Summary by Stephen G. Van Ooteghem, MD, MSW, Gail D’Onofrio, MD, and Federico E. Vaca, MD, MPH
81
Based on “Principles of Addiction Medicine” Chapter by Federico E. Vaca, MD, MPH, FACEP, and Gail D’Onofrio, MD
INTRODUCTION
Alcohol and other drug use contributes to a substantial portion of injury events. Injured patients with alcohol and drug involvement tend to suffer more severe complications, with wide-ranging effects on families, the workplace, and society. There is a growing body of literature describing the epidemiology of this social problem, as well as screening tools and interventions that identify and treat high-risk populations.
EPIDEMIOLOGY OF ALCOHOL- AND OTHER DRUG-RELATED INJURY
Alcohol is involved in over 50% of major traumas and 22% of minor traumas. It is a major risk factor for all categories of intentional and unintentional injuries and is implicated in approximately one third of fatal car accidents. Alcohol has been found to be associated with numerous types of traumatic injury, including fatal burns, boating fatalities, interpersonal violence, and work-related injuries. Alcohol is similarly implicated in injuries to the adolescent population.
Among injured patients, alcohol and drug dependence is correlated with more severe injury. Of patients with injuries severe enough to require hospital admission, 54% of adult trauma patients had a history of substance abuse, 24% had a current diagnosis of alcohol use disorder, and 18% had a current diagnosis of a drug use disorder.
The association between traumatic injury and other drug use has not been as well described. However, there are studies linking cocaine to as many as 25% of motor vehicle crash (MVC) fatalities and marijuana to increased risk for MVC.
SCREENING FOR ALCOHOL PROBLEMS IN THE EMERGENCY DEPARTMENT
Screening and intervention can take place at any time during the ED visit by appropriately trained health care providers. It is recommended that the screening protocol be a routine component of the ED visit. Interventions are targeted to the individual patient and must take into account the spectrum of alcohol use and high-risk behaviors pertinent to each particular patient. For example, an at-risk drinker might be encouraged to reduce the quantity of consumption, a harmful drinker might be encouraged to avoid driving while intoxicated, and a dependent drinker might be encouraged to accept a referral to specialized treatment program.
Alcohol use exists along a spectrum, with three broad categories of increasing severity: at-risk drinkers, harmful drinkers, and dependent drinkers. As defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), at-risk drinkers have 14 or more drinks in a week, or 4 or more on a given day for men, and 7 or more drinks in a week, or 3 or more on a given day for women. Compared to normal controls, at-risk drinkers are more likely to experience alcohol-related consequences in the future. Harmful drinkers experience negative consequences related to their drinking such as medical, social, and legal problems. Harmful drinkers may have poor work or school performance, familial strife, car crashes, and instances of driving under the influence (DUIs). Dependent drinkers experience the physiologic symptoms of tolerance and withdrawal and often display more severe social and occupational dysfunction.
Conventional screening systems such as CAGE, TWEAK, and AUDIT have identified harmful and dependent drinkers, but are not ideal for identifying at-risk drinkers. More recently, the Screening, Brief Intervention, and Referral to Treatment (SBIRT) model has screened for at-risk drinkers using the NIAAA quantity and frequency questions, the AUDIT-C (a shortened version of the AUDIT), and the ASSIST. These tools are ideally suited for emergency department use in that these tools are quickly and easily administered, and are suitably sensitive and specific for identifying at-risk drinkers as well as harmful and dependent drinkers. Because at-risk drinking is responsible for a considerable portion of alcohol-related injuries, this is a useful characteristic.
The NIAAA screen consists of the interviewer asking how many times in the past year the patient has had more than five drinks in a day (men) or four drinks in a day (women). Any answer over “0” is considered positive. The AUDIT-C is composed of three multiple-choice questions, which assess the quantity, frequency, and intensity of drinking behavior. The patient is assigned a score based upon the answers, which can be used to identify suitable candidates for intervention.
INTERVENTIONS WITH INJURED PATIENTS
Alcohol- or drug-related injury provides a unique opportunity for intervention, referred to as a “teachable moment.” In fact, many patients change their drinking behavior to some extent following these injuries, even without formal intervention. The degree to which patients alter their behavior appears to be related to the degree to which they attribute their alcohol or drug use to the injury event. In one study of emergency department patients who were injured in MVCs and who had been drinking alcohol, more than one third connected their alcohol use to the injury event. Studies have shown that intervention reduces alcohol consumption, as well as the occurrence of alcohol-related injuries. One systematic review, which evaluated 19 randomized controlled trials, found that treatment for problem drinking was associated with a reduction in suicide attempts, domestic violence, falls, drinking-related injuries, hospitalizations, and deaths. Of seven trials comparing intervention with control group, nearly all showed a decrease in injury-related outcomes, including a 65% reduction in accidental and violent deaths. Because emergency department patients are more likely to report heavy drinking, alcohol dependence, or prior treatment for alcohol-related problems as compared to patients in primary care clinics, they are an ideal group for intervention.
Brief interventions consist of short counseling sessions. Structurally, these incorporate elements summarized by the FRAMES mnemonic: feedback, responsibility, advice, menu of strategies, empathy, and self-efficacy. Elements such as goal setting, timing, and follow-up may also be incorporated. Behavior changes are agreed upon with the patient and vary based upon the individual’s drinking patterns and any high-risk behaviors in which they are engaged.
Many of the recent ED SBIRT studies, where the screening and brief intervention model is applied to ED patients, have shown promising results. In one study, ED patients receiving brief intervention consumed fewer drinks at 3 months and 1 year compared to controls. At-risk drinkers appeared to benefit more than dependent drinkers. Other studies have shown a decrease in alcohol use and abuse by adolescents, including reduced rates of drinking and driving, alcohol-related injuries, and alcohol-related social dysfunction. One RCT showed a reduction from baseline of 7.4 drinks per week compared to a reduction of 3.3 in the control group. This study also showed a reduction in rates of driving after drinking in the experimental group as compared to the control group.
SBIRT use in relation to other drugs has been studied less in the ED setting, although one RCT showed efficacy of brief intervention in marijuana users promoting abstinence.
INCORPORATING SCREENING AND BRIEF INTERVENTION INTO PRACTICE
Ideal screening tools in the ED are short, simple, and easily administered by a variety of providers. These should detect alcohol use disorders across the entire spectrum, from at-risk to dependent drinkers, as at-risk drinkers may benefit the most from intervention.
Brief interventions may include advice only or incorporate some motivational enhancement techniques. For the at-risk drinker or the patient who has sustained an alcohol-related injury but is not alcohol dependent, setting goals within safe limits, coupled with a referral to the patient’s primary care physician, may be all that is needed. For the patient with nondependent drug use, negotiating abstinence or harm reduction, such as no use while driving, and a referral to primary care may be sufficient. For the patient who is dependent on drugs or alcohol, when the clinician is uncertain as to where a patient fits on the continuum of alcohol and drug use disorders, the brief intervention becomes a negotiation process to seek further assessment or referral to a specialized treatment program.
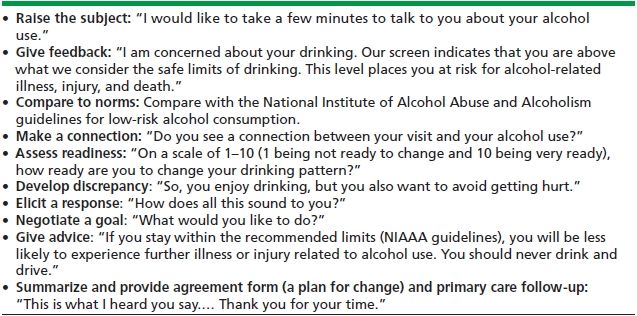
The contents of such a brief intervention are outlined in Table 81-1.
TABLE 81-1. BRIEF INTERVENTION FOR INJURED PATIENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


