David P. Gawronski
Trauma Surgery
Trauma is ranked as one of the foremost public health issues in the United States. Unintentional injury related to trauma is the fifth leading cause of death and the leading cause of death for people ages 1 to 44 years (Barclay, 2009). Whether the injury is a result of a motor vehicle collision, violence, crime, or is a work-related injury, trauma occurs unplanned and without warning. The unpredictable nature of trauma poses a major challenge to the perioperative nurse and the patient care team.
The potential for injury has existed since the beginning of humanity. Many of the major advances in care of critically injured patients have been accomplished through experience in the military. Clearly the shorter the response time, the greater the survival rate for casualties. This was demonstrated by the success of the mobile army surgical hospital (MASH) units during the Korean conflict and again during the Vietnam conflict; MASH brought the necessary supplies, equipment, and personnel closer to the battlefields and consequently improved patient outcomes.
Eventually this concept was applied to the civilian population and is commonly referred to as the “golden hour” of trauma care. More specifically, the golden hour refers to the time immediately after the injury when rapid and definitive interventions can be most effective in the reduction of morbidity and mortality. The golden hour starts at the scene, where prehospital personnel determine the severity of injury, initiate medical treatment, and identify the most appropriate facility to which to transport the patient. Traumatic deaths may occur in three phases, or timeframes. The first occurs immediately after the injury. In this phase, death is usually a result of lacerations to the heart or aorta or brainstem injury. These patients rarely survive transport to the hospital, and die at the scene. The second phase occurs within the first 1 to 2 hours after the injury. These patients have injuries to the spleen, liver, lung, or other organs that result in significant blood loss. This is the group in which definitive trauma care (i.e., appropriate and aggressive resuscitation with adequate volume replacement) may have the most significant effect (the golden hour). The third phase occurs days to weeks after the injury, often during the intensive care phase, and is usually caused by complications or a failure of multiple organ systems.
The wars in Iraq and Afghanistan have resulted in some changes in the way traumatic injuries are managed; the military has not set up convalescence centers as in Vietnam and Desert Storm. Rather, the doctrine of “essential care in theater” is followed. Physicians and nurses have been trained to provide immediate care, keeping in mind the treatment resources that will be available at the next level of care. Soldiers with upper body injuries are surviving because of body armor. However, there is no protection for upper extremities; therefore, many amputations are performed, including above-elbow and shoulder disarticulations. The new philosophy is to stress continuity of care with the goal of returning the soldier to the highest possible level of function.
Time is of the essence in providing definitive care to the critically injured person. A significant number of patient deaths can be prevented if rapid transport is provided from the scene to a facility equipped to provide resuscitation and treatment in an efficient and timely manner. This concept is reflected in the national development of the emergency medical services (EMS) system. Facilities and resources are allocated and coordinated to provide specific interventions for a group of patients. For example, facilities that meet certain criteria to accommodate the specialized needs of the critically injured patient are designated as trauma centers. Communities establish transfer and triage protocols that allow for a trauma patient to reach the appropriate facility with the least out-of-hospital time possible. This may be accomplished by a helicopter with a specially trained flight crew or by the use of ground transport with an advanced life support (ALS) ambulance team (Figure 28-1).
Trauma centers (TCs) are classified based on the scope of available services and resources. A level I TC is capable of providing total care for every type of injury. Accepting this designation commits the TC to providing qualified personnel and equipment necessary for rapid diagnosis and treatment on a 24-hour basis. A level II TC provides comprehensive care for all injuries but lacks some of the specialized clinicians and resources required for the level I designation. A level II facility may provide surgical intervention if the critical nature of the injury dictates immediate intervention before transfer to a level I facility. A level III facility provides prompt evaluation, resuscitation, emergency surgery, and stabilization, as needed, before transfer to a higher-level facility. The American College of Surgeons (ACS) recommends that in level II and III centers, an operating room (OR) team be readily available at all times. Depending on the population served and the volume of urgent cases, this requirement may be met with on-call staff. A level IV trauma center has the ability to provide advanced trauma life support before patient transfer. These facilities may be located in rural areas with limited access and may be a clinic or a hospital.
Although the risk for death is 25% lower for a severe injury treated in a level I TC (Barclay, 2009), not all patients require the services of a level I TC and thus may be transported to the closest emergency department (ED) for care. New guidelines and recommendations for triage, first developed as a position statement by the ACS in 1986, have been published (Barclay, 2009). Known as the Decision Scheme, this algorithm guides EMS personnel through the following four decision points: physiologic parameters, anatomic parameters, mechanism of injury (MOI), and other special considerations. Personnel review physiologic parameters. Patients with a Glasgow Coma Scale (see Table 21-2) score less than 14, systolic blood pressure less than 90 mm Hg, or respiratory rate less than 10 breaths per minute or greater than 29 breaths per minute should be transported to the highest level facility available. The anatomic parameters include specific types of injuries, such as penetrating injuries of the neck or torso, flail chest, or proximal long bone fracture; these patients are also transported to the highest level facility available. The MOI and other special considerations, such as age or prior medical history, are also reviewed to determine to what level facility the patient is transported.
Trauma patients require immediate access to the OR 24 hours per day, 365 days per year. A sudden influx of a large number of trauma patients to a trauma center may necessitate triage or classification of those less seriously injured as less urgent, allowing immediate access for the critically injured patients. The elective surgery schedule may need to be interrupted to expedite care for the trauma patient or patients. Scheduling policies and procedures are established collaboratively by the departments of surgery, trauma, anesthesia, and perioperative nursing services. Consequently, the perioperative nurse and scrub person (who may be a registered nurse or surgical technologist) need to be familiar with supplies and equipment located in the OR designated for trauma or in the ORs that are used most frequently for these patients.
Perioperative Nursing Considerations
Preliminary Evaluation: Mechanism of Injury
Because of the unpredictable timing of trauma, it is often the on-call perioperative nursing team who cares for injured patients requiring surgical intervention. In contrast to an elective surgical procedure, little information may be known about trauma patients and preparation time is often abbreviated. A working knowledge of the MOI is essential to assist the perioperative nurse in rapid patient assessment.
MOI, or kinematics, involves the action of forces on the human body and their effects. Knowing the forces applied provides valuable information in evaluation of the patient and injuries that may be present. The first EMS team to respond to the scene of an injury must carefully evaluate the patient in relation to the MOI. For example, the position of the victim in a car, whether the person was the driver or a passenger seated in the back seat or front seat, estimated velocity of the vehicle, location of impact, and use of a seat belt or air bag are all pieces of information used to determine the index of suspicion about the probable causes of injuries to the patient. After immediate threats to life are addressed, the MOI can provide valuable clues as to probable cause of injuries. This systematic approach can reduce morbidity and mortality (Table 28-1).
TABLE 28-1
| Mechanisms of Injury | Phases of Injury |
| Vehicle of transfer of energy from environment to human host | Examples |
| Falls | |
| Motor vehicle collisions | |
| Bullets | |
| Stabbing instruments | |
| Blasts/bombs | |
| Deceleration Forces | |
| Decrease in speed of a moving object or person | External Forces |
| Victim strikes steering column | |
| Victim impacts ground | |
| Acceleration Forces | |
| Increase in speed of a moving object or person | Pedestrian thrown when struck by moving vehicle |
| Blast Forces | |
| Heat, light, pressure | Bomb explosion |
| Low- and high-velocity missiles | Bullets |
| Stabbing instruments | |
| Human body’s response to kinetic energy load | Internal Forces |
| Stress | |
| Cells separate, stretch, compress, or shear | |
| Strain | |
| Tissue damage or deformation from stress | |
| Describing for clinical and diagnostic purpose | Types of Injuries |
| Blunt vs. penetrating | |
| Closed vs. open | |
| Primary vs. secondary | |
| Direct vs. indirect | |
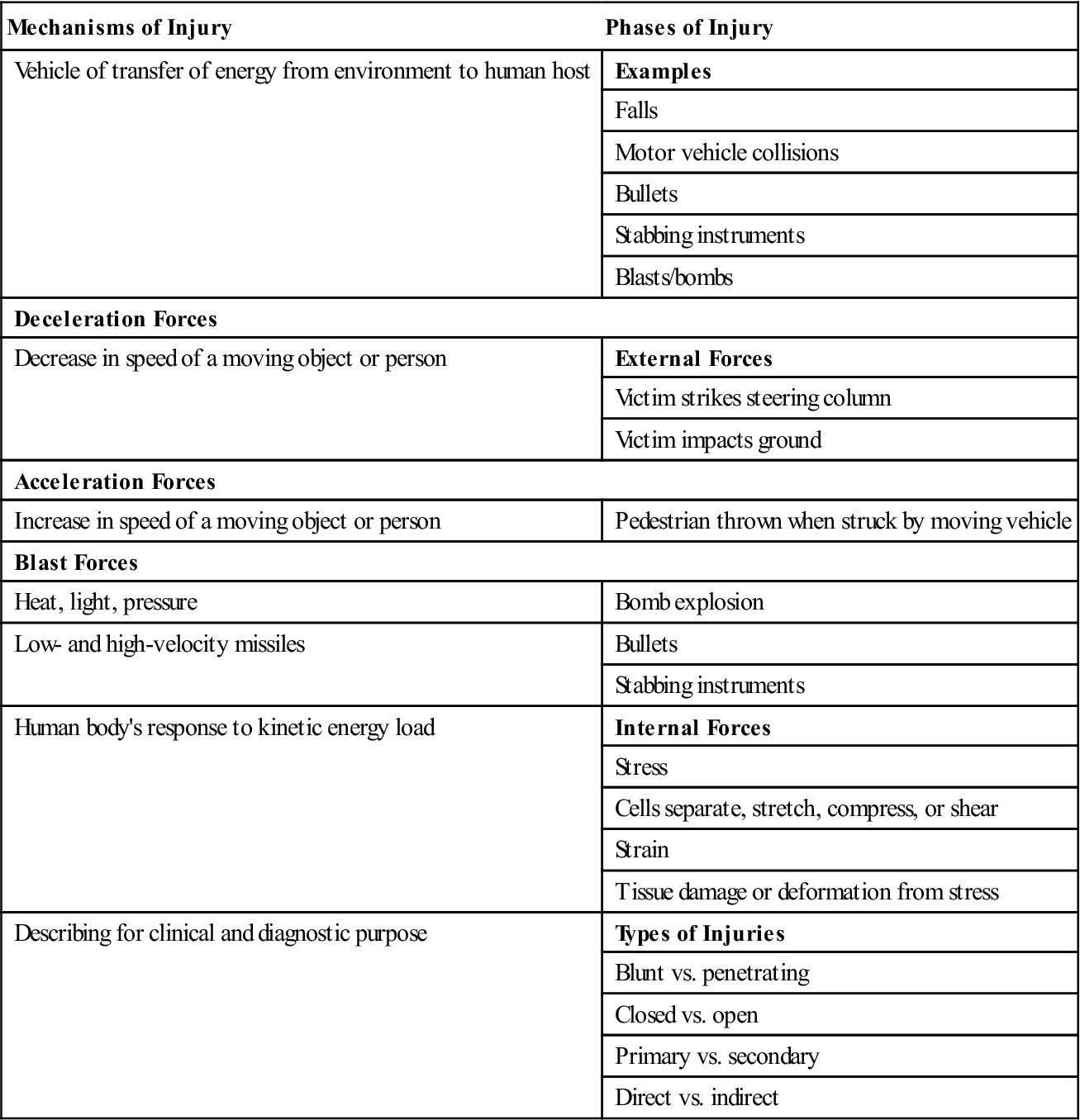
Modified from Emergency Nurses Association (ENA): Trauma nursing core course, ed 6, Des Plaines, IL, 2007, Author.
The MOI is a product of the type of injuring force and the resulting tissue response. The velocity of the collision, the shape of the object, and the tissue’s flexibility influence the magnitude of the injury sustained. For example, long bone tissue has little or no flexibility. A strong collision involving a long bone most often results in a fracture of some type. In contrast, soft tissue injury from a colliding force may result in a contusion because this tissue has greater flexibility.
Blunt trauma is injury resulting from a combination of forces, such as acceleration, deceleration, shearing, and compression that do not result in a break of the skin. Morbidity and mortality may be greater than with penetrating trauma because identification of injuries is more difficult when injuries are less obvious. Causes of blunt trauma include motor vehicle collisions (MVCs), contact sports injuries, aggravated assault, and falls. Even low-energy trauma, such as that associated with low-level falls, can produce significant injuries.
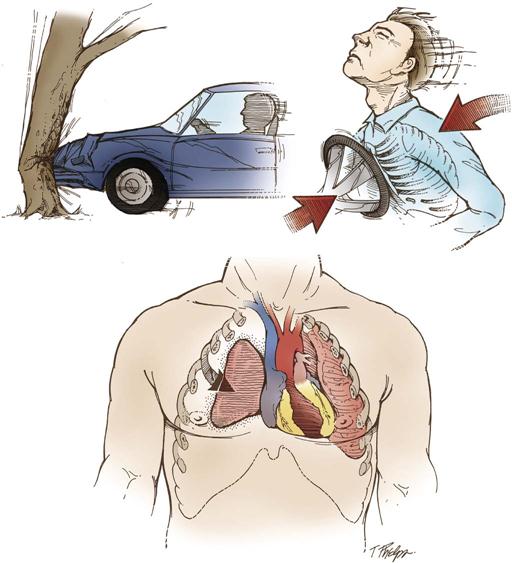
Acceleration and deceleration injuries occur most frequently in blunt trauma. A ruptured thoracic aorta is an example of an injury that occurs as a result of these types of forces. In an MVC the large vessels are stopped or decelerated rapidly, resulting in vessel damage caused by stretching that exceeds the vessel’s elastic ability. This affects the aorta at the ligamentum arteriosum, the anatomic point where it is affixed tightly to the chest wall, just below the origin of the subclavian artery. This shearing below the attachment site causes a rupture as the aorta continues to move in a forward motion after the chest wall motion has stopped.
MVCs account for a high degree of blunt trauma (Research Highlight). During an MVC, actually three collisions occur (Figure 28-2). The first collision is that of a car into another object. The second collision is the impact of the occupant’s body on the vehicle’s interior. The third collision occurs when an internal body structure hits a rigid bony surface. A coup-contrecoup injury of the brain, for example, is the result of an acceleration force to one area of the brain and a deceleration force to an opposite area. Front and side air bag deployment along with the use of seat belts can decrease the severity of traumatic injury.
Falls also cause a significant number of traumatic deaths in the United States. Injuries are most commonly associated with children experiencing falls more than twice their height. In adults, falls more than 10 to 15 feet are usually accompanied by significant injury. Deceleration forces in falls produce forces of stretching, shearing, and compression. Consequently, aortic injuries are also suspect in this group of patients. Skeletal injuries occur as well, because of the compressive forces present.
Penetrating trauma is a result of the passage of a foreign object through tissue. The degree or extent of tissue injury is a function of the energy that is dissipated to the tissue and the surrounding areas. The anatomic structures most often injured include the liver, intestines, and vascular system. The extent of the injury relates to the nature of the foreign object (e.g., bullet caliber, knife size), distance from the weapon, structures penetrated, and amount of energy dissipated to the structures.
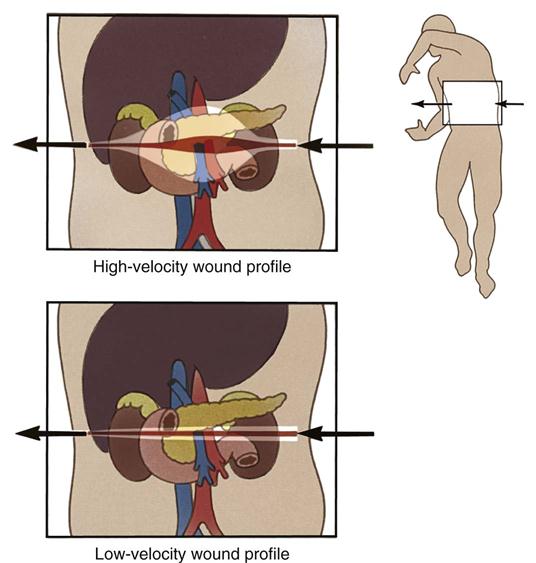
The velocity of a bullet is responsible for the degree of injury or cavitation to the tissue. A low-velocity bullet is one that travels at a lower speed (1000 feet per second or less) and disrupts only the bullet tract and its immediate surrounding area. A high-velocity weapon, such as used by the military, fires a bullet traveling at a greater speed (3000 feet or more per second) and causes significantly more damage and tissue destruction because the bullet tract involves more extensive surrounding tissue (Figure 28-3). The distance from the weapon also influences the degree of injury because the velocity is greatest when the bullet leaves the weapon and decreases as it travels. In addition, the type of bullet (e.g., shotgun shells with multiple pellets and hollow-point bullets, which mushroom on impact) influences the degree of injury. Commonly the entrance wound is smaller than the exit wound because of the dissipation of energy, but an exit wound may not always be present. If the bullet completely fragments or is lodged in an internal structure, there will not be an exit wound. Depending on the position of the bullet and any injury that could be caused by attempting to remove it, bullets are not always removed.
Stab and impalement wounds are considered to be low-velocity wounds. The associated injuries usually correspond to the path of the penetrating object. Factors such as the object’s width and length assist in identifying the possible occurrence of injuries. A single injury site may penetrate several different organs or cavities. Penetrating injuries located at or below the nipple line may cause both chest and abdominal injuries. This is attributable to the diaphragmatic excursion that occurs with inspiration and expiration. Impaled objects should not be removed at the scene or in the ED. The impaled object provides a tamponade effect to injured blood vessels and is removed only when the ability to control potential bleeding from those vessels is present. Wound debridement may also be necessary. Therefore, these objects are removed in the OR, where the needed supplies and instrumentation are located.
Injuries that result from explosions are related to the effects of the blast. With the threat of domestic terrorism on the rise, the treatment of blast victims may become more frequent in trauma settings. Blast injuries are capable of inflicting a variety of injuries. Primary blast injury is the result of a direct pressure wave on the body, most likely to affect the lungs, gastrointestinal (GI) tract, tympanic membrane, or blood vessels. Secondary blast injuries are often present as penetrating organ injury and result from airborne shrapnel and debris. Tertiary injuries result from the blast wind moving bodies and debris (Kumar, 2010). The type of injury sustained and its intensity are directly related to factors such as the size of the blast and the proximity of the victim or victims. Patients from a blast explosion may present with penetrating injury, contusions, lacerations, amputations, abrasions, avulsions, evisceration, and various degrees of burns (Table 28-2).
TABLE 28-2
| Category | Areas Affected | Types of Injuries |
| Primary: Caused by blast itself | Gas-filled organs most susceptible: | |
| • Eye | Rupture of globe | |
| • Middle ear/tympanic membrane | Rupture and permanent deafness possible | |
| • Lungs | Pneumothorax, alveolar rupture, air embolus | |
| • GI tract | Abdominal hemorrhage, contusions, rupture | |
| • Central nervous system | Diffuse cerebral hemorrhage, cerebral air embolism, concussion syndrome (injury without physical signs) | |
| Secondary: Caused by debris and projectiles | Any body part | Varies depending on size of projectiles: penetrating or blunt injury |
| Tertiary: Caused by victim being thrown against stationary objects | Any body part | Similar to those seen in motor vehicle collisions: fractures, traumatic amputations, closed/open brain injury |
| Quaternary: Exacerbation or complications of existing conditions | Any body part | Burns, crush injuries, inhalation of dust or toxic gases causing exacerbation of asthma or COPD, angina |
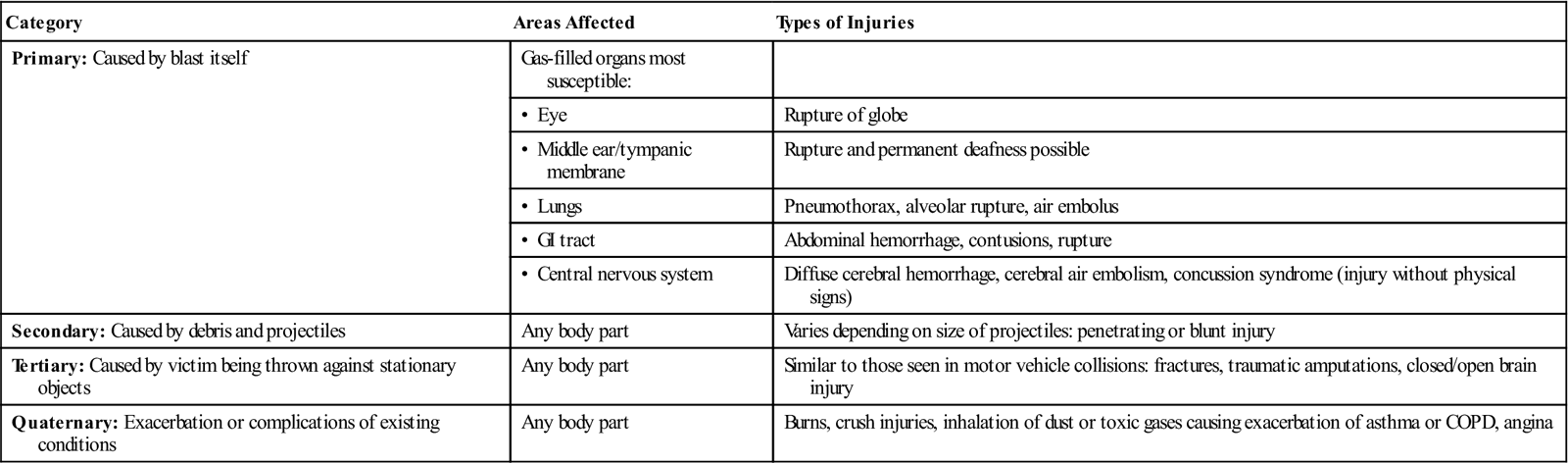
COPD, Chronic obstructive pulmonary disease; GI, gastrointestinal.
Modified from Emergency Nurses Association (ENA): Trauma nursing core course, ed 6, Des Plaines, IL, 2007, Author.
Thermal and electrical tissue damage and inhalation injuries may occur from an explosion or as a sole mechanism of injury. These patients are usually resuscitated and require operative intervention for debridement on a nonemergent basis, unless the injury is limb- or life-threatening.
Injuries can be scored objectively according to their severity. This scoring system assists medical personnel in more effective triage and provides a universal method of communication among facilities, departments, and nursing personnel. The ACS guidelines, as published by the National Expert Panel on Field Triage, now recommend the use of the Decision Scheme (Table 28-3).
TABLE 28-3
Decision Scheme Recommendations*
| Steps | Transition | Recommendations |
| Step 1 | Transport to TC for any of the following: GCS <14, systolic BP <90 mm Hg, respiratory rate <10 or >29 breaths/min | |
| 1 to 2 | These patients have potentially serious injuries and should be transported to highest level TC available | |
| Step 2 | Transport to TC for any of the following: penetrating injuries of head, neck, torso, and extremities proximal to elbow and knee; flail chest; 2 or more proximal long bone fractures; crushed, degloved, or mangled extremity; amputation proximal to wrist and ankle; pelvic fracture; open or depressed skull fracture; paralysis | |
| 2 to 3 | If yes to any criteria, transport to highest level TC available; if patient does not meet step 2 criteria, proceed to step 3 | |
| Step 3 | Transport to TC for any of the following: falls >20 feet for adults, >10 feet or 2-3 times child’s height; motor vehicle collision with partial or complete ejection of occupant; auto vs. pedestrian/bicyclist thrown; motorcycle crash at speeds >20 mph | |
| 3 to 4 | If yes to any criteria, transport to closest TC | |
| Step 4 | Consider transport to TC for the following: age >55 or <15, anticoagulation and bleeding disorders, burns, time-sensitive extremity injury, end-stage renal disease requiring dialysis, pregnancy, or provider judgment |
BP, Blood pressure; GCS, Glasgow Coma Scale; TC, trauma center.
*The Decision Scheme is an essential component of the trauma system, guiding EMS providers in transporting injured patients to the most appropriate facility, ensuring proper treatment, and thus reducing death and disability.
Modified from Barclay L: Guidelines issued for field triage of injured patients, Medscape Medical News, 2009, available at www.medscape.org/viewarticle/587385. Accessed October 20, 2012.
Assessment
The resuscitative process begins with arrival of emergency personnel on the scene and ends when the patient has been stabilized, received definitive care, and undergone a complete and thorough physical examination to determine all injuries sustained. When the patient arrives in the ED, the trauma team initiates a primary assessment and secondary assessment. This is a logical, orderly process of patient assessment for potential life threats. These assessment activities are based on established protocols for advanced trauma life support (ATLS). The mnemonic used for the primary assessment is “ABCDE,” representing assessment of the following:
• Airway (with cervical spine precautions)
• Disability (brief neurologic examination)
• Exposure (to reveal all life-threatening injuries) and environmental control (thermoregulation)
Airway interventions may include manual maneuvers (chin-lift, jaw-thrust), insertion of oral or nasopharyngeal airways, or intubation. The trauma team may also perform emergent procedures, such as tracheotomy or needle cricothyrotomy, to secure the patient’s airway. Pulse oximetry and capnography monitoring are used. If cervical spine precautions were not implemented before arrival at the hospital, the team initiates them before performing any other procedures on the patient. A trauma team member can stabilize the head and neck, if necessary, until a cervical collar is placed. Once placed, the team does not remove it until an examination and cervical radiograph confirms there is no neck injury.
During this time, the surgeon or ED physician and trauma team identify and correct life threats that are present before progressing to the next part of the examination. A patient requiring immediate surgery is transported to the OR, undergoes surgical intervention, and then is transferred to the postanesthesia care unit (PACU) or intensive care unit (ICU), depending on his or her condition. On the other hand, a patient may have a penetrating wound with evisceration of abdominal contents. However, correcting the obvious defect, which is currently not life-threatening, is postponed until the trauma team is assured that the patient has a patent airway and an effective breathing pattern and cervical spine precautions have been implemented. An evisceration needs to be corrected, but an inadequate airway is an immediate life threat and assumes priority.
Depending on the patient’s injury, the surgeon may order an arterial blood gas (ABG) measurement. This test provides an accurate assessment of the ventilatory status of the patient and evaluates resuscitative airway and breathing interventions. Metabolic acidosis or a large base deficit (pH <7.35 or >7.45), with all other causes ruled out, may indicate internal bleeding. The surgeon may check for coagulopathy using thromboelastography (TEG). Rapid TEG testing can provide valuable information about the depleted component within the clotting cascade, allowing for direct therapy to correct the coagulopathy (Jeger et al, 2009).
After the trauma team completes the primary assessment and corrects any immediate life threats, they perform a secondary assessment. The purpose of the secondary assessment is to identify all injuries present. Sometimes the secondary assessment may be completed by the perioperative nurse, the PACU nurse, or the critical care nurse. The mnemonic used for the secondary assessment is “FGHI,” representing assessment of the following:
This assessment begins with a full set of vital signs, including a rectal or tympanic temperature, unless contraindicated, and placement of noninvasive monitoring devices. Often during resuscitation the nurse will insert a Foley catheter to monitor urine output and fluid resuscitation efforts. The nurse should inspect the urinary meatus for the presence of blood before inserting the catheter. If blood is noted, the nurse notifies the surgeon and does not insert the catheter. The patient may have a ruptured bladder or a urethral injury, either of which is commonly associated with a fracture of the pelvis. The surgeon may wish to perform a retrograde urethrogram to examine the bladder and urethra for the presence of tears or disruption. After catheter insertion, urine is obtained for a urinalysis and urine drug screen. The identification of specific drugs in the urine may assist in further diagnosis and treatment. The urine will also be tested to determine the presence of red blood cells (RBCs). Depending on the amount of hematuria present, a renal contusion or other renal injury may be present. In addition, a nasogastric tube may be inserted at this time. The nurse prepares to provide comfort measures by assessing the patient’s pain by using a pain scale (if indicated, orders for pain medication should be obtained).
The history and past medical history begin with information generated from the patient; if the patient is unable to provide the history, the team obtains the information from the family or significant others when possible (Emergency Nurses Association [ENA], 2007). This history is referred to as the “AMPLE” history and may be obtained even after the patient is transferred to the OR by the ED personnel. The history includes the following:
If the history is obtained after the initiation of surgery, it is important to communicate it to the surgeon and the anesthesia providers.
The head-to-toe evaluation of the patient—inspection, palpation, percussion, and auscultation—is used in the complete head-to-toe assessment to reveal any deformities, open injuries, tenderness, or swelling. The assessment begins at the head and face and then moves to the neck (including the spine), the chest, the abdomen, and the pelvis. The four extremities are next; distal pulses, motor function, and sensation are assessed. The final check is the back; the patient is carefully log-rolled to the side for a full visual and tactile assessment (Evidence for Practice).
Routine Laboratory Tests.
Laboratory values aid the trauma team in evaluating the patient’s status (see Appendix A). Appropriate laboratory tests include a minimum of a complete blood count (CBC), hemoglobin and hematocrit (H&H) value, blood alcohol level (BAL), and a blood type and screen; other tests may be requested during evaluation. The results of the laboratory studies should be reviewed and communicated as appropriate. An abnormal level of RBCs may signify dehydration, hypovolemia, or fluid overload (dilutional). An elevated white blood cell (WBC) count, indicating the presence of infection, may be related to inflammation, tissue necrosis, or immunocompromise. H&H values also are important to note. Caution is recommended when evaluating an H&H drawn in the ED. The time delay between bleeding and a drop in the H&H value can be significant. It is only after hemodilution occurs (from shock compensation or crystalloid replacement) that hematocrit level drops. Frequently, abnormal values in the patient with blunt trauma alert the team to the possibility of internal bleeding.
BAL also assists the trauma team in their evaluation. If the patient’s level is significantly high, the physical examination and response may be unreliable. In addition, the neurologic status of patients with high BALs is very difficult to assess. Abnormal clotting studies are of obvious significance in trauma patients. These results may be attributable to anticoagulant medication the patient is taking or the effects of profound hypothermia. Clotting times may also be prolonged in the presence of excessive alcohol ingestion or the use of anabolic steroids. Clotting times may decrease with the use of antihistamines and diuretics.
A blood type and screen shortens the time needed by the blood bank to obtain a crossmatch, if needed later. Most trauma centers have several units of type O-negative blood (universal donor) available in the event that a blood transfusion is required before a type and crossmatch (T&C) can be performed. Because of regional shortages of O-negative blood, O-positive blood can be used in male patients and adult female patients of non-childbearing age. Initially, trauma patients are fluid-resuscitated with warmed crystalloid solutions, such as lactated Ringer’s solution or normal saline solution. If the patient’s blood pressure responds, the diagnostic examination continues. However, if the hypotension returns, blood transfusions may be initiated and the patient may be transported immediately to the OR for exploratory surgery.
Many trauma centers are implementing massive transfusion policies for the clinical management of patients experiencing massive hemorrhage and to coordinate interdisciplinary and interdepartmental resources. Massive transfusion is defined as the replacement of one or more blood volumes within a 24-hour period, or 50% of estimated blood volume in 3 hours or less (Nessen et al, 2008). This volume is approximately equal to the transfusion of 10 units of RBCs. Transfusion guidelines recommend a balanced administration of blood products. Replacing a patient’s circulating volume with packed RBC/plasma/platelet ratios of 1 : 1 : 1 improves outcomes by preventing and treating coagulopathy due to massive hemorrhage (Johansson et al, 2012). This simple ratio not only is easy to use but also has the benefit of administration of higher plasma and platelet volumes.
Diagnostic Procedures
Radiology.
Depending on the trauma center protocol, a blunt trauma radiographic series may be ordered during the resuscitative phase. The series minimally includes a lateral view of the cervical spine and an anteroposterior (AP) view of the chest. In addition, the patient also undergoes lateral thoracic and lumbar spine films and an AP view of the pelvis. Any area with deformity, swelling, or pain may also be examined by x-ray. Trauma patients are always treated as if they have a cervical spine injury until proven otherwise. When reviewing the cervical spine films for cervical spine injury clearance, the clinician should consider any existing factors that place the patient at high risk for spine injury. These include age older than 65 years, a dangerous MOI, and paresthesias in the extremities. Patients with penetrating trauma injuries usually are transferred immediately to the OR for exploratory laparotomy.
If the resources are available, the trauma center protocol may also include a computed tomography (CT) scan as a diagnostic or screening tool. Depending on the MOI, such as a fall, CT scans of the head and abdomen may be performed. Because injuries in blunt trauma are very difficult to diagnose, the CT scan is frequently done before patient transfer to the OR. A high index of suspicion is maintained for other injuries until proven otherwise. Bowel injuries may be missed during initial scanning. A CT scan of the brain revealing an injury incompatible with life may alter the course of definitive treatment for a patient.
A CT-angiogram may be indicated in diagnosis of vascular injuries. If the patient is hemodynamically stable, this test is of great value in determining the extent of the injury. It is particularly beneficial in the diagnosis of a ruptured thoracic aorta, in which extravasation of the dye at the area of aortic fixation to the chest wall is noted. Other uses include evaluation of penetrating wounds, especially in the extremity. Vessel injury can be noted and the need for surgical intervention determined.
Other Diagnostic Tests.
Cardiac monitoring is another component of the initial phase of trauma care and is particularly important in blunt trauma. Early detection of ventricular dysrhythmias may indicate a myocardial contusion, or bruising of the heart. An electrocardiogram (ECG) is obtained when indicated by the mechanism of injury or the patient’s symptoms. Undiagnosed heart disease, as evidenced by an abnormal ECG, is noteworthy in a patient requiring operative intervention.
Focused assessment with sonography in trauma (FAST) may assist with diagnosis in difficult situations. FAST is a portable, noninvasive scan that can determine the presence of free fluid in the chest or abdomen. The typical FAST scan consists of chest, pelvic, and four abdominal scans. The chest scan examines right and left chest views and can determine the presence of pericardial fluid. The upper right abdominal scan evaluates the hepatorenal area, the first area that shows the presence of air. The left upper scan examines the splenorenal area. The left and right paracolic gutters are also scanned. The pelvic scan assesses for free fluid near the bladder. FAST is also used in pregnant patients with blunt abdominal trauma; it is both faster and safer than a CT scan, which is contraindicated in the pregnant patient because of the use of iodinated contrast medium and ionizing radiation (Cunningham, 2008).
Although FAST is useful in diagnosing free fluid, it cannot determine damage to solid organs; therefore, it complements rather than replaces other imaging scans. Diagnostic peritoneal lavage (DPL) may be performed to determine the presence of abdominal injury. This tool is of particular benefit when evaluation of the abdomen is difficult, such as when the patient is intoxicated, unconscious, or hemodynamically unstable. DPL can be performed in the ED, OR, PACU, or ICU. Nonetheless, retroperitoneal blood may be missed with a DPL, whereas the FAST approach may be quicker and visualize more structures, even pericardium; it is also less expensive and noninvasive. Thus FAST may be used with patients who are unstable and need a quick approach without the risk of a false-positive tap (Table 28-4).
TABLE 28-4
Comparison of DPL, FAST, and CT Scans
| Diagnostic Peritoneal Lavage (DPL) Documents Bleeding | Focused Assessment with Sonography in Trauma (FAST) Documents Fluid | Computed Tomography (CT) Scan Documents Organ Injury |
| Advantages | ||
| Early diagnosis Performed rapidly 98% sensitive Detects bowel injury | Early diagnosis Noninvasive Performed rapidly 86%-97% accurate Repeatable | Most specific to injury 92% sensitive 98% accurate |
| Disadvantages | ||
| Invasive Low specificity Misses diaphragmatic and retroperitoneal injuries | Operator dependent Bowel gas and subcutaneous air distortion Misses diaphragm, bowel, and pancreatic injuries | Increased cost and time Misses diaphragm, bowel, and some pancreatic injuries |
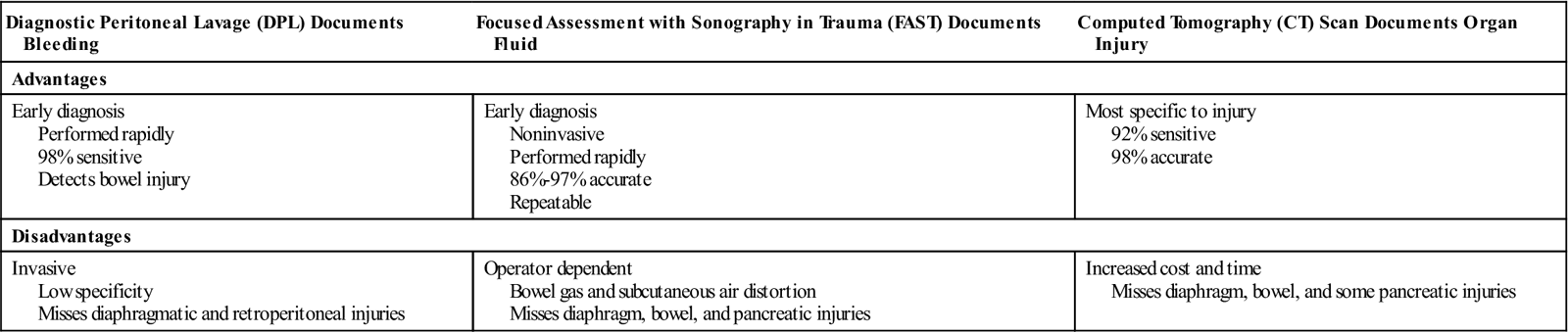
Modified from Emergency Nurses Association (ENA): Trauma nursing core course, ed 6, Des Plaines, IL, 2007, Author.
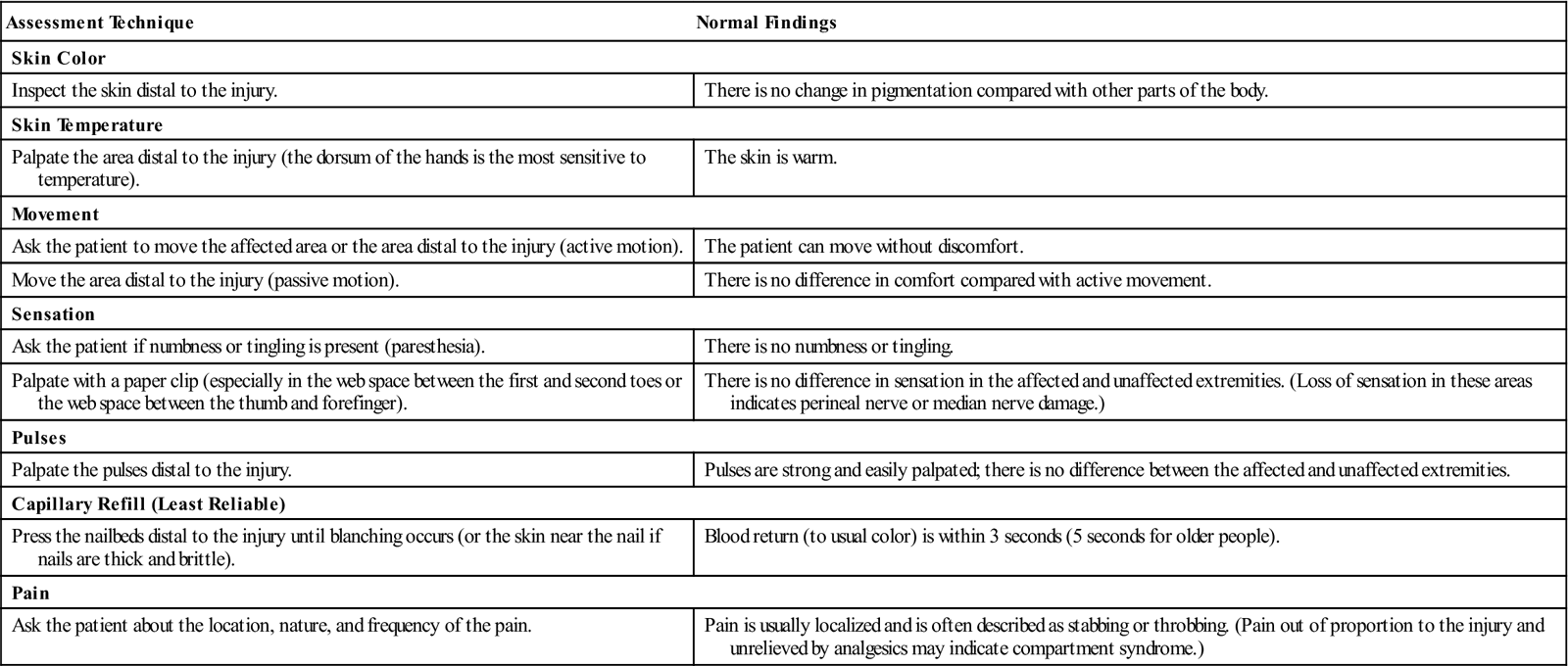
Internal compartment pressures may be measured with an injury to the extremity as well as to the abdomen. Swelling of the muscles below the fascia covering may compromise circulation and result in the eventual loss of the extremity because of tissue necrosis. This is known as compartment syndrome. There are multiple compartments in the lower extremity that may be affected (Figure 28-4). Surgeons may measure compartment pressures with a manometer/stopcock/syringe or a commercial compartment pressure–measuring device. Normal compartmental pressures are less than 20 mm Hg. Pressures more than 30 mm Hg require a fasciotomy. Symptoms include severe pain, paresthesia, and a decrease in motor movement in the involved extremity, especially on passive movement (Table 28-5).
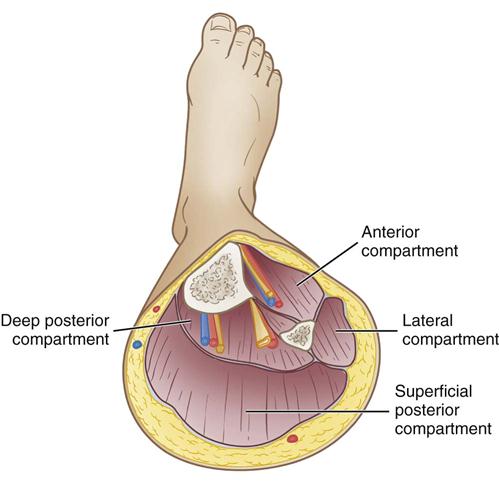
TABLE 28-5
Signs and Symptoms Associated with Compartmental Syndromes
| Compartment | Location of Sensory Changes | Movement Weakened | Painful Passive Movement | Location of Pain or Tenseness |
| Lower Leg | ||||
| Anterior | First web space | Toe extension | Toe flexion | Along lateral side of anterior tibia |
| Lateral | Dorsum (top) of foot | Foot eversion | Foot inversion | Lateral lower leg |
| Superficial posterior | None | Foot plantar flexion | Foot dorsiflexion | Calf |
| Deep posterior | Sole of foot | Toe flexion | Toe extension | Deep calf—palpable between Achilles tendon and medial malleoli |
| Forearm | ||||
| Volar | Volar (palmar) aspect of fingers | Wrist and finger flexion | Wrist and finger extension | Volar forearm |
| Dorsal | None | Wrist and finger extension | Wrist and finger flexion | Dorsal forearm |
| Hand | ||||
| Intraosseous | None | Finger adduction and abduction | Finger adduction and abduction | Between metacarpals on dorsum of hand |
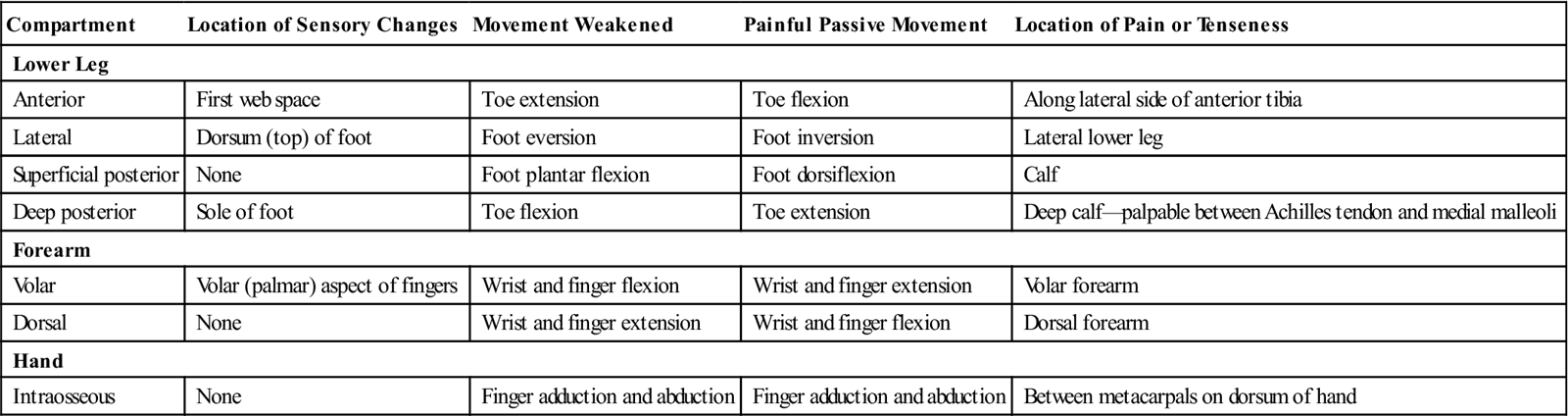
Modified from Warme WW, Matsen FA: Compartmental syndromes, 2011, available at www.orthop.washington.edu/?q=patient-care/articles/shoulder/compartmental-syndromes.html. Accessed November 3, 2012.
Massive intestinal edema may occur with trauma patients, causing compromise to internal organs and development of a different type of compartment syndrome. Abdominal compartment syndrome, also called abdominal hypertension, is characterized by increased intra-abdominal pressure (IAP). An increase in IAP can have a negative effect on the respiratory, splanchnic, and cerebral functions. It contributes to sepsis or multiple organ failure seen in many trauma patients. Normal IAP is approximately 5 to 7 mm Hg; elevation to 25 mm Hg is often seen in patients with septic shock and correlates with high mortality (Vegar-Brozovic et al, 2008). IAP is graded from I to IV based on a 12 to more than 25 mm Hg scale. Adverse effects on organ function may manifest as decreased cardiac output, oliguria, and hypoxia. Elevated intrathoracic pressure reduces left ventricular compliance, causing limitations in effective ventilation, often requiring ventilator support. Elevated IAP may cause an increase in intracranial pressure related to obstruction of cerebral venous blood outflow and increased intrathoracic and central venous pressure. Delay in treatment of IAP may lead to brain deterioration and damage.
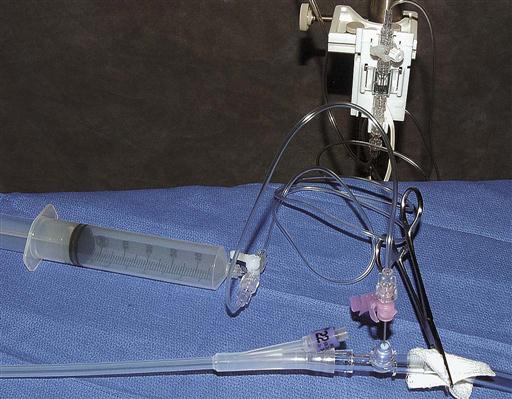
Management involves a decompressive laparotomy. After a decompression the greatest nursing priority is wound management. The swelling may render the abdomen difficult or impossible to close. If the abdomen is closed, IAP may rise to a level greater than 25 cm of H2O, at which point it may lead to significant organ dysfunction (Kulaylat and Dayton, 2012). IAP monitoring is accomplished with the use of a nasogastric tube in the stomach or a Foley catheter in the bladder. Simple water-column manometry is done at 2- to 4-hour intervals, although it is possible to connect a pressure transducer to a Foley catheter by way of the sampling port (Figure 28-5). By establishing a water column of urine in the Foley catheter with a clamp distal to the port, a pressure gradient is established. After zero-balancing the transducer, an 18-gauge needle is placed on the end of the pressure tubing and inserted into the sampling port. Using the pressure tubing and a 60-mL syringe, 50 to 60 mL of normal saline is then instilled into the Foley. On instillation of the saline, the waveform on the monitor is correlated to the existing bladder pressure. Normal IAP is zero, or subatmospheric. A pressure of more than 25 cm of H2O is considered diagnostic of abdominal compartment syndrome (Kulaylat and Dayton, 2012). Postoperatively these patients are susceptible to fluid and heat loss. Continuous hemodynamic monitoring is essential in the critical care phase of treatment.
Admission Assessment.
The perioperative nurse may not obtain information concerning the trauma patient until the patient arrives in the OR for surgical intervention. If the patient’s condition permits, the perioperative nurse should obtain a brief, precise report from the ED nurse that contains the following information: MOI, an AMPLE history (if available), condition on arrival (e.g., level of consciousness), availability of and prior administration of blood or blood products, spine clearance, injuries present, and any other pertinent information (e.g., family present, completion of secondary assessment). If the injury is life- or limb-threatening, implied surgical consent is assumed (i.e., if the patient were able, consent would be given).
Additional data are collected as the perioperative nurse accompanies the patient to the OR. The status of the airway, as well as breathing patterns and circulatory condition, can be observed. The ED record also provides information concerning amount and type of intravenous (IV) fluid received, vital signs, core temperature, and laboratory and other diagnostic examinations performed. A quick visual and physical survey of the patient when the perioperative nurse is preparing the patient for the procedure enables identification of other sites of injury that might require attention.
The patient’s psychologic status also can be assessed. If the patient is conscious, the perioperative nurse is challenged to allay fear and anxiety. The trauma patient has endured a very frightening experience and is in need of support. The perioperative nurse is often the best member of the surgical team to communicate with the patient and explain the interventions occurring before anesthesia induction. A touch or handhold is an important aspect of this communication process, demonstrating the nurse’s caring behaviors and offering comfort.
Nursing Diagnosis
Nursing diagnoses related to the care of trauma patients undergoing operative intervention might include the following:
Outcome Identification
Outcomes identified for the selected nursing diagnoses could be stated as follows:
Planning
Because of the unexpected nature of trauma, planning perioperative care is of the utmost importance. Equipment, instruments, and supplies that have a high probability of use must be immediately available. Autologous blood salvage units should also be considered during patient care preparation, because blood salvage will be done if not contraindicated by the nature of the injury. (A Sample Plan of Care for a trauma patient is shown on page 1113.)