Undifferentiated (Anaplastic) Carcinoma
Lester D. R. Thompson, MD
Key Facts
Terminology
Highly aggressive malignancy of undifferentiated cells
Etiology/Pathogenesis
Preexisting benign or malignant thyroid disease in nearly all cases, with transformation of preexisting carcinoma
Clinical Issues
Majority > 65 years, present with rapidly enlarging neck mass
Grave overall prognosis: > 95% die from disease even with multimodality therapy
Macroscopic Features
Fleshy to firm mass, typically completely replacing thyroid parenchyma, ˜ 6 cm
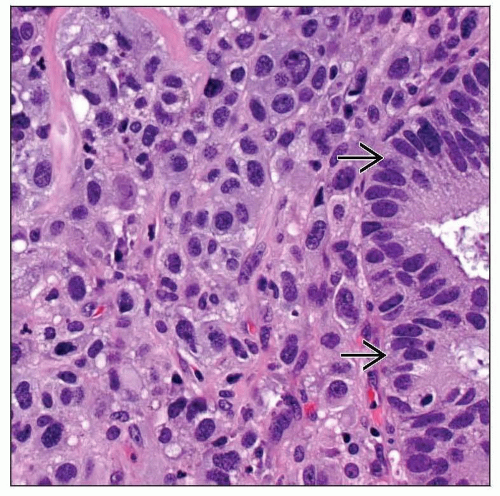
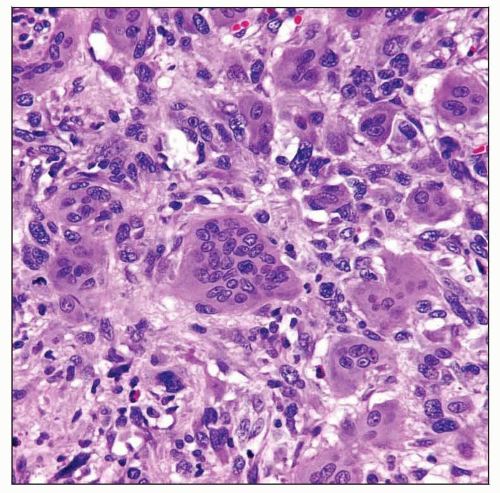
Microscopic Pathology
Extrathyroidal extension, lymph-vascular invasion
Significant necrosis and hemorrhage
Variety of patterns: Sheet-like, storiform, fascicular, angiomatoid, meningothelial
Poorly differentiated cells, polygonal, pleomorphic, spindle, giant, epithelioid, squamoid
Profound pleomorphism, increased mitotic activity
Ancillary Tests
Positive: Cytokeratin, p63, vimentin, EMA
Negative: Thyroglobulin, TTF-1
Top Differential Diagnoses
Metastases, primary sarcoma, melanoma, lymphoma, primary carcinoma, Riedel thyroiditis
TERMINOLOGY
Synonyms
Anaplastic carcinoma
Spindle and giant cell carcinoma
Sarcomatoid carcinoma
Pleomorphic carcinoma
Dedifferentiated carcinoma
Metaplastic carcinoma
Carcinosarcoma
Definitions
Highly aggressive malignant thyroid neoplasm composed of undifferentiated cells that exhibit immunohistochemical or ultrastructural epithelial differentiation
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Radiation
˜ 10% of patients report radiation exposure
Iodine deficiency (for at least 20 years)
Thyroid Disease
Preexisting benign or malignant thyroid disease in nearly all cases
Longstanding goiter (nodules)
Often decades
Constant stimulation improves odds of transformation
Transformation (dedifferentiation) of preexisting differentiated carcinoma
Papillary, follicular, or poorly differentiated carcinoma
Identified in up to 80% of undifferentiated carcinoma (UC)
Papillary carcinoma is most common (80%)
Pathogenesis
Thyroid follicular epithelial cell origin
Difficult to show origin in many cases
CLINICAL ISSUES
Epidemiology
Incidence
Represents ˜ 2% of all thyroid gland malignancies
Approximately 1-2/1,000,000 population annually
Higher in endemic goiter regions (iodine deficiency), Europe, and low socioeconomic status
Age
Elderly
Vast majority are > 65 years at diagnosis
Gender
Female > Male (1.5:1)
Site
Most are single (60%) lobe tumors
Multifocal (40%) or bilateral (25%)
Presentation
Rapidly expanding neck mass
Exceedingly fast tumor doubling: 1-2 weeks
Fixed and hard mass
Usually long history of thyroid disease
Hoarseness, dysphagia, vocal cord paralysis, cervical pain, and dyspnea are common
Invades into soft tissues (muscle, fat and nerves), esophagus, trachea
Lymphadenopathy common
Hyperthyroidism is uncommon; results from rapid destruction of follicles with hormone release
Laboratory Tests
Leukocytosis can be seen (secretion of macrophage colony-stimulating factor)
Treatment
Options, risks, complications
Multimodality therapy required
Targeted therapy (such as gelfitinib, an EGFR inhibitor and bevacizumab, an antibody against VEGF-R) shows promise
Surgical approaches
Value of surgery is yielding diagnostic material and palliation
Debulking, as resectability is unlikely
May be valuable in limited disease cases
Adjuvant therapy
Combination chemotherapy (doxorubicin, cisplatin)
Response is poor at best
Radiation
Radiation (external beam, 3 dimensional conformal therapy, intensity modulated radiotherapy)
Hyperfractionation or accelerated dosing regimens improves efficacy
Rapid doubling rate requires accelerated dosing
Chemosensitization (doxorubicin) may help
Careful monitoring to minimize toxicity
Prognosis
Rapidly progressive local disease
Many patients have lymph node disease at presentation
Up to 50% cervical adenopathy
Metastases to distant sites common
Up to 50% at presentation
Lungs (50%), bones (15%), brain (10%)
Grave overall prognosis
> 95% die from disease
Median survival: 3 months
Accounts for > 50% of all thyroid cancer deaths
Better prognosis in cases where anaplastic carcinoma is confined to encapsulated tumor or minor component of another tumor
Worse prognosis if patients > 60 years, male, have tumors > 5 cm, or have extensive local disease
IMAGE FINDINGS
General Features
Computed tomography shows extent of disease
Infiltrative (carotid and internal jugular), heterogeneous mass with irregular borders, and necrosis
Calcifications may be seen
MACROSCOPIC FEATURES
General Features
Fleshy to firm mass, typically completely replacing thyroid parenchyma
Infiltrative with irregular borders
Extrathyroidal extension: Soft tissue, larynx, trachea, esophagus, lymph nodes
Pale, white-tan, brown
Commonly variegated, with areas of necrosis and hemorrhage
Sections To Be Submitted
Adequate sampling required to find preexisting or coexisting carcinoma
Size
Range: 1-20 cm
Mean: 6 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Up to 50% of tumors show extrathyroidal extension
Local extension into soft tissues or other organs
Effacement of thyroid parenchyma
Extensive lymph-vascular invasion
Vessel walls invaded or colonized and destroyed
Significant coagulative-type necrosis, hemorrhage, and degeneration
Colloid is absent, but “entrapment” of follicles can be seen at periphery
Desmoplastic stroma may be present
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree