FIGURES 7-1A AND 7-1B Twelve-lead ECG during typical AVNRT and normal sinus rhythm. During typical AVNRT, the QRS complex is usually narrow, and the P wave is often absent due to simultaneous activation of the atrium and ventricle. If, however, the atrial depolarization is slightly delayed, a portion of the P wave may be seen at the end of the QRS complex and be manifest as a pseudo R’ wave in lead V1 or a pseudo S wave in the inferior leads. Figure 7-1A was taken during tachycardia at a rate of 173 bpm. No clear P wave was discernible, but terminal deflections were seen in leads V1 and II consistent with pseudo R’ and pseudo S waves (labeled R’ and S, respectively). A comparison to the baseline ECG (shown in Figure 7-1B) is required to confirm this, and as can be seen there were no R’ or S waves in leads V1 or II during normal sinus rhythm.
EPIDEMIOLOGY
AVNRT is the most common type of regular narrow QRS complex SVT and accounts for approximately 60% to 70% of cases. There is a higher incidence in women and younger individuals, with the mean age of symptom onset at 30 years.1,2 The slow-fast variant of AVNRT accounts for nearly 90% of all AVNRT and is therefore referred to as typical AVNRT.
CLINICAL PRESENTATION
The onset of symptoms with AVNRT are usually paroxysmal in nature occurring suddenly without warning, but in some patients episodes can be brought on during high adrenergic states such as exercise. Symptoms that occur during AVNRT, like other forms of PSVT, are nonspecific and include palpitations, shortness of breath, chest pain, and dizziness. Frank syncope occurs rarely and appears to be rate-related since it is uncommon at rates less than 170 bpm.3
ANATOMY
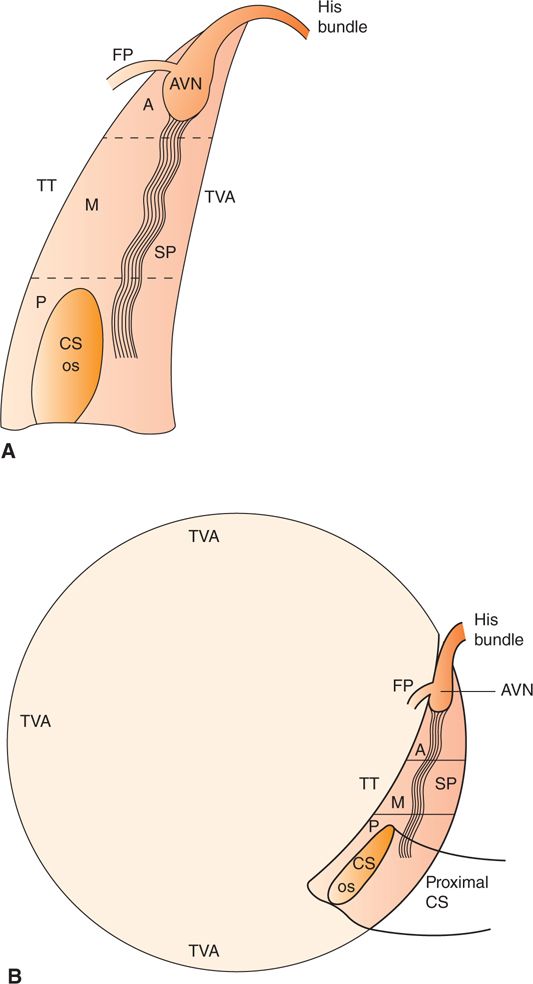
AVNRT utilizes both AV nodal and peri-AV nodal tissue as substrate for the reentrant circuit.2 This circuit is located within the triangle of Koch, which is boarded by the tricuspid annulus anteriorly, the tendon of Todoro posteriorly, and the coronary sinus inferiorly (Figure 7-2A and B). The triangle of Koch is divided into three zones: anterior, middle, and posterior. The anterior zone is located at the apex of the triangle and contains the compact AV node and initial portion of the His bundle. The middle zone is located just inferior to the anterior zone, and the posterior zone is located at the base of the triangle and contains the ostium of the coronary sinus. The fast and slow pathways that make up the reentrant circuit for typical AVNRT are also located within the triangle of Koch. The fast pathway is located in the anterior portion of the triangle in close proximity to the compact AV node. The slow pathway is found in the middle or posterior portions of the triangle often around the coronary sinus ostium. The fast and slow pathways join at the lower and upper common pathways. The latter is located within the AV node proximal to the bundle of His.4 Understanding this anatomy is especially important when ablative therapy is contemplated. Energy delivery in the anterior zone targeting the fast pathway carries a significant risk of creating AV block since this is where the compact AV node and proximal His bundle are located.
FIGURES 7-2A AND 7-2B Anatomy of the triangle of Koch. Figure 7-2A depicts the anatomy in the right anterior oblique (RAO) view, and Figure 7-2B depicts the anatomy in the left anterior oblique (LAO) view. The triangle of Koch is bordered anteriorly by the tricuspid valve annulus (TVA), posteriorly by the Tendon of Todaro (TT), and inferiorly by the coronary sinus ostium (CS os). The anterior (A) zone contains the compact atrioventricular node (AVN) and the fast pathway (FP). The middle (M) and posterior zones contain the slow pathway (SP), and the posterior zone also includes the coronary sinus ostium (CS os).
ELECTROPHYSIOLOGY
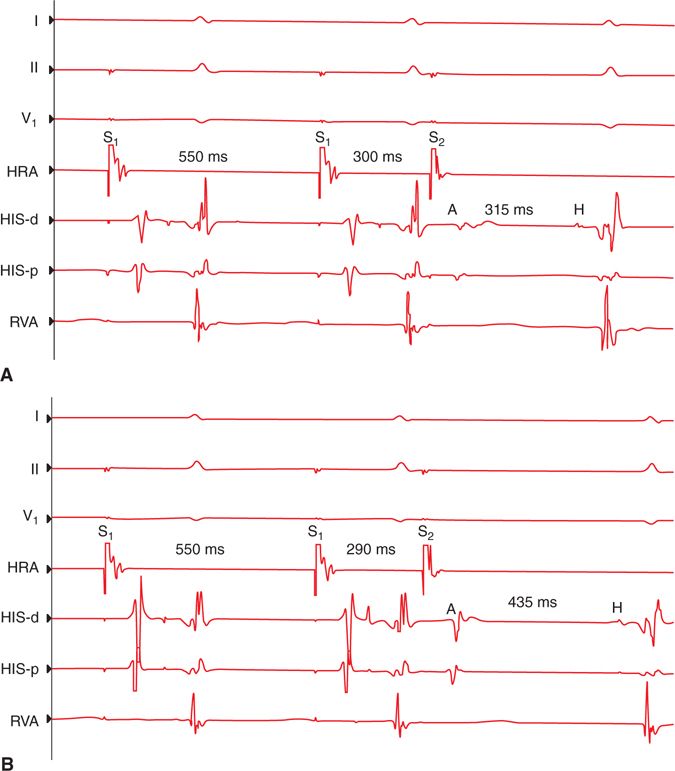
The basic components of a typical AVNRT circuit are a slow pathway that conducts in the antegrade direction, a fast pathway that conducts in the retrograde direction, and upper and lower common pathways which link the fast and slow pathways. Antegrade conduction over both a fast and slow AV nodal pathway (“dual AV nodal physiology”) can usually be demonstrated in patients with typical AVNRT. The fast pathway has more rapid conduction but usually has a longer refractory period compared to the slow pathway. When an appropriately timed premature atrial contraction occurs, it will block in the fast pathway and conduct over the slow pathway to the His bundle and ventricle resulting in significant prolongation of the AH and PR intervals compared to the normal sinus beat. This electrophysiologic (EP) phenomenon of changing conduction from the fast to the slow pathway is known as an “AV nodal Jump.”5 During an EP study, an AV nodal jump is defined as a 50 ms increase in the AH interval corresponding to a 10 ms decrease in the A1-A2coupling interval during atrial extrastimulus testing (Figure 7-3A and B).
FIGURES 7-3A AND 7-3B Dual AV nodal physiology. These figures demonstrate atrial extrastimulus pacing at a drive train of 550 ms. Shown are surface leads I, II, and V1 and intracardiac recordings from the high right atrium (HRA), His bundle distal (His-d), His bundle proximal (His-p), and right ventricle apex (RVA). In Figure 7-3A, with an S2 coupling interval of 300 ms the corresponding atrial to His (AH) interval is 315 ms. In Figure 7-3B the S1S2 coupling interval is 290 ms with a corresponding AH interval of 435 ms, an increase of 120 ms. An AH interval increase of >50 ms for a decrement in the S1S2 coupling of 10 ms defines an AV nodal jump and indicates the presence of antegrade dual AV nodal physiology.
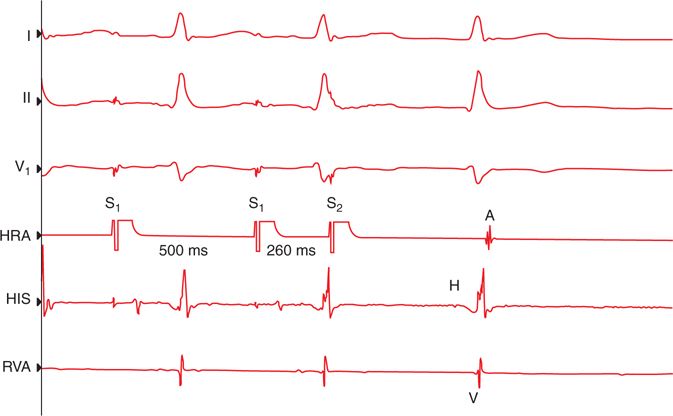
The finding of antegrade dual AV nodal physiology only defines the presence of antegrade fast and slow pathways, but it does not demonstrate the existence of a retrograde fast pathway, which is a necessary component of the AVNRT circuit. The presence of a retrograde fast pathway is suggested when there is rapid ventriculo-atrial (VA) conduction during ventricular pacing. Some patients with typical AVNRT may have very poor VA conduction or VA dissociation during baseline EP testing and may require the addition of an isoproterenol infusion to elicit fast pathway conduction.5 The presence of a retrograde fast pathway is confirmed if an AV nodal echo can be demonstrated during atrial pacing maneuvers (Figure 7-4). An AV nodal echo is the result of antegrade conduction down the slow pathway to the lower common pathway and then simultaneous conduction retrograde over the fast pathway to the atrium and antegrade over the His-Purkinje system to the ventricle. It is this simultaneous or “in parallel” conduction along with very rapid retrograde fast pathway conduction that results in the short VA times (≤70 ms recorded on the His bundle catheters) that are characteristic of typical AVNRT. In some cases the VA time during tachycardia may be zero or even negative. This can occur if the conduction time from the lower common pathway retrograde to the atrium is equal to or faster than the antegrade conduction time to the ventricle. If after an AV node echo the slow pathway is not refractory, then antegrade conduction can occur over the slow pathway, and typical AVNRT can be induced (Figure 7-5A and B).
FIGURE 7-4 AV nodal echo. This figure demonstrates atrial extrastimulus pacing at a drive train of 550 ms. Shown are surface leads I, II, and V1 and intracardiac recordings from the high right atrium (HRA), His bundle (His), and right ventricle apex (RVA). An S1S2 coupling interval of 260 ms results in conduction down the slow pathway and a prolonged AH interval. At this degree of AH prolongation an atrial event (A) with a short VA conduction time occurs. This is an AV nodal echo and confirms the presence of retrograde fast pathway conduction.
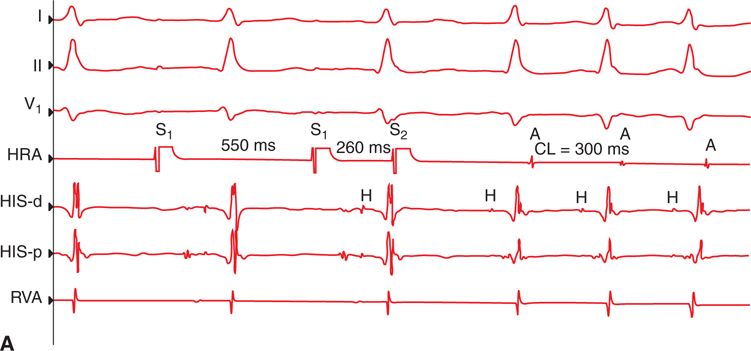
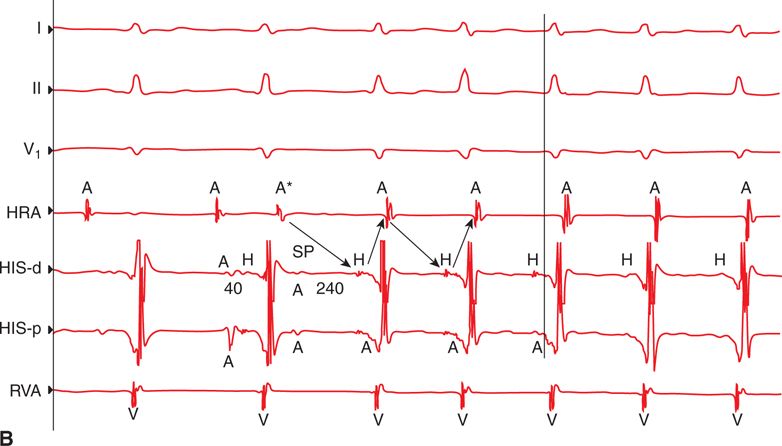
FIGURE 7-5A Initiation of AVNRT. Figure 7-5A demonstrates atrial extrastimulus pacing at a drive train of 550 ms. Shown are surface leads I, II, and V1 and intracardiac recordings from the high right atrial (HRA), His bundle distal (His-d), His bundle proximal (His-p), and right ventricular apex (RVA). An S1S2 coupling interval of 260 ms results in antegrade conduction down the slow pathway and initiation of typical AVNRT at a cycle length of 300 ms. The atrial, His, and ventricular electrograms are labeled A, H, and V, respectively, on the intracardiac recordings.
FIGURE 7-5B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree