Chapter 8
Treatment Burden and Multimorbidity
Katie I. Gallacher1, Victor M. Montori2, Carl R. May3, and Frances S. Mair1
1General Practice and Primary Care, Institute of Health and Wellbeing, University of Glasgow, UK
2Knowledge and Evaluation Research Unit, Department of Health Sciences Research and Medicine, Mayo Clinic, USA
3Faculty of Health Sciences, University of Southampton, UK
Overview
- Patients with long-term conditions experience treatment burden
- The key components of treatment burden are learning about treatments and their consequences, engaging with others, adhering to treatments and lifestyle changes and monitoring treatments
- Multimorbidity can affect patients by (1) increasing treatment burden and (2) decreasing the capacity of the patient to cope
- Excessive treatment burden can reduce adherence to management plans and lead to negative outcomes for patients and their caregivers
- Better ways of measuring treatment burden are required
- Changes are needed at practice and policy level to minimize treatment burden and improve patient outcomes among multimorbid patients.
Definition of treatment burden
Treatment burden refers to the tasks that patients with a long-term condition must perform to respond to the requirements of their healthcare providers and the impact that these practices have on their functioning and well-being. This includes all activities that healthcare providers require those with long-term conditions to perform to manage their illness, including learning about treatments and their side effects, taking medications, enacting lifestyle changes, attending appointments, undergoing investigations and monitoring symptoms (see Figure 8.1). Treatment burden encompasses a different set of burdens to those imposed by the illness itself such as symptoms, disabilities and psychological difficulties. However, illness and treatment burden certainly influence one another and also overlap. For example, a stroke patient who is suffering from depression (illness burden) may fail to carry out the demanding daily physiotherapy exercises assigned to him (treatment burden) and therefore fail to improve physically (illness burden).
Figure 8.1 Polypharmacy is only one aspect of treatment burden but a substantial one for many patients with multimorbidity.
Patient capacity
Patients suffering from different types and levels of morbidity will experience different kinds of treatment burden, often as a result of management decisions taken by health professionals. The capacity that a patient has to cope with these demands will influence the patient’s experience. Internal factors may include personal capabilities, level of education, personality, cognition and psychological condition; external factors may include amount of social support, employment, financial circumstances and available community facilities. As healthcare providers impose heavier treatment burden, then the capacity of patients and caregivers to accommodate these demands is stretched until a ‘coping threshold’ is reached, beyond which the balance tips and patients fail to follow treatments. Alternatively, patients may perceive the coping threshold approaching and unilaterally prioritize their workload in order to ‘fit’ their capacity and maintain a balance. Or patients with stable treatment plans may see their capacity reduced by competing demands (personal or work-related, emotional or financial, mental or physical illness) and be no longer able to sustain the current treatments (see Figure 8.2).
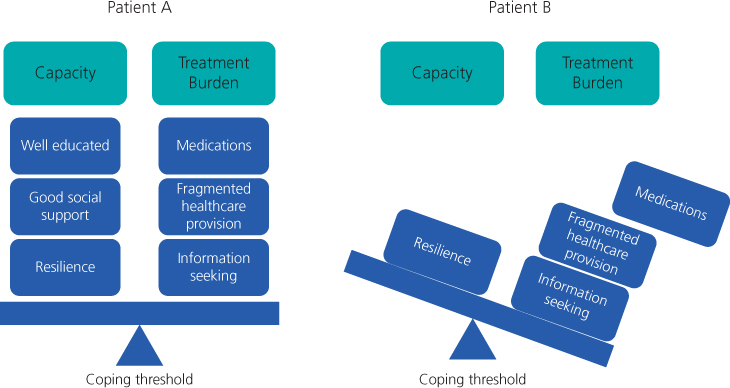
Figure 8.2 A demonstration of the balance between patient capacity and treatment burden. The two scales each represent a different patient. Patient A: treatment burden and patient capacity are balanced, the patient maintains their management plan. Patient B: treatment burden outweighs patient capacity, the coping threshold is exceeded and the balance tips leading to a collapse in the management and failure to follow treatments.
Treatment burden and multimorbidity
As we have seen in Chapter 2, multimorbidity is becoming increasingly common. Long-term conditions require lifelong management with input from health services and long-term investment from patients. Owing to advances in science and technology, patients are living longer, following more complicated management plans, utilizing more health services (Chapter 4) and therefore experiencing an increasing level of treatment burden.
Multimorbidity can affect patients by (1) increasing treatment burden and (2) decreasing the capacity of the patient to cope with these demands. Treatment burden is likely to increase with each extra morbidity not only because of an increase in the volume of tasks but also because these may actually negatively interact with each other [e.g. drug interactions (Figure 8.1) or clashing appointment times]. Recently, health services have increasingly moved away from the provision of generalized care to a more speciality-based service increasing the number of healthcare professionals involved with each patient and resulting in a more disease-centred approach. This has resulted in an increase in treatment burden for patients. As mentioned earlier, multimorbidity may decrease patient capacity as patients are more likely to suffer from a poorer quality of life and functional status (Chapter 3), as well as being more at risk of depression and psychological disorders (Chapter 9). All of these factors may decrease the patient’s ability to cope with the demands of illness management.
Patient adherence and other outcomes
As discussed earlier, increasing levels of treatment burden may overwhelm the patient, pushing them past their ‘coping threshold’ and leading to a reduced adherence to therapies (see Figure 8.2). Non-adherence may result from patients feeling that they have too much to cope with and cutting back on aspects of care to make life more manageable. It may also result from a misunderstanding or error by the patient as formal or informal care processes become increasingly complicated. Non-adherence in the management of long-term conditions is a global health problem identified by the World Heath Association. Non-adherence is associated with negative outcomes such as increased morbidity and mortality, difficulties in professional–patient relationships and wasted expenditure by health services. Whilst improving patient knowledge, through education and access to sources of information, positively affects adherence, there is good evidence that workload factors, including the scheduling of treatments and the logistics of access to care, can play a major role. It is therefore of vital importance that the issue of treatment burden is addressed in order to improve patient outcomes (see Figure 8.3).
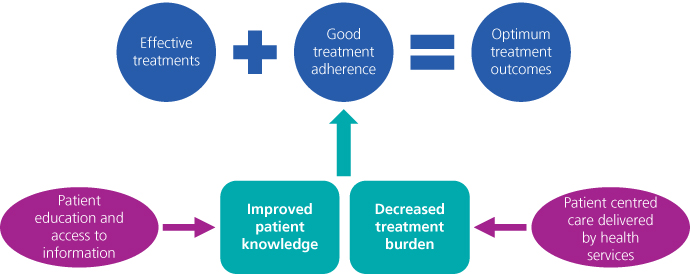
Figure 8.3 The association between knowledge, treatment burden and adherence.
Typology of treatment burden
The key components of treatment burden are learning about treatments and their consequences, engaging with others, adhering to treatments and lifestyle changes and monitoring treatments (see Figure 8.4, Box 8.1).
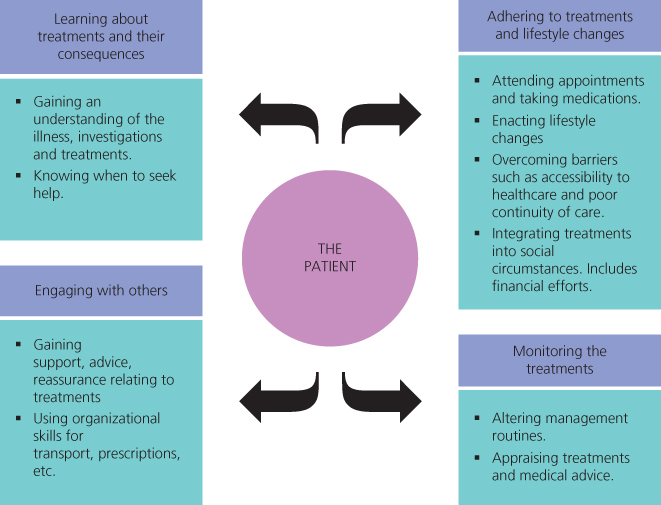
Figure 8.4 Typology of treatment burden.
Gallacher et al. 2011.
Box 8.1
What are the key components of treatment burden?
What are the effects of excessive treatment burden in patients with multimorbidity?
How might treatment burden be decreased in patients with multimorbidity?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


