into the same classification with zero shear viscosity, above (Fig. 24–2). Future viscoelastics may be manufactured with viscosity and cohesion somewhat dissociated from each other, especially if a rheologic component other than hyaluronic acid is used as the basic constituent. Then these parameters may not correlate as well. Therefore, one of these parameters alone is insufficient for classification. FIGURE 24–1 Pseudoplasticity curves of common commercial ophthalmic viscoelastics. Pseudoplasticity curves of common commercial ophthalmic viscosurgical devices (OVDs) are usually plotted as shown here with log dynamic viscosity (millipascal-seconds) vs. log shear rate (seconds 1). The zero-shear or stationary viscosity is the level at the far left of each curve, and is indicative of the ability of the OVD to maintain space when stationary. The viscosity level in the mid–shear rate ranges (100 to 101) represents the resistance offered by the OVD to the normal rate of movement of surgical instruments through the eye during surgery. The viscosity at high rates of shear (about 103) is indicative of the resistance offered by the OVD to flow through a small cannula. Different laboratories tend to report these data with significant variation. It is therefore wise to consider differences of less than 10% in any given point as equivalent. The surgical tasks for which ophthalmic viscoelastics are utilized are generally facilitated by higher zero-shear viscosity. Highly viscous OVDs tend invariably to be more cohesive (less dispersive). However, in certain situations dispersive rather than cohesive behavior may be desirable (e.g., to retain a thick layer of viscoelastic adjacent to the corneal endothelium to protect it from the trauma of phaco or irrigation). In such circumstances it is often better to accept lower viscosity to gain greater dispersion, rather than the reverse. It is helpful, therefore, when considering surgical use, to classify ophthalmic viscoelastics based on zero-shear viscosity as well as the cohesive or dispersive nature. All current OVDs in this category possess, as their active rheologic agent, various concentrations and chain lengths of non–cross-linked long-chain hyaluronic acid. In addition all have zero-shear dynamic viscosities greater than 100,000 mPas. Super–viscous-cohesive viscoelastics, a subcategory including MicroVisc Plus (iVisc Plus in Canada) and Healon GV, have zero-shear viscosities exceeding 1,000,000 mPas. Viscous-cohesive viscoelastics, including, among others, MicroVisc, Allervisc Plus (Viscorneal Plus), ProVisc, Healon, Biolon, Allervisc (Viscorneal), Amvisc, and Amvisc Plus (Table 24–1) possess zero-shear viscosities between 100,000 and 1,000,000 mPas. Clinical trials have shown that the members of each of these subcategories share similar physical properties, behave in a similar fashion intraoperatively, and lead to comparable surgical results. However, the super–viscous-cohesive viscoelastics appear to have an advantage over the regular viscous-cohesive viscoelastics in facilitating surgical maneuvers, ease of removal, and endothelial protection.5–8 FIGURE 24–2 Cohesive and dispersive viscoelastics. Relative cohesion of ophthalmic OVDs correlates with zero shear viscosity and molecular weight. When OVDs are plotted on a graph where log zero shear viscosity is on the ordinate and log molecular weight on the abscissa, cohesive and dispersive viscoelastics cluster in their respective groups. Zero-shear viscosity correlates well with elasticity.9 Highly viscous-cohesive OVDs are the best for creating space with their viscosity, and preserving it by their elasticity. Elasticity allows the OVD to contract and expand in the presence of an ocular pulse or externally applied force, without being expelled from the eye. These OVDs can displace and stabilize tissues in the surgical environment. Balanced intraocular pressure (i.e., the maintenance of a deep anterior chamber after the creation of the cataract incision), is best accomplished with an elastic and viscous substance. Only the highly viscous-cohesive elastic OVDs are capable of neutralizing posterior positive pressure. I have referred to this OVD-induced pressure-neutral situation as “pressure equalized cataract surgery.” As a result, the higher viscosity-cohesive OVDs are best used in problem cases to create space and stability where it is otherwise inadequate. This benefit can be recognized during surgery when topical anesthesia is utilized. There is often shallowing of the anterior chamber during capsulorrhexis. This is due to the tone of the nonparalyzed extraocular muscles. CCC is enhanced by using viscoelastic to pressurize the anterior chamber equal to that of the posterior pressure. The effect of flattening the anterior convexity of the cataractous lens is to reduce the vector force compelling the tear to extend toward the equator. A round CCC of the appropriate size is therefore more easily accomplished in a pressure equalized environment. A corollary of this principle pertains to the management of a tear that begins to extend toward the periphery. External sources of excessive posterior pressure such as a tight lid speculum or drapes should be alleviated after injection of a superviscous cohesive OVD to flatten the cataractous lens surface, and the CCC should be completed as described in Chapter 5.
USING VISCOELASTICS TO MANAGE
PROBLEMS IN CATARACT SURGERY*
CLASSIFICATION OF OPHTHALMIC VISCOELASTICS
HIGHER VISCOSITY-COHESIVE VISCOELASTICS
Advantages (Table 24–2)
Higher Viscosity-cohesive To create and stabilize spaces | Lower Viscosity-dispersive To selectively isolate and partition spaces |
To deepen the anterior chamber in hyperopic eyes to insert phaco | To protect corneas with Fuchs’ endothelial dystrophy |
To stabilize a difficult capsulorrhexis | To isolate a piece of frayed iris from aspiration by the phaco tip |
To enlarge small pupils | To isolate an area of disinserted zonules |
To dissect adhesions | To isolate vitreous behind a small hole in the posterior capsule |
To implant foldable intraocular lenses | To partition the anterior chamber |
Other uses include expanding a shallow anterior chamber in hyperopia, facilitating the insertion of the phacoemulsification tip where there is positive posterior pressure or a flaccid iris, enlarging a small pupil, dissecting iris-lens capsule adhesions, and assisting during the implantation of foldable intraocular lenses (IOLs) so that the haptic of the lens cannot catch on a fold in the posterior capsule, resulting in a torn capsule (Table 24–2).
Disadvantages
The high cohesion of viscous-cohesive and super–viscous-cohesive OVDs results in ease of removal by irrigation and aspiration at the end of the surgical procedure. However, the same cohesive behavior results in cohesive OVDs being rapidly washed out of the anterior chamber during phaco. Although an invisible thin layer of hyaluronate bound to endothelial cell membrane specific binding sites remains behind,10 there may be insufficient protection of corneal endothelium. Furthermore, cohesive viscoelastics are unable to partition fluid spaces within the anterior chamber (AC). It is therefore impossible, using a cohesive viscoelastic, to sequester an OVD-coated and protected structure in the AC, while working on the other side of the AC with the irrigation and aspiration (I&A) tip, without aspirating the OVD and the structure that should have been sequestered (vitreous, frayed iris, etc.) during phaco or I&A.
LOWER-VISCOSITY DISPERSIVE VISCOELASTICS
Lower-viscosity dispersive viscoelastics include all current OVDs with zero-shear viscosities of less than 100,000 mPs (to date all dispersives marketed have zero shear viscosities less than 50,000 mPs). In these viscoelastics, molecular chain entanglement is less prevalent. Cohesion tends to be significantly weaker, resulting in a tendency for the OVD to disperse when injected into the anterior chamber.
There are two subgroups. The first, the medium viscosity dispersive viscoelastics, possess zero-shear viscosities between 10,000 and 100,000 mPas. They include Viscoat, Cellugel, and Vitrax. The second, the very low viscosity dispersive viscoelastics, consisting of all the unmodified hydroxypropyl methylcelluloses, includes iCell, Ocuvis, Ocucoat, Adatocel, Hymecel, Visilon, Celoftal, and many others (Table 24–1).
Advantages (Table 24–2)
Surgically, the most useful properties of dispersive viscoelastics are their resistance to aspiration and their ability to partition spaces. A dispersive nature, negative electrical charge, and the presence of hyaluronic acid to bind to specific endothelial-binding sites are the three factors that have been demonstrated by Poyer et al11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree