Type III Collagen Glomerulopathy
Helen Liapis, MD
Joseph Gaut, MD, PhD
Key Facts
Terminology
Idiopathic glomerular disease defined by accumulation of mesangial and subendothelial type III collagen
Clinical Issues
Rare (< 0.1% of biopsies)
Presents with hematuria or proteinuria
Hemolytic uremic syndrome, children
Variable disease course
Increased serum and urine procollagen III peptide
Microscopic Pathology
Lobular glomeruli without inflammation
Thickened capillary walls
Mesangial and capillary wall expansion with eosinophilic, silver-positive material
Electron microscopy
Mesangial and subendothelial curvilinear fibrils
Fibers tend to be frayed and curved, ˜ 60 nm periodicity
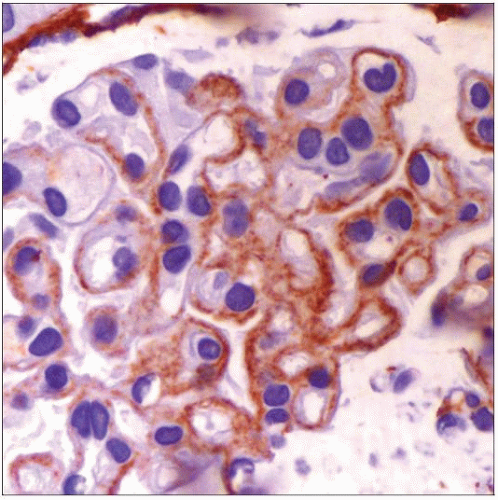
Immunohistochemical staining for type III collagen positive in mesangium and GBM
Top Differential Diagnoses
Nail-patella syndrome
Hereditary multiple exostoses
Fibronectin glomerulopathy
Fibrillary glomerulopathy
Diagnostic Checklist
Diagnosis made by demonstration of collagen III in glomeruli
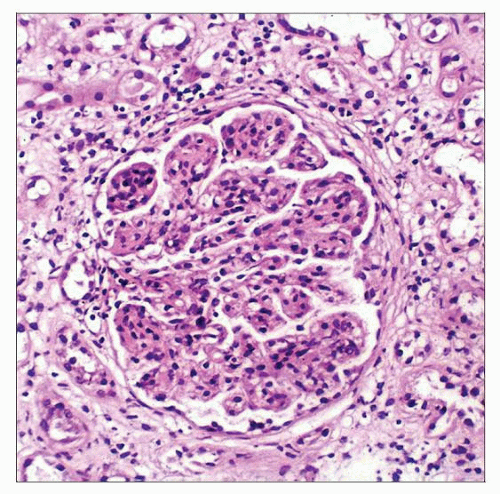 Type III collagen glomerulopathy has a varied glomerular pathology. In this particular case, the glomeruli are hypercellular with a lobular appearance. (Courtesy G. Herrera, MD.) |
TERMINOLOGY
Synonyms
Collagenofibrotic glomerulopathy
Definitions
Idiopathic glomerular disease defined by accumulation of mesangial and subendothelial type III collagen
Initially described by Arakawa and colleagues in 1979
ETIOLOGY/PATHOGENESIS
Proposed Etiologies
Probably systemic disease of collagen metabolism
Increased level of N-terminal procollagen type III in blood
Indicative of increased synthesis/catabolism
Deposit in glomeruli
Excreted in urine
Occasional cases in siblings suggest a genetic component, as yet unidentified
Some believe this is a primary disease of the glomerulus
CLINICAL ISSUES
Epidemiology
Incidence
Rare (˜ 0.1% of biopsies)
Age
All ages
Gender
M:F = 1:1
Ethnicity
Majority of reported cases are Japanese
Cases also reported in USA, Europe, India, South America, China
Presentation
Microhematuria
Hypertension
Edema
Proteinuria, nephrotic range in 60%
Anemia
Adults typically have anemia of chronic disease
Children occasionally present with thrombotic microangiopathy
Hemolytic uremic syndrome, children
Laboratory Tests
10-100x increase in serum and urine N-terminal procollagen type III peptide (PIIINP)
Treatment
Drugs
No specific treatment
Steroid therapy is reported to slow disease progression
Prognosis
Variable disease course, limited data
˜ 35% of adults and ˜ 90% of children progress to end-stage renal failure
MICROSCOPIC PATHOLOGY
Histologic Features
Glomeruli
Lobular or mesangial hypercellularity, variable
Nodular pattern at times resembles diabetic glomerulopathy
Expansion of mesangium with eosinophilic, silver-positive material
Thickening of GBM
Occasional double contours
Closure of capillary loops
No inflammation
No specific changes in tubules, interstitium, or vessels
ANCILLARY TESTS
Immunohistochemistry
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree