Ulcerative Colitis, Colon
Scott R. Owens, MD
Key Facts
Terminology
Chronic, idiopathic, remitting, and relapsing inflammatory disease
Part of spectrum of inflammatory bowel disease (IBD)
Clinical Issues
Rectum usually involved
Variable amount of contiguous disease proximal to rectum
Correlation of histological and endoscopic findings essential for accurate diagnosis
Precise endoscopic appearance of any “polyps” or areas of raised mucosa important
Classically characterized by periods of remission and relapse (“UC flares”)
Markedly ↑ risk of dysplasia/neoplasia in IBD (1-2% ↑ carcinoma risk each year after 10 years)
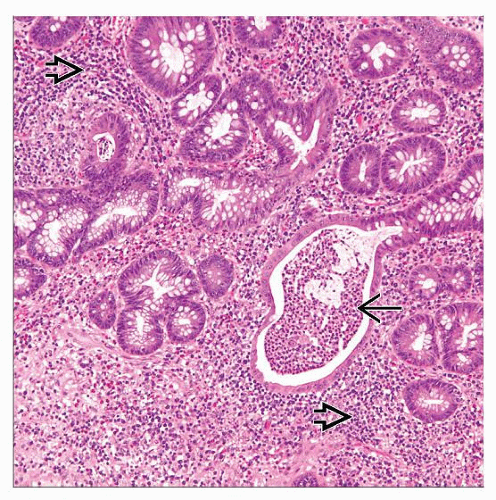
Microscopic Pathology
Lymphoplasmacytic inflammation in lamina propria
Active inflammation
Evidence of chronic and ongoing mucosal injury
Diagnostic Checklist
Not all polypoid dysplasia in UC is DALM
Sporadic adenomas possible
Mucosal granulomas not specific to CD
Distribution of chronic changes most important in determination of type and overall extent of disease
Reporting Considerations
Knowledge of extent of disease important for ongoing assessment of colitis-associated dysplasia
Avoid phrases such as “nonspecific chronic colitis” or “nonspecific chronic inflammation”
TERMINOLOGY
Abbreviations
Ulcerative colitis (UC)
Definitions
Chronic, idiopathic, remitting, and relapsing inflammatory disease
Autoimmune-like
Primarily affects colonic mucosa
Part of spectrum of inflammatory bowel disease (IBD)
Crohn disease (CD) → separate subtype of IBD
Associated with ↑ risk of neoplasia
ETIOLOGY/PATHOGENESIS
Infectious Agents
UC may involve dysregulation of immune response to luminal bacteria
Response to infection and tolerance of commensal organisms normally closely controlled
Loss of normal regulation probably involves genetically determined susceptibility
Genetic Predisposition
Certain HLA haplotypes associated with UC
A7, A11
DRB*12, DRB*103
CLINICAL ISSUES
Epidemiology
Incidence
Around 10-20/100,000 individuals in North America
Incidence reportedly increased in last 2 decades in USA and Europe
Age
Mean age at diagnosis in early 4th decade
3 peaks of incidence
1st in early 20s
2nd in early 40s
3rd in early 60s
Gender
M < F
Occurs earlier in women than in men
Ethnicity
Highest incidence in those of European descent
Site
UC classically involves only colon
Rectum usually involved
Can be termed ulcerative proctitis if limited to rectum
Variable amount of contiguous disease proximal to rectum
Proctosigmoiditis involves sigmoid colon and rectum
Left-sided UC begins in vicinity of splenic flexure and continues distally
Pancolitis begins proximal to hepatic flexure and continues distally
Appendix may be involved
Relatively rare upper tract (particularly duodenal) involvement possible in otherwise typical UC
Extraintestinal manifestations
Arthralgias
Primary sclerosing cholangitis (PSC)
Fibroinflammatory disease of biliary tree
˜ 5% of UC patients also have PSC
˜ 70% of PSC patients have UC
Presentation
Endoscopic Findings
Contiguous mucosal inflammation
Evidence of disease activity
Mucosal erythema
Shallow ulcers
Fresh blood, mucosal oozing
Evidence of chronic inflammation and mucosal injury
Loss of normal vascular pattern
Mucosal granularity
Loss of normal mucosal folds
Correlation of histological and endoscopic findings essential for accurate diagnosis
Allows accurate determination of disease distribution
Ideally, endoscopic report should be available for review by pathologist
Knowledge of biopsy sites and appearance of mucosa biopsied are important
Grossly/endoscopically normal mucosa may be inflamed
Both normal- and abnormal-appearing mucosa should be biopsied throughout colon
Colons with longstanding disease may have extensive changes
Flat, featureless mucosa
Foreshortened, tube-like anatomy
Caused by smooth muscle contraction and mucosal changes
Precise endoscopic appearance of any “polyps” or areas of raised mucosa important
Evidence of colitis-associated dysplasia must be sought
Raised dysplasia often has unusual, worrisome endoscopic appearance
Dysplasia may be endoscopically invisible (flat dysplasia)
Sporadic adenomas and other polyps also possible in UC patients
Biopsy of “polyps” should prompt discussion with endoscopist as to exact appearance
Must know whether polyp was within area affected (currently or historically) by colitis
“Filiform” polyps → long, finger-like or worm-like mucosal projections into colonic lumen
Essentially old inflammatory polyps
May be extensive in longstanding disease (“filiform polyposis”)
Laboratory Tests
Serology
Antineutrophil cytoplasmic antibodies (ANCA)
Occur more often in UC than in CD patients
Anti-Saccharomyces cerevisiae antibodies (ASCA)
Occur in CD patients
May be helpful in establishing diagnosis in difficult cases
Natural History
Classically characterized by periods of remission and relapse (“UC flares”)
1st onset may be abrupt
Most have distal disease (proctitis) at presentation
May continue as proctitis or spread more proximally over time
Some patients present with more extensive colitis (including pancolitis)
Remissions
Some patients essentially symptom-free between periods of activity (“recurrent colitis”)
Others have continuous disease with waxing and waning severity
Toxic megacolon
Severe UC complication occurring in small number of patients
Characterized by extensive dilation, loss of colonic motility, and thinning of wall
May lead to mural necrosis and perforation
Usually occurs in patients with pancolitis
Colitis-associated dysplasia
Markedly increased risk of dysplasia/neoplasia in IBD (1-2% increased carcinoma risk each year after 10 years)
Develops in areas affected by chronic inflammation
Can be flat (endoscopically invisible) or raised (dysplasia-associated lesion/mass [DALM])
Risk directly related to duration and extent of disease
Treatment
Surgical approaches
Colectomy may be urgent/emergent or elective
Urgent indications: Fulminant colitis, perforation, intractable bleeding, toxic megacolon
Elective indications: Failed medical therapy, development of dysplasia/carcinoma
Definitive operation → total abdominal colectomy with ileal pouch-anal anastomosis (IPAA)
Most patients have so-called ileal J-pouch created → serves as fecal reservoir
Interim ileostomy may be constructed, particularly when surgery is emergent
Drugs
1st line therapy (effective in mild-moderate disease)
5-aminosalicylic acid (5-ASA, mesalamine)
Corticosteroids
Refractory or continuously active disease
Azathioprine
6-mercaptopurine (6-MP)
Other immunomodulators (tacrolimus, methotrexate, infliximab)
Novel therapies
Probiotics → alter luminal flora (may be beneficial as adjunctive therapy)
Prognosis
Chronic, usually unrelenting disease
High probability of active disease (˜ 75%) in any year following year in which disease was active
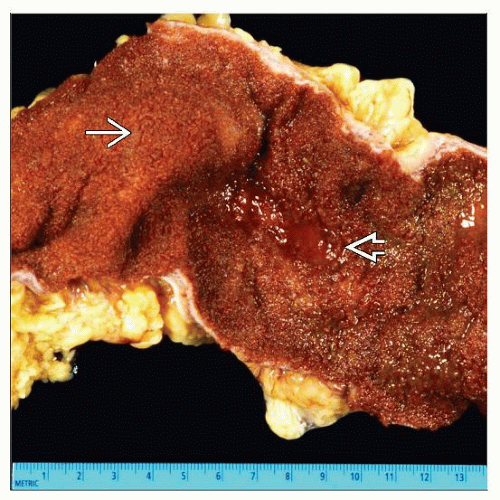
MACROSCOPIC FEATURES
General Features
Mucosal abnormalities in active disease
Granularity and erythema
Pseudopolyps
Inflamed projections of regenerative mucosa created when ulcers undermine adjacent mucosa
May impart “cobblestone” appearance to mucosa if multiple
Shallow ulcers
Adherent blood &/or mucopurulent exudate
Chronic changes
Flattened, finely granular mucosa
Muscular contraction and mucosal fibrosis may lead to rigid, “foreshortened” colon
Disease distribution
Should be described in relation to normal anatomical landmarks
Sections to Be Submitted
Colectomy specimens should be systematically sampled from proximal to distal
Allows for precise determination of histological extent of disease
Sections should include
Ileum, ileocecal valve
Appendix (submitted as with appendectomy specimen)
Cecum and ascending colon
Hepatic flexure, transverse colon, splenic flexure
Descending colon
Sigmoid colon
Rectum
Sampling of transition between normal and abnormal mucosa useful
Areas of polypoid, raised, or unusual-appearing mucosa should be sampled
Some cases have innumerable pseudopolyps &/or filiform polyps
Polyps with unusual appearance particularly important to sample
Large lesions must be serially cut and explored for underlying invasive carcinoma
Any large lymph nodes may be submitted
Systematic and careful lymph node dissection crucial if lesion(s) suspicious for carcinoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree