, Tsunehisa Kaku2, Toru Sugiyama3 and Steven G. Silverberg4
(1)
Matsue City Hospital, Matsue, Shimane, Japan
(2)
Department of Health Sciences, Department of Health Sciences Graduate School of Medical Sciences, Fukuoka, Fukuoka, Japan
(3)
Department of Obstetrics and Gynecology, Iwate Medical University School of Medicine, Morioka, Iwate, Japan
(4)
Department of Pathology, University of Maryland School of Medicine, Baltimore, MD, USA
Clear cell carcinoma of the ovary is one of the most instantly recognizable ovarian tumors and probably the single most recognizable type of ovarian adenocarcinoma. In our own review of over six hundred cases, over 95 % of cases submitted as clear cell carcinoma (CCC) were accepted on histopathologic central review, and a similar proportion of the cases were accepted in a review done in Canada [1]. The picture at scanning lens magnification is one of micropapillary, tubulocystic, and solid patterns, often with admixtures of more than one of these patterns (and occasionally others as well) in the same tumor (Figs. 3.1, 3.2, 3.3, 3.4, 3.5, 3.6, 3.7, 3.8, 3.9, 3.10, 3.11, 3.12, 3.13, 3.14, 3.15, 3.16, 3.17, 3.18, and 3.19).
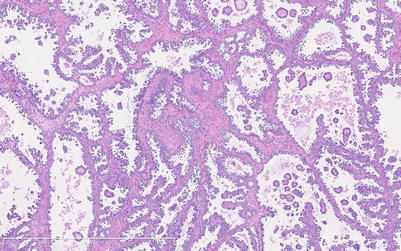
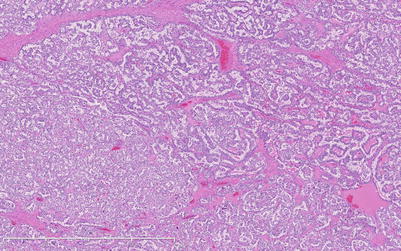
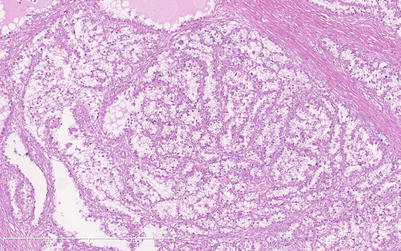
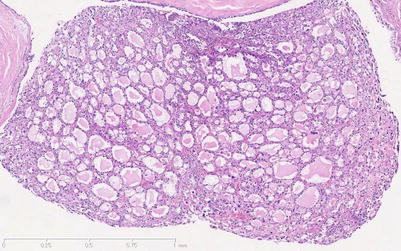
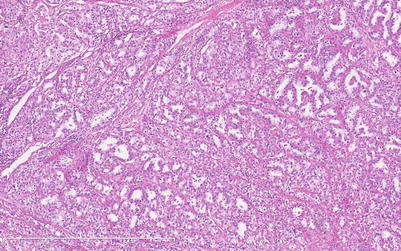
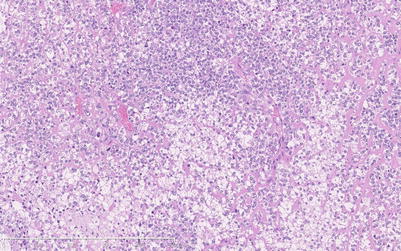
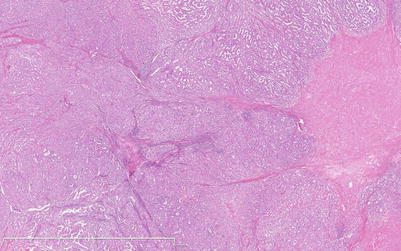
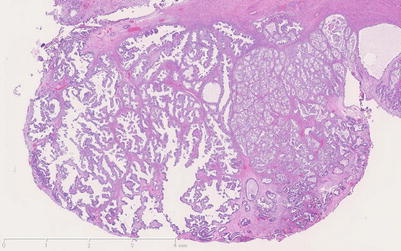
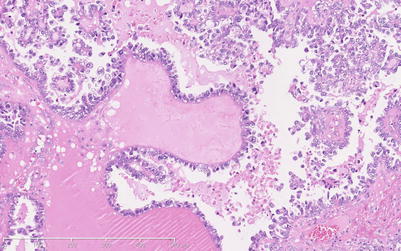
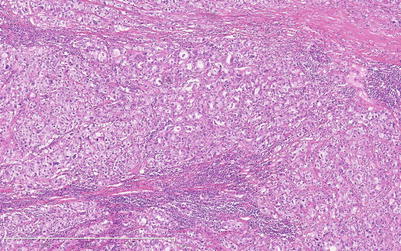
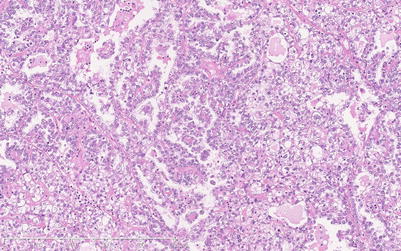
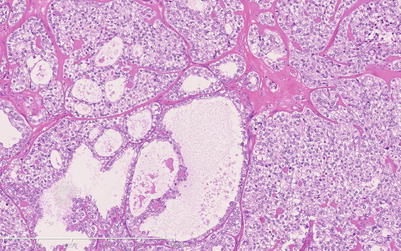
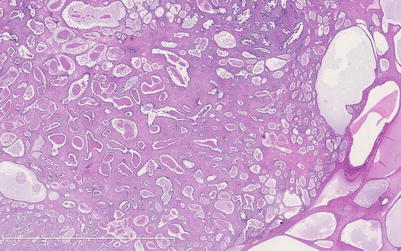
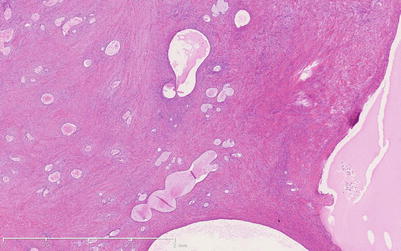
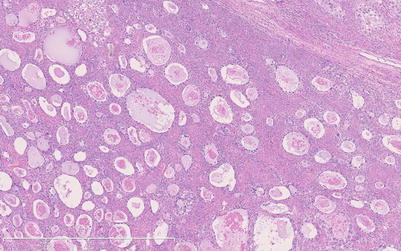
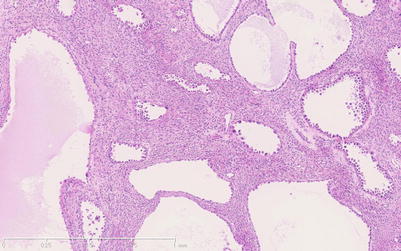
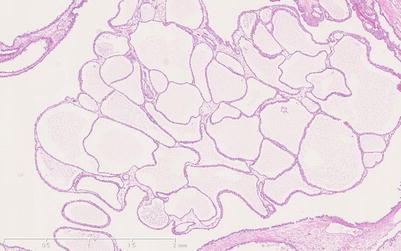
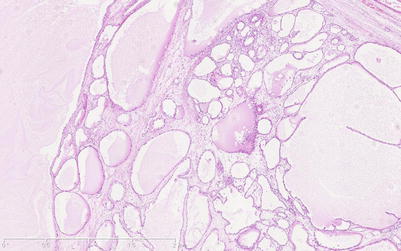
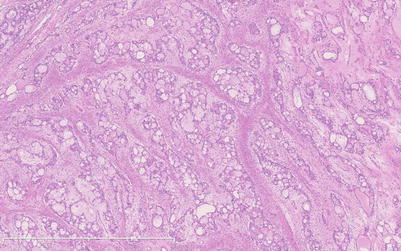
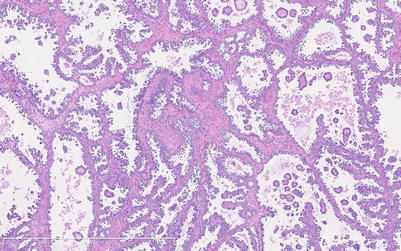
Fig. 3.1
Low-power magnification view of ovarian clear cell carcinoma (CCC) with predominantly micropapillary pattern. Micropapillae with largely hyalinized stroma grown into large cystic spaces
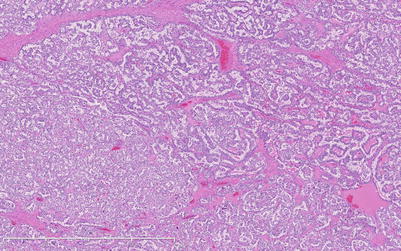
Fig. 3.2
Tubulo-papillary pattern in CCC, with admixture of micropapillary and tubular growth
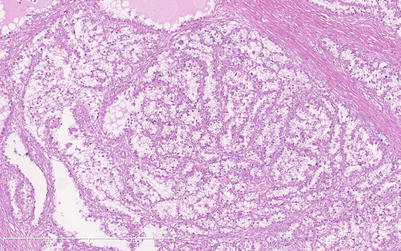
Fig. 3.3
Tubular pattern, with uniformly sized tubules lined by predominantly clear cells
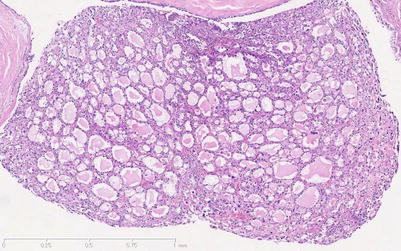
Fig. 3.4
Tubular pattern, with small tubules containing myxoid-appearing debris
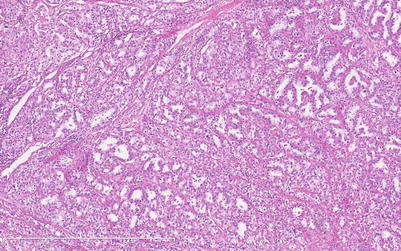
Fig. 3.5
Tubular pattern, in which there is more variation in tubular size and shape
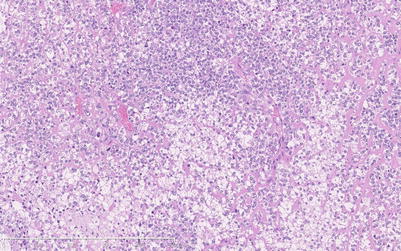
Fig. 3.6
Solid pattern of growth, in which clear cytoplasm can be seen in a good many but not all of the cells at this magnification
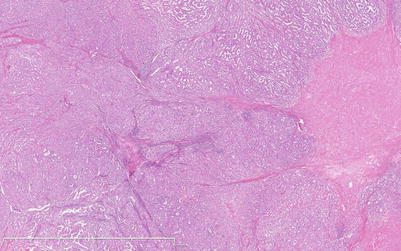
Fig. 3.7
Admixture of solid and tubular growth patterns
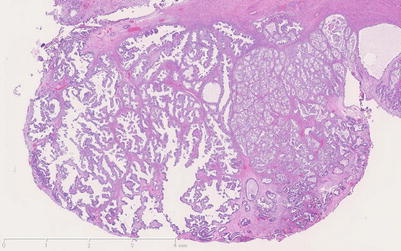
Fig. 3.8
Admixture of micropapillary and solid patterns
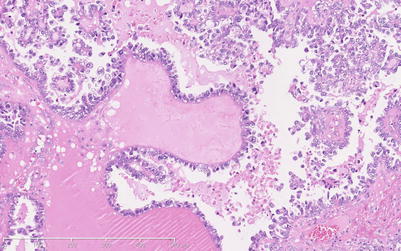
Fig. 3.9
Papillary growth of CCC featuring both macro- and micropapillae
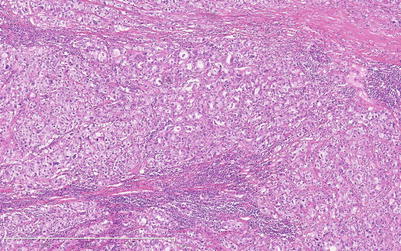
Fig. 3.10
Admixture of solid and tubular patterns in a predominantly fibrous stroma
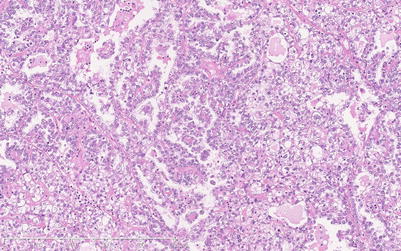
Fig. 3.11
Admixture in one field of tubular, micropapillary, and solid grown patterns
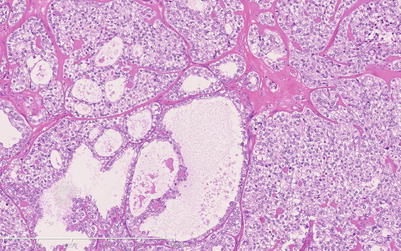
Fig. 3.12
Solid and tubulocystic growth patterns
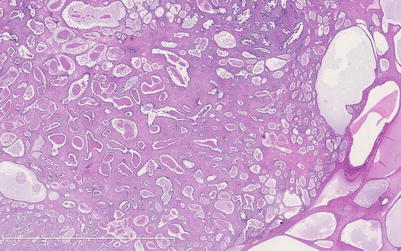
Fig. 3.13
Adenofibromatous pattern of CCC, in which both small and large tubules grow within a largely fibromatous stroma
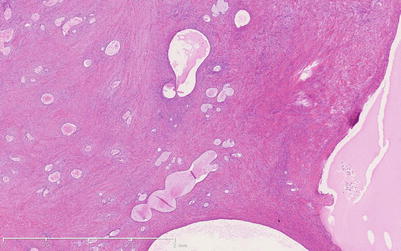
Fig. 3.14
Adenofibromatous pattern with more widely spaced tubules, some of which are cystically dilated, than in Fig. 3.13
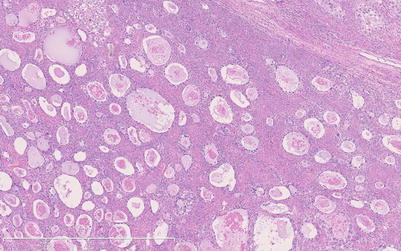
Fig. 3.15
Adenofibromatous pattern in which the tubules are separated by a more cellular fibrous stroma. Note the necrotic-appearing debris within tubular lumina
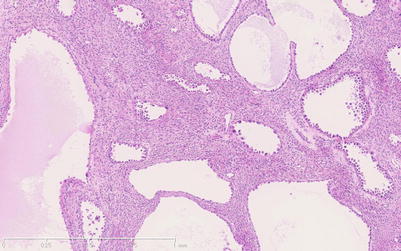
Fig. 3.16
Adenofibromatous pattern in which a cellular ovarian cortical-type stroma is present. Hobnail type cells are easily seen lining the tubules at this magnification
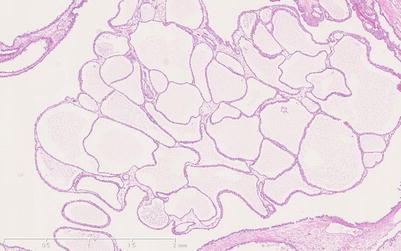
Fig. 3.17
Tubulocystic pattern in which the tubular structures are all cystic and minimal stroma remains between them
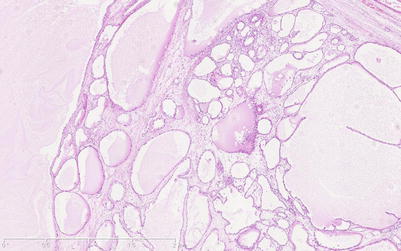
Fig. 3.18
Another tubulocystic growth pattern in which small tubules and larger cystically dilated ones coexist
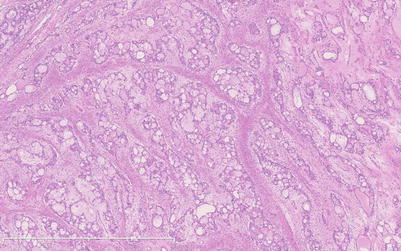
Fig. 3.19
Variant of tubulocystic pattern in which tubules have coalesced to create a cribriform growth pattern
The adenofibromatous pattern (Figs. 3.13, 3.14, 3.15, and 3.16) is present (alone or mixed with other patterns) in 20–25 % of cases. Atypia and evidence of stromal invasion are often minimal in these foci, leading to the differential diagnosis with benign or borderline clear cell adenofibroma. Multiple sections may be required for the diagnosis of CCC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


