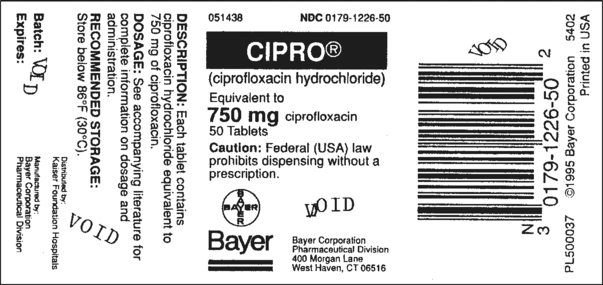
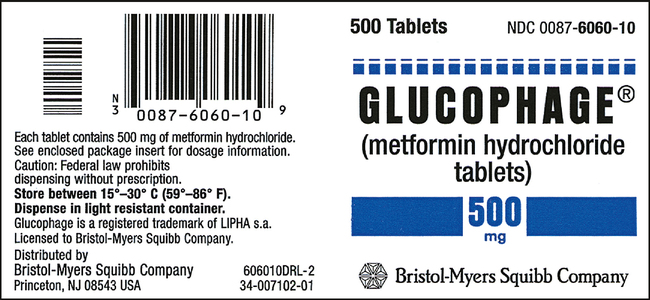
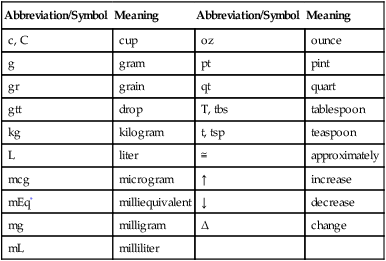
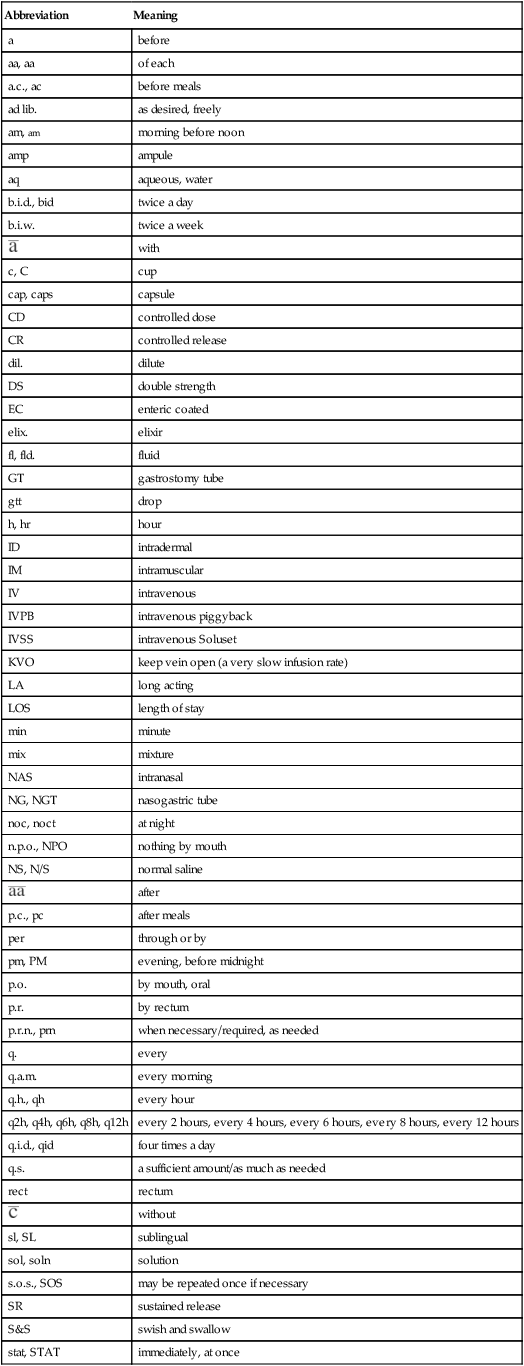
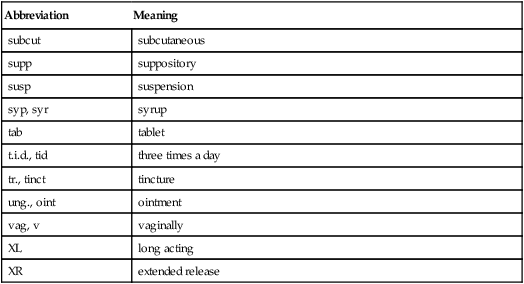
CHAPTER 11 After reviewing this chapter, you should be able to: 1. Identify the components of a medication order 2. Identify the meanings of standard abbreviations used in medication administration 3. Interpret a given medication order 4. Identify abbreviations, acronyms, and symbols recommended by the Joint Commission’s “Do Not Use” List and ISMP’s List of Error-Prone Abbreviations, Symbols, and Dose Designations Before transcribing an order or preparing a dosage, the nurse must be familiar with reading and interpreting an order. To interpret a medication order, the nurse must know the components of a medication order and the standard abbreviations and symbols used in writing a medication order as well as those abbreviations and symbols that should not be used. The nurse therefore must memorize the abbreviations and symbols commonly used in medication orders. The abbreviations include units of measure, route, and frequency for the medication ordered. The common abbreviations and symbols used in medication administration are listed in Tables 11-1 and 11-2 and must be committed to memory. The Joint Commission’s “Do Not Use” List is shown in Table 11-3, and ISMP’s List of Error-Prone Abbreviations, Symbols, and Dose Designations will be presented later in this chapter. TABLE 11-1 Symbols and Abbreviations for Units of Measure Used in Medication Administration *mEq (milliequivalent) is a drug measure in which electrolytes are measured; it expresses the ionic activity of a drug. TABLE 11-2 Commonly Used Medication Abbreviations TABLE 11-3 The Joint Commission’s Official “Do Not Use” List* *Applies to all orders and all medication-related documentation that is handwritten (including free-text computer entry) or on preprinted forms. †Exception: A “trailing zero” may be used only where required to demonstrate the level of precision of the value being reported, such as for laboratory results, imaging studies that report size of lesions, or catheter/tube sizes. It may not be used in medication orders or other medication-related documentation. © The Joint Commission, 2008. Reprinted with permission. The medication may be ordered by the generic or brand name (Figures 11-1 and 11-2). To avoid confusion with another medication, the name of the medication should be written clearly and spelled correctly.
Understanding and Interpreting Medication Orders
VERBAL ORDERS
Abbreviation/Symbol
Meaning
Abbreviation/Symbol
Meaning
c, C
cup
oz
ounce
g
gram
pt
pint
gr
grain
qt
quart
gtt
drop
T, tbs
tablespoon
kg
kilogram
t, tsp
teaspoon
L
liter
≅
approximately
mcg
microgram
↑
increase
mEq*
milliequivalent
↓
decrease
mg
milligram
Δ
change
mL
milliliter
Abbreviation
Meaning
a
before
aa, aa
of each
a.c., ac
before meals
ad lib.
as desired, freely
am, am
morning before noon
amp
ampule
aq
aqueous, water
b.i.d., bid
twice a day
b.i.w.
twice a week

with
c, C
cup
cap, caps
capsule
CD
controlled dose
CR
controlled release
dil.
dilute
DS
double strength
EC
enteric coated
elix.
elixir
fl, fld.
fluid
GT
gastrostomy tube
gtt
drop
h, hr
hour
ID
intradermal
IM
intramuscular
IV
intravenous
IVPB
intravenous piggyback
IVSS
intravenous Soluset
KVO
keep vein open (a very slow infusion rate)
LA
long acting
LOS
length of stay
min
minute
mix
mixture
NAS
intranasal
NG, NGT
nasogastric tube
noc, noct
at night
n.p.o., NPO
nothing by mouth
NS, N/S
normal saline

after
p.c., pc
after meals
per
through or by
pm, PM
evening, before midnight
p.o.
by mouth, oral
p.r.
by rectum
p.r.n., prn
when necessary/required, as needed
q.
every
q.a.m.
every morning
q.h., qh
every hour
q2h, q4h, q6h, q8h, q12h
every 2 hours, every 4 hours, every 6 hours, every 8 hours, every 12 hours
q.i.d., qid
four times a day
q.s.
a sufficient amount/as much as needed
rect
rectum

without
sl, SL
sublingual
sol, soln
solution
s.o.s., SOS
may be repeated once if necessary
SR
sustained release
S&S
swish and swallow
stat, STAT
immediately, at once
subcut
subcutaneous
supp
suppository
susp
suspension
syp, syr
syrup
tab
tablet
t.i.d., tid
three times a day
tr., tinct
tincture
ung., oint
ointment
vag, v
vaginally
XL
long acting
XR
extended release
Do Not Use
Potential Problem
Use Instead
U (unit)
Mistaken for “0” (zero), the number “4” (four), or “cc”
Write “unit”
IU (International Unit)
Mistaken for IV (intravenous)
Write “International Unit”
Q.D., QD, q.d., qd (daily)
Mistaken for each other
Write “daily”
Q.O.D., QOD, q.o.d. qod (every other day)
Period after the Q mistaken for “I” and the “O” mistaken for “I”
Write “every other day”
Trailing zero (X.0 mg)†
Decimal point is missed
Write × mg
Lack of leading zero (.X mg)
Write 0.X mg
MS
Can mean morphine sulfate or magnesium sulfate
Write “morphine sulfate”
MSO4 and MgSO4
Confused for one another
Write “magnesium sulfate”
COMPONENTS OF A MEDICATION ORDER
NAME OF THE MEDICATION
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Understanding and Interpreting Medication Orders

 Critical Thinking
Critical Thinking