Trauma
Trauma is one of the leading causes of death in the United States. Emergency trauma care basics include triage; assessing and maintaining airway, breathing, and circulation (the ABCs); protecting the cervical spine; assessing the level of consciousness (LOC); and, as needed, preparing the patient for transport and possibly surgery.
Common mechanisms of trauma include car, bicycle, and other vehicle accidents; carpedestrian accidents; drowning; firearms; burns; and falls.
TRIAGE: FIRST THINGS FIRST
Triage is the setting of medical priorities for emergency care by making sound, rapid assessments. The need for triage usually arises at the scene of injury and continues in the emergency department. Following health care facility protocol, you’ll decide which patient to treat first, which injury to treat first, how to best utilize other members of the medical team, and how to control patient and staff traffic.
In most cases, victims are assigned to the following categories:
emergent—life-threatening or limb-threatening injury requiring treatment within a few minutes to prevent death or further injury; includes patients with moderate to severe respiratory distress, cardiopulmonary arrest, compensated or uncompensated shock, limb injury with neurovascular compromise, alteration in neurologic status, and patients who have attempted suicide
urgent—serious, but not immediately lifethreatening injury that should receive treatment within 2 hours; includes patients with mild wheezing and mild or no respiratory distress, mild to moderate dehydration, and suspected forearm fracture (These patients require periodic assessment because they can deteriorate and become emergent.)
nonurgent—presence of minor or stable illness or injury that doesn’t require treatment within 2 hours; includes patients with ear discomfort, minor or isolated soft tissue wounds, and sore throat
During the assessment, if the patient is discovered to have a life-threatening condition, immediate intervention is needed. It may also be necessary to prioritize patients within the same triage category based on the severity of each patient’s symptoms.
Trauma care is very stressful. Often, you must deal with patients and families who are upset, angry, belligerent, intoxicated, or frightened; some may speak only a foreign language. Thus, you must work calmly and rationally, employing crisis-intervention techniques. You can help the patient a great deal by talking to him. Be sure to tell him what you’re going to do before you touch him. You must also handle difficult situations diplomatically and intelligently, recognize your limitations, and ask for help when you need it.
THE ABCS
Begin your care of an injured patient with a quick primary assessment of the ABCs. Also assess for disability and neurologic status.
To assess airway patency, routinely check for respiratory distress or signs of obstruction, such as stridor, choking, conversational dyspnea, or cyanosis. Be especially alert for respiratory distress in a patient who inhaled chemicals, was in a fire, or has upper body burns. If the airway is obstructed, remove vomitus, dentures, blood clots, or foreign bodies from the mouth.
In a semiconscious or unconscious patient, open the airway using a jaw-thrust maneuver. (Don’t use the head-tilt maneuver for a trauma patient. Suspect cervical spine injury until Xrays rule it out.) Then insert an oropharyngeal or nasopharyngeal airway. A nasopharyngeal airway is contraindicated in patients with massive facial trauma and those with possible basal skull fractures. Assist with endotracheal tube insertion as necessary. If rescue personnel have performed an alternate airway (AA) insertion, leave it in place until the patient has been tracheally intubated. This will prevent him from vomiting and possibly aspirating.
Next, make sure the patient’s breathing is adequate. Look, listen, and feel for respirations. If the patient isn’t breathing, call for help immediately, begin bag-valve-mask resuscitation, and prepare for intubation. Give supplemental oxygen; then draw samples for arterial blood gas measurement and calculate the supplemental oxygen’s effects to establish a baseline for oxygen and acid-base therapy. Multiple injuries create a need for supplemental oxygen because of blood loss and significant physiologic stress. A conscious multipleinjury patient usually displays compensatory hyperventilation. If he doesn’t, expect neurologic involvement or chest injury. Needle thoracentesis may be done to decompress tension pneumothorax.
To assess circulation, check for central and peripheral pulses, as well as capillary refill (which should be less than 2 seconds). If a carotid pulse is absent, institute cardiopulmonary
resuscitation. If external hemorrhage is evident, apply direct pressure to the bleeding site and, if the wound is on a limb, elevate it above heart level if possible. Apply a tourniquet only if the hemorrhage is life threatening.
resuscitation. If external hemorrhage is evident, apply direct pressure to the bleeding site and, if the wound is on a limb, elevate it above heart level if possible. Apply a tourniquet only if the hemorrhage is life threatening.
Managing tetanus prophylaxis
History of tetanus immunization (number of doses) | Tetanus-prone wounds | Non-tetanus-prone wounds | ||
T | TIG** | Tdap* | TIG | |
Uncertain | Yes | Yes | Yes | No |
0 to 1 | Yes | Yes | Yes | No |
2 | Yes | Yes | Yes | No |
3 or more | No (yes if more than 5 years since last dose) | No | No (yes if more than 10 years since last dose) | No |
* Tdap = Tetanus, diphtheria, and acellular pertussis, 0.5 ml. | ||||
Note: When Tdap and TIG are given concurrently, separate syringes and separate sites should be used. | ||||
Note: For children younger than age 7, tetanus and diphtheria toxoids and pertussis vaccine, adsorbed (DPT) are preferred over tetanus toxoid alone. If pertussis vaccine is contraindicated, administer tetanus and diphtheria toxoids, adsorbed (DT). | ||||
Monitor the patient’s vital signs even if he appears stable. Because vital signs can change rapidly, taking them serially can identify subtle and overt changes. Document baseline readings, and obtain new readings every 5 to 15 minutes until the patient is stable. Assess trends in vital sign readings to detect changes. Place him on a cardiac monitor and a pulse oximeter. Remember that the patient may have up to a 25% volume loss before it’s reflected in vital sign readings.
Draw blood for type and crossmatch, complete blood count, prothrombin time, partial thromboplastin time, platelet count, and routine blood studies, including amylase and lipase levels. Begin at least two I.V. lines with 14G or 16G catheters for fluid resuscitation with normal saline or lactated Ringer’s solution. Administer tetanus prophylaxis as needed. (See Managing tetan us prophylaxis.)
Immobilize the patient’s head and neck with a rigid cervical collar, supportive blocks, backboard, and tape, if this hasn’t been done. Obtain cervical spine X-rays as appropriate and rule out cervical spine injury before moving the patient again. Presume spinal injury and take precautions to prevent further injury, such as logrolling and using adequate staff to move the patient, until spinal injury has been ruled out.
Proceed with assessment of the patient’s disability; assess the patient’s LOC and pupillary and motor response to check the patient’s neurologic status. Attempt to establish the patient’s Glasgow Coma Scale rating. Report decorticate or decerebrate responses immediately. The patient need not have a head injury to exhibit an abnormal neurologic response. Any injury that impairs ventilation or perfusion can cause cerebral edema and raise intracranial pressure.
EXPOSE THE PATIENT FOR SECONDARY ASSESSMENT
Secondary assessment includes removal of the patient’s clothes to enable a more thorough examination. The clothing is placed in bags, which are labeled with the patient’s name and the date and time that he was brought to your facility. The bag will be given to the patient’s family or to the authorities if an investigation into the circumstances of the trauma is necessary. If the clothing must be given to the authorities, document having done so. Institute environmental controls by providing warming measures, such as warming blankets and units, warmed oxygen and I.V. solutions, and increased environmental temperature.
Assess the patient’s vital signs, and inform the patient’s family of his status. They can help to provide his history, especially his immunization status. Assess the need for comfort
measures; pain medication may be given as appropriate, and other techniques may be used to make the patient comfortable.
measures; pain medication may be given as appropriate, and other techniques may be used to make the patient comfortable.
Head-to-toe assessment
Secondary assessment also includes a thorough head-to-toe assessment of the patient. Quickly and carefully look for multiple injuries by systematically examining the patient. If you detect no spinal injury, carefully logroll the patient over to inspect his back for other wounds.
In chest trauma, assess for open wounds, tension pneumothorax, hemothorax, cardiac tamponade, bruises and hematomas, flail chest, tracheal deviation, and fractured larynx. Cover open wounds, and apply direct pressure to the wound as necessary. Be ready to assist with insertion of chest tubes, pericardiocentesis, cricothyrotomy, or tracheotomy, as appropriate.
Insert an indwelling urinary catheter and a nasogastric tube, and give prophylactic antibiotics and immunizations, as indicated. Appropriate diagnostic studies—such as X-rays, computed tomography (CT) scans, peritoneal lavage, magnetic resonance imaging (MRI), and excretory urography—may be performed based on assessment findings and patient stabilization. Notify medical or surgical specialists, as appropriate.
STABILIZE THE PATIENT
Because severe injuries commonly lead to shock, check skin temperature, color, and moisture. To control shock, administer I.V. fluids (lactated Ringer’s or normal saline solution) followed by blood or blood products.
In all cases of massive external bleeding or suspected internal bleeding, watch for hypovolemia and estimate blood loss. Remember, however, that a blood loss of 500 to 1,000 ml might not change systolic blood pressure but may elevate the pulse rate. However, bradycardia may be an ominous sign and a late finding of hemorrhagic shock. Stay alert for signs of occult bleeding, which commonly occurs in the chest, abdomen, and thigh. Repeat abdominal examinations frequently to assess the patient for abdominal distention; this could be a sign of internal injuries and bleeding.
Increased diameter of the legs or abdomen usually means that blood has leaked into these tissues (as much as 4,000 ml into the abdomen, 3,000 ml into the chest, and 2,000 ml into a thigh). Such blood loss will induce signs of hypovolemic shock (tachycardia, tachypnea, hypotension, restlessness, decreased urine output, delayed capillary refill, and cold, clammy skin).
If the patient has renal injuries or a fractured pelvis, look for the classic sign of retroperitoneal hematoma—numbness or pain in the leg on the affected side as a result of pressure on the lateral femoral cutaneous nerve in L1 to L3. Retroperitoneal bleeding may not cause abdominal tenderness. If the patient shows clinical signs of hypovolemia, immediately begin I.V. therapy with two or more large-bore catheters, and regulate fluids according to the severity of the hypovolemia. Although the initial resuscitation fluids are crystalloids, significant hypovolemia caused by hemorrhage requires blood transfusion. Assist with insertion of a central venous pressure or pulmonary artery catheter to monitor circulating blood volume.
If spinal trauma is suspected, methylprednisolone may be given I.V. If head trauma is present, the patient may be given emergency medication, such as mannitol, and ventilation may be controlled. The patient may also require emergency surgery—either exploratory or lifesaving—to help with stabilization, depending on the injury’s type and extent.
Limb fractures can be a source of blood loss. Look for limb fractures and dislocations. Check circulation and neurovascular status distal to the injury by palpating pulses distal to the injury and looking for the classic signs of arterial insufficiency: decreased or absent pulse, pallor, paresthesia, pain, and paralysis. Splint and apply traction as needed.
The patient will require X-rays, a CT scan, or an MRI to determine the extent of injury to the limb, so prepare the patient for transport. Use special care in suspected cervical spinal injury. If necessary, after splinting the injury site, also splint the areas above and below it to prevent further soft-tissue and neurovascular damage and to minimize pain. For example, if the forearm is injured, splint the wrist and elbow, too.
Types of splints include:
air splint—an inflatable splint
hard splint—a rigid splint with a firm surface, such as a long or short board, an aluminum ladder splint, or a cardboard splint
soft splint—a nonrigid splint, such as a pillow or blanket
traction splint—a splint that uses traction to decrease angulation and reduce pain.
Tips on applying a splint
Splint most injuries “as they lie,” except when the patient’s neurovascular status is compromised.
Whenever possible, have one person support the injured part while another applies padding and the splint.
Secure the splint with straps or gauze, not an elastic bandage.
To apply an air splint, slide the splint backward over your arm and grasp the distal portion of the injured limb. Then slip the splint from your arm onto the injured limb and inflate the splint. Don’t apply the splint too tightly; be sure to assess neurovascular integrity before placing the splint and then after the splint is in place.
SPECIAL CONSIDERATIONS
After the patient is stabilized, he’ll need ongoing care and assessment and, possibly, rehabilitation to ensure recovery. Specialists may be consulted for certain types of trauma.
Regularly evaluate the patient’s ABCs, as well as his neurologic status.
Keep the patient’s family informed about his condition and provide support as indicated.
Depending on the type of injury, the patient may be admitted to your facility or transferred to another facility.
HEAD
Concussion
By far the most common traumatic brain injury, a concussion results from a blow to the head—a blow hard enough to jostle the brain and make it strike the skull, causing temporary neural dysfunction, but not hard enough to cause a cerebral contusion. Most concussion patients recover completely within 24 to 48 hours. Repeated concussions, however, exact a cumulative toll on the brain.
CAUSES AND INCIDENCE
The blow that causes a concussion is usually sudden and forceful. It occurs when the head strikes a stationary object (as in a fall to the ground) or when a moving object strikes the head (as in a punch to the head). Such blows may also result from automobile accidents, athletic injury, or child abuse. Significant jarring can lead to unconsciousness. Microscopic shearing of nerve fibers is thought to occur in the brain from sudden acceleration or deceleration from the head injury.
COMPLICATIONS
Seizures
Persistent vomiting
Second-impact syndrome
SIGNS AND SYMPTOMS
A concussion may produce vomiting and a short-term loss of consciousness. The patient may also suffer from anterograde and retrograde amnesia, in which the patient not only can’t recall what happened immediately after the injury, but also has difficulty recalling events that led up to the traumatic incident. The presence of anterograde amnesia and the duration of retrograde amnesia reliably correlate with the injury’s severity. The length of the unconsciousness may also relate to the concussion’s severity.
This type of injury commonly causes adults to be irritable or lethargic, to behave out of character, and to complain of dizziness, nausea, or severe headache. Some children have no apparent ill effects, but many grow lethargic and somnolent in a few hours. Postconcussion syndrome—characterized by headache, dizziness, vertigo, anxiety, and fatigue—may persist for several weeks after the injury.
DIAGNOSIS
Differentiating between a concussion and more serious head injuries requires a thorough history of the injury and a neurologic examination. Such an examination must evaluate the patient’s level of consciousness (LOC), mental status, cranial nerve and motor function, deep tendon reflexes, and orientation to time, place, and person. If no abnormalities are found and if a severe head injury appears unlikely, the patient should be observed for signs of more severe cerebral trauma. Observation provides a baseline for gauging any deterioration in the patient’s condition. Whenever you suspect a severe head injury, obtain a computed tomography scan or magnetic resonance imaging to rule out fractures and more serious injuries. A neurosurgeon should be consulted immediately.
TREATMENT
Treatment for concussion varies according to the type of injury. Supportive care may include application of an ice pack to the site of injury, analgesics for mild headache, and sutures or adhesive strips for lacerations.
SPECIAL CONSIDERATIONS
Before discharge, provide a head injury instruction sheet and advise the patient to be alert for vomiting, worsening of headache, and signs of an ear bleed or cerebrospinal fluid leak.
♦ Instruct the family or caregiver to wake the patient every few hours at night for observation of his mental state and for medication administration. Tell them they should follow these precautions for at least 3 days. Review the head injury instruction sheet and ensure that the family or caregiver is aware of signs necessitating a return to the emergency department.
To avoid second-impact syndrome, it is important for athletes not to return to sports while they are still experiencing signs and symptoms of a concussion. Experiencing a second concussion before the first concussion has resolved may result in a rapid, possibly fatal brain swelling.
Cerebral contusion
A cerebral contusion is a bruising of brain tissue as a result of a severe blow to the head. More serious than a concussion, a contusion disrupts normal nerve function in the bruised area and may cause loss of consciousness, hemorrhage, edema, and even death.
CAUSES AND INCIDENCE
A cerebral contusion results from coup-contrecoup or acceleration-deceleration injuries. Such injuries can occur directly beneath the site of impact when the brain rebounds against the skull from the force of a blow (such as in a beating with a blunt instrument), when the force of the blow drives the brain against the opposite side of the skull, or when the head is hurled forward and stopped abruptly (as in an automobile accident when a driver’s head strikes the windshield). The brain continues moving and slaps against the skull (acceleration) and then rebounds (deceleration). These injuries can also cause the brain to strike against bony prominences inside the skull (especially the sphenoidal ridges), causing intracranial hemorrhage or hematoma that may result in tentorial herniation. (See Hemorrhage, hematoma, and tentorial herniation.)
SIGNS AND SYMPTOMS
The patient with a cerebral contusion may have severe scalp wounds and labored respirations. He may lose consciousness for a few minutes or longer. If conscious, he may be drowsy, confused, disoriented, agitated, or even violent. He may display hemiparesis, unequal pupillary response, and decorticate or decerebrate posturing. Eventually, he should return to a relatively alert state, perhaps with temporary aphasia, slight hemiparesis, or unilateral numbness. A lucid period followed by rapid deterioration suggests epidural hematoma.
DIAGNOSIS
An accurate history of the injury and a neurologic examination are the principal diagnostic tools. A computed tomography (CT) scan or magnetic resonance imaging shows ischemic tissue, hematomas, and fractures. Intracranial hemorrhage contraindicates lumbar puncture.
TREATMENT
Treatment of a cerebral contusion focuses on establishing a patent airway and performing regular evaluations of the patient’s level of consciousness (LOC), motor responses, and intracranial pressure. If needed, assist with a tracheotomy or endotracheal intubation. Start an I.V. fluid infusion with lactated Ringer’s or normal saline solution. Mannitol I.V. may be given in consultation with a neurosurgeon to reduce cerebral edema.
SPECIAL CONSIDERATIONS
Verify that a head CT scan has been performed to assess for a basilar skull fracture.
Restrict total fluid intake to 1,200 to 1,500 ml/day to reduce volume and intracerebral swelling.
If spinal injury is ruled out, elevate the bed’s head 30 degrees. Enforce bed rest.
If the patient is intubated, use mild hyperventilation until his partial pressure of arterial carbon dioxide reaches 30 to 35 mm Hg.
Type and crossmatch blood for a patient suspected of having an intracerebral hemorrhage. Such a patient may need a blood transfusion, and possibly a craniotomy, to control bleeding and to aspirate blood.
Insert an indwelling urinary catheter as ordered and monitor intake and output. If the patient is unconscious, insert a nasogastric tube to prevent aspiration.
Observe carefully for leakage of cerebrospinal fluid (CSF) from the nostrils and ear canals. If you detect blood in the canal and aren’t sure
whether CSF is mixed in, place a drop on a white sheet or a piece of filter paper and check for a central spot of blood surrounded by a lighter ring (halo sign). If CSF leakage develops, raise the bed’s head 30 degrees. If you detect CSF leaking from the nose, place a gauze pad under the nostrils. Be sure to tell the patient not to blow his nose, but to wipe it instead. If CSF leaks from the ear, position the patient so that the ear drains naturally, and don’t pack the ear or nose.
Monitor the patient’s vital signs and respirations regularly (usually every 15 minutes). Abnormal respirations could indicate a breakdown in the respiratory center in the brain stem and, possibly, impending tentorial herniation—a critical neurologic emergency.
Check his neurologic status frequently. Assess for restlessness, LOC, and orientation.
After the patient is stabilized, clean and dress any superficial scalp wounds. (If the skin has been broken, tetanus prophylaxis may be in order.) Assist with suturing if necessary.
Hemorrhage, hematoma, and tentorial herniation
Among the most serious consequences of a head injury are hemorrhage, hematoma, and tentorial herniation. An epidural hematoma results from a rapid accumulation of blood between the skull and the dura mater; a subdural hematoma results from a slow accumulation of blood between the dura mater and the subarachnoid membrane. Intracerebral hemorrhage occurs within the cerebrum itself. Tentorial herniation occurs when injured brain tissue swells and squeezes through the tentorial notch, constricting the brain stem.
Epidural hemorrhage or hematoma can cause immediate loss of consciousness, followed by a lucid interval lasting minutes to hours, which eventually gives way to a rapidly progressive decrease in the level of consciousness. Other effects are contralateral hemiparesis, progressively severe headache, ipsilateral pupillary dilation, and signs of increased intracranial pressure (ICP).
With a subacute or chronic subdural hemorrhage or hematoma, blood accumulates slowly, so symptoms may not occur until days after the injury. In an acute subdural hematoma, symptoms appear within 24 hours of the injury. Loss of consciousness occurs, commonly with weakness or paralysis. Intracerebral hemorrhage usually causes nuchal rigidity, photophobia, nausea, vomiting, dizziness, seizures, decreased respiratory rate, and progressive obtundation.
Tentorial herniation causes drowsiness, confusion, dilation of one or both pupils, hyperventilation, nuchal rigidity, bradycardia, and decorticate or decerebrate posturing. Irreversible brain damage or death can occur rapidly.
Intracranial hemorrhage may require a craniotomy to locate and control bleeding and to aspirate blood. Increased ICP may be controlled with I.V. mannitol, steroids, hyperventilation, or induced coma, but emergency surgery is usually required.
Fractured skull
Because of possible brain damage, a skull fracture is considered a neurosurgical condition. Skull fractures may be classified as simple (closed) or compound (open) and may displace bone fragments. Skull fractures are further described as linear, comminuted, depressed, or diastatic. A linear fracture is a common hairline break, without displacement of structures; a comminuted fracture splinters or crushes the bone into several fragments; a depressed fracture pushes the bone toward the brain; a diastatic fracture causes the skull to separate at the suture (joint between two plates).
In children, the skull’s thinness and elasticity allow a depression without a fracture. (A linear fracture across a suture line increases the possibility of epidural hematoma.) Skull fractures are also classified according to location, such as cranial vault fracture and basilar fractures. Because of the danger of grave cranial complications and meningitis, basilar fractures are usually far more serious than cranial vault fractures.
CAUSES AND INCIDENCE
Skull fractures invariably result from a traumatic blow to the head. Motor vehicle accidents, bad falls, sports injuries, and physical assaults top the list of causes. The brain can be directly affected by damage to the nervous system and by bleeding.
Closed head injuries occur in 200 out of every 100,000 patients. Severe head trauma carries a 30% mortality rate.
COMPLICATIONS
Infection
Intracerebral hemorrhage
Hematoma
Brain abscess
Increased intracranial pressure
SIGNS AND SYMPTOMS
Many skull fractures are accompanied by scalp wounds—abrasions, contusions, lacerations, or avulsions. If the scalp has been lacerated or torn away, bleeding may be profuse because the scalp contains many blood vessels. Occasionally, bleeding may be heavy enough to induce hypovolemic shock. The patient may also be in shock from other injuries or from medullary failure in severe head injuries.
Linear fractures that are associated only with concussion don’t produce loss of consciousness. They require evaluation, but not definitive treatment. A fracture that results in a cerebral contusion or laceration, however, may cause the classic signs of brain injury: agitation and irritability, loss of consciousness, changes in respiratory pattern (labored respirations), abnormal deep tendon reflexes, and altered pupillary and motor responses.
If the patient with a skull fracture remains conscious, he is apt to complain of a persistent, localized headache. A skull fracture may also result in cerebral edema, which may cause compression of the reticular activating system. This cuts off the normal flow of impulses to the brain and results in possible respiratory distress. The patient may experience alterations in level of consciousness (LOC), progressing to unconsciousness or even death.
When jagged bone fragments pierce the dura mater or the cerebral cortex, skull fractures may cause subdural, epidural, or intracerebral hemorrhage or hematoma. With the resulting spaceoccupying lesions, clinical findings may include hemiparesis, unequal pupils, dizziness, seizures, projectile vomiting, progressive unresponsiveness, and decreased pulse and respiratory rates. Sphenoidal fractures may also damage the optic nerve, causing blindness, whereas temporal fractures may cause unilateral deafness or facial paralysis. Symptoms reflect the head injury’s severity and extent. However, some elderly patients may have cortical brain atrophy, with more space for brain swelling under the cranium, and consequently may not show signs of increased intracranial pressure (ICP) until it’s very high.
Vault fractures commonly produce soft-tissue swelling near the fracture, making it difficult to detect without a computed tomography (CT) scan.
Basilar fractures commonly produce a hemorrhage from the nose, pharynx, or ears; blood under the periorbital skin (raccoon eyes) and under the conjunctiva; and Battle’s sign (supramastoid ecchymosis), sometimes with bleeding behind the eardrum (hemotympanum). This type of fracture may also cause cerebrospinal fluid (CSF) or even brain tissue to leak from the nose or ears.
Depending on the extent of brain damage, the patient with a skull fracture may suffer residual effects, such as seizures, hydrocephalus, and organic brain syndrome. Children may develop headaches, giddiness, easy fatigability, neuroses, and behavior disorders.
DIAGNOSIS
Suspect brain injury in all patients with a skull fracture until clinical evaluation proves otherwise. Consequently, you’ll need to obtain a thorough injury history and magnetic resonance imaging (MRI) or a CT scan (to locate the fracture) for every suspected skull injury. (Keep in mind that many vault fractures aren’t visible or palpable.)
A fracture also requires a neurologic examination to check cerebral function (mental status and orientation to time, place, and person), LOC, pupillary response, motor function, and deep tendon reflexes.
Using reagent strips, test the draining nasal or ear fluid for CSF. The tape will turn blue in the presence of CSF but will remain the same in the presence of blood alone. However, the tape will also turn blue if the patient is hyperglycemic. Also check the patient’s bedsheets for the halo sign—a blood-tinged spot surrounded by a lighter ring—from leakage of CSF.
Brain damage can be assessed by a CT scan and MRI, which reveal intracranial hemorrhage from ruptured blood vessels and swelling. Expanding lesions contraindicate a lumbar puncture.
TREATMENT
Although occasionally even a simple linear skull fracture can tear an underlying blood vessel or cause a CSF leak, linear fractures generally require only supportive treatment, including mild analgesics such as acetaminophen, and cleaning, debridement, and repair of any wounds after injection of a local anesthetic.
If the patient with a skull fracture hasn’t lost consciousness, observe him in the emergency department for at least 4 hours. Following this observation period, if his vital signs are stable and if the neurosurgeon concurs, you can discharge him. Before discharge, give the patient an instruction sheet to follow for 24 to 48 hours of observation at home.
More severe vault fractures, especially depressed fractures, usually require a craniotomy to elevate or remove fragments that have been driven into the brain and to extract foreign bodies and necrotic tissue. This reduces the risk of infection and further brain damage. Other treatments for severe vault fractures include antibiotic therapy and, in profound hemorrhage, blood transfusions.
Basilar fractures call for immediate prophylactic antibiotics to prevent the onset of meningitis from CSF leaks as well as close observation for secondary hematomas and hemorrhages. Surgery may be necessary.
SPECIAL CONSIDERATIONS
Establish and maintain a patent airway; nasal airways are contraindicated in patients who may have a basilar skull fracture. Intubation may be necessary. Suction the patient through the mouth, not the nose, to prevent introducing bacteria if a CSF leak is present.
Be sure to obtain a complete history of the traumatic injury from the patient, family members, any eyewitnesses, and emergency medical services personnel. Ask whether the patient lost consciousness and, if so, for how long.
Assist with diagnostic tests, including a complete neurologic examination, CT scan, and other studies.
Check for abnormal reflexes such as Babinski’s reflex.
Look for CSF draining from the patient’s ears, nose, or mouth. Check pillowcases and linens for CSF leaks and look for a halo sign. If the patient’s nose is draining CSF, wipe it—don’t let him blow it. If an ear is draining, cover it lightly with sterile gauze—don’t pack it.
Position the patient with a head injury so that secretions can drain properly. Elevate the bed’s head 30 degrees if intracerebral injury is suspected.
Cover scalp wounds carefully with a sterile dressing; control any bleeding as necessary.
Take seizure precautions, but don’t restrain the patient. Agitated behavior may be due to hypoxia or increased ICP, so check for these symptoms. Speak in a calm, reassuring voice, and touch the patient gently. Don’t make any sudden, unexpected moves.
Don’t give the patient opioids or sedatives because they may depress respirations, increase carbon dioxide levels, lead to increased ICP, and mask changes in neurologic status. Give acetaminophen or another mild analgesic for pain as ordered.
If a skull fracture requires surgery, proceed as follows:
Obtain consent, as needed, to shave the patient’s head. Explain that you’re performing this procedure to provide a clean area for surgery. Type and crossmatch blood. Obtain baseline laboratory studies, such as a complete blood count, serum electrolyte studies, prothrombin time, partial thromboplastin time, and urinalysis.
After surgery, monitor the patient’s vital signs and neurologic status frequently (usually every 5 minutes until the patient is stable and then every 15 minutes for 1 hour), and note any changes in LOC. Because skull fractures and brain injuries heal slowly, don’t expect dramatic postoperative improvement.
Monitor intake and output frequently, and maintain the patency of the indwelling urinary catheter. Monitor fluid intake carefully. Because hypotonic fluids (such as dextrose 5% in water) can increase cerebral edema, give fluids only as indicated.
If the patient is unconscious, provide parenteral nutrition. (Remember, the patient may regurgitate and aspirate food if you use a nasogastric tube for feedings.)
If the fracture doesn’t require surgery, proceed as follows:
Wear sterile gloves to examine the scalp laceration. With your finger, probe the wound for foreign bodies and a palpable fracture. Gently clean lacerations and the surrounding area; cover them with sterile gauze. The wound should be sutured if necessary.
Provide emotional support for the patient and his family. Explain the need for procedures to reduce the risk of brain injury.
Before discharge, instruct the patient’s family to watch closely for changes in mental status, LOC, or respirations and to give the patient acetaminophen for a headache. Tell them to return him to the hospital immediately if his LOC decreases, if his headache persists after several doses of mild analgesics, if he vomits more than once, or if he develops weakness in his arms or legs.
Teach the patient and his family how to care for his scalp wound. Emphasize the need to return for suture removal and follow-up evaluation.
Fractured nose
The most common facial fracture, a fractured nose usually results from blunt injury and may be associated with other facial fractures. The fracture’s severity depends on the direction, force, and type of the blow. A severe, comminuted fracture may cause extreme swelling or bleeding that may partially obstruct the airway. Inadequate or delayed treatment may cause permanent nasal displacement, septal deviation, and obstruction.
CAUSES AND INCIDENCE
Nasal bone fractures usually result from direct trauma. The causative injury may be relatively minor, such as a fall, or more severe, such as a car accident.
COMPLICATIONS
Deviated septum
Airway obstruction
Septal hematoma
Cerebrospinal fluid (CSF) leakage
Intracranial air penetration
SIGNS AND SYMPTOMS
Immediately after injury, a nosebleed may occur, and soft-tissue swelling may quickly obscure the break. Nasal fractures may cause significant blood loss. After several hours, pain, edema, periorbital ecchymoses, and nasal displacement and deformity are prominent. Possible complications include septal hematoma, which may lead to abscess formation, resulting in avascular septal necrosis and saddle nose deformity.
DIAGNOSIS
Palpation, Xrays, and clinical findings such as a deviated septum confirm a nasalfracture.
Diagnosis also requires a complete patient history, including the injury’s cause and the amount of nasal bleeding. Watch for clear fluid drainage, which may suggest a CSF leak and a basilar skull fracture. If facial or mandibular fractures are suspected, a computed tomography (CT) scan is necessary.
TREATMENT
Treatment restores normal facial appearance and re-establishes bilateral nasal passage after swelling subsides. Reduction of the fracture corrects alignment; immobilization (intranasal packing and an external splint shaped to the nose and taped) maintains it. Reduction is best accomplished in the operating room under local anesthesia for adults and general anesthesia for children. Severe swelling may delay treatment. CSF leakage calls for close observation, a CT scan of the basilar skull, and antibiotic therapy; septal hematoma requires incision and drainage to prevent necrosis.
Start treatment immediately. While waiting for X-rays, apply ice packs to the nose to minimize swelling. Wrap the ice packs in a light towel to prevent ice from directly contacting the skin. To control anterior bleeding, gently apply local pressure. Posterior bleeding is rare and requires an internal tamponade applied in the emergency department.
SPECIAL CONSIDERATIONS
Because the patient will find breathing more difficult as swelling increases, instruct him to breathe slowly through his mouth. To warm the inhaled air during cold weather, tell him to cover his mouth with a handkerchief or scarf. To prevent subcutaneous emphysema or intracranial air penetration (and potential meningitis), warn him not to blow his nose.
After packing and splinting, apply ice in a plastic bag.
Before discharge, tell the patient that ecchymoses should fade after about 2 weeks.
Dislocated or fractured jaw
Dislocation of the jaw is a displacement of the temporomandibular joint. A jaw fracture is a break in one or both of the two maxillae (upper jawbones) or the mandible (lower jawbone). Treatment can usually restore jaw alignment and function.
CAUSES AND INCIDENCE
Simple fractures or dislocations are usually caused by a manual blow along the jawline; more serious compound fractures commonly result from automobile accidents. Other causes include industrial accidents, recreational or sports injuries, assaults, or other trauma. Recurrence of a dislocated jaw is common.
COMPLICATIONS
Infection
Sublingual hematoma
Trauma to nerves of jaw and face
SIGNS AND SYMPTOMS
Malocclusion is the most obvious sign of a dislocation or fracture. Other signs include mandibular pain, swelling, ecchymosis, loss of
function, and asymmetry. In addition, mandibular fractures that damage the alveolar nerve produce paresthesia or anesthesia of the chin and lower lip. Maxillary fractures produce infraorbital paresthesia and commonly accompany fractures of the nasal and orbital complex.
function, and asymmetry. In addition, mandibular fractures that damage the alveolar nerve produce paresthesia or anesthesia of the chin and lower lip. Maxillary fractures produce infraorbital paresthesia and commonly accompany fractures of the nasal and orbital complex.
DIAGNOSIS
Abnormal maxillary or mandibular mobility during the physical examination and a history of traumatic injury suggest a fracture or dislocation; X-rays confirm it.
TREATMENT
As in all traumatic injuries, check first for a patent airway, adequate ventilation, and pulses; then control hemorrhage and check for other injuries. As necessary, maintain a patent airway with an oropharyngeal airway, nasotracheal intubation, or a cricothyrotomy. Relieve pain with analgesics as needed.
After the patient stabilizes, surgical reduction and fixation by wiring restores mandibular and maxillary alignment. Maxillary fractures may also require reconstruction and repair of softtissue injuries. Teeth and bones are never removed during surgery unless unavoidable. If the patient has lost teeth from trauma, the surgeon will decide whether they can be reimplanted. If they can, he’ll reimplant them within 6 hours, while they’re still viable. Viability is increased if the tooth is placed in milk, saliva, or normal saline solution. Dislocations are usually reduced manually under anesthesia.
SPECIAL CONSIDERATIONS
After reconstructive surgery, perform the following:
Position the patient on his side with his head slightly elevated. He’ll usually have a nasogastric tube in place, with low suction to remove gastric contents and prevent nausea, vomiting, and aspiration of vomitus. As necessary, suction the nasopharynx through the nose or by pulling the cheek away from the teeth and inserting a small suction catheter through any natural gap between teeth.
If the patient isn’t intubated, provide nourishment through a straw. If he has a natural gap between his teeth, insert the straw there; if not, one or two teeth may have to be extracted. After the patient can tolerate clear liquids, offer milkshakes, broth, juices, pureed foods, and nutritional supplements.
If the patient can’t tolerate oral fluids, I.V. therapy can maintain hydration postoperatively.
Administer antiemetics as indicated to minimize nausea and prevent aspiration of vomitus (a real danger in a patient whose jaw is wired). Keep a pair of wire cutters at the bedside to snip the wires should the patient vomit.
A dental water-pulsator may be used for mouth care while the wires are intact.
Because the patient will have difficulty talking while his jaw is wired, provide a Magic Slate or pencil and paper and suggest appropriate diversionary activities.
Perforated eardrum
Perforation of the eardrum is a rupture of the tympanic membrane that may cause otitis media and hearing loss.
CAUSES AND INCIDENCE
The usual cause of perforated eardrum is trauma, such as the deliberate or accidental insertion of foreign objects (cotton swabs or bobby pins) or sudden excessive changes in pressure (explosion, a blow to the head, flying, or diving). The injury may also result from untreated otitis media and, in children, from acute otitis media.
COMPLICATIONS
Mastoiditis
Meningitis
Otitis media
Permanent hearing loss
SIGNS AND SYMPTOMS
Sudden onset of a severe earache and bleeding, clear drainage, or drainage of pus from the ear are the first signs of a perforated eardrum. Other symptoms include hearing loss, tinnitus, and vertigo. Purulent otorrhea within 24 to 48 hours of injury signals infection.
DIAGNOSIS
A severe earache and bleeding from the ear with a history of trauma strongly suggest a perforated eardrum; direct visualization of the perforated tympanic membrane with an otoscope confirms it.
Additional diagnostic measures include audiometric testing and a check of voluntary facial movements to rule out facial nerve damage.
TREATMENT
If you detect bleeding from the ear, use a sterile, cotton-tipped applicator to absorb the blood, and check for purulent drainage or evidence
of cerebrospinal fluid leakage. A culture of the specimen may be appropriate.
of cerebrospinal fluid leakage. A culture of the specimen may be appropriate.
Irrigation of the ear is absolutely contraindicated in a patient with perforation of the eardrum.
Apply a sterile dressing over the outer ear, and refer the patient to an ear specialist. A large perforation with uncontrolled bleeding may require immediate surgery to approximate the ruptured edges. Other measures may include administration of a mild analgesic, a sedative to decrease anxiety, and an oral antibiotic.
SPECIAL CONSIDERATIONS
Before discharge, tell the patient not to blow his nose or get water in his ear canal until the perforation heals.
Advise the patient to follow up with an ear specialist, as appropriate.
Instruct the patient and his family to notify the physician if he develops signs of infection, such as fever, increasing discomfort, and continued or purulent drainage.
Inform the authorities if child abuse is suspected as the cause of injuries.
NECK AND SPINE
Acceleration-deceleration cervical injuries
Acceleration-deceleration cervical injuries (commonly known as whiplash) result from sharp hyperextension and flexion of the neck that damages muscles, ligaments, disks, and nerve tissue. The prognosis for this type of injury is excellent; symptoms usually subside with treatment.
CAUSES AND INCIDENCE
Whiplash commonly results from rear-end automobile accidents. A seat belt keeps a person’s body from being thrown forward, but the head may snap forward, then backward, causing a whiplash injury to the neck. Other causes include roller coasters or other amusement park rides, sports injuries, or punches or shoves.
SIGNS AND SYMPTOMS
Although symptoms may develop immediately, they’re often delayed 12 to 24 hours if the injury is mild. Whiplash produces moderate to severe anterior and posterior neck pain. Within several days, the anterior pain diminishes, but the posterior pain persists or even intensifies, causing patients to seek medical attention if they didn’t do so before. Whiplash may also cause dizziness, gait disturbances, vomiting, headache, nuchal rigidity, neck muscle asymmetry, and rigidity or numbness in the arms.
DIAGNOSIS
Full cervical spine X-rays are required to rule out cervical fractures. If the X-rays are negative, the physical examination focuses on motor ability and sensation below the cervical spine to detect signs of nerve root compression. If the patient’s cervical spine continues to be tender to examination, magnetic resonance imaging or computed tomography scan may be required to rule out ligamentous injury.
TREATMENT
Treatment aims to control symptoms and includes:
a mild analgesic—such as aspirin with codeine or ibuprofen—and possibly a muscle relaxant—such as diazepam, cyclobenzaprine, or chlorzoxazone with acetaminophen
ice or cool compresses to the neck to relieve pain
immobilization with a soft, padded cervical collar for several days or weeks
in severe muscle spasms, short-term cervical traction
Most whiplash patients are discharged immediately.
SPECIAL CONSIDERATIONS
In all suspected spinal injuries, as- sume that the spine is injured until proven otherwise. Until an X-ray rules out a cervical fracture, move the patient as little as possible. Before the X-ray is taken, remove any ear and neck jewelry carefully. Don’t undress the patient; cut clothes away if necessary. Caution him to avoid making movements that could injure his spine.
Teach the patient to watch for possible adverse drug effects; to avoid alcohol if he’s taking diazepam, opioids, or muscle relaxants; and to rest for a few days and avoid lifting heavy objects.
Instruct the patient to return to the hospital immediately if he experiences persistent pain or develops numbness, tingling, or weakness on one or both sides.
Spinal injuries
Spinal injuries (without cord damage) include fractures, contusions, and compressions of the vertebral column, usually as a result of head or neck trauma. The real danger lies in possible spinal cord damage. Spinal fractures most commonly occur in the 5th, 6th, and 7th cervical, 12th thoracic, and 1st lumbar vertebrae.
CAUSES AND INCIDENCE
Most serious spinal injuries result from motor vehicle accidents, falls, dives into shallow water, and gunshot wounds. Less serious injuries result from heavy object lifting and minor falls. Spinal dysfunction may also result from hyperparathyroidism and neoplastic lesions.
Spinal cord injuries occur in 12,000 to 15,000 people per year in the United States. About 10,000 of these injuries cause permanent paralysis; many other patients die as a result of these injuries. Most spinal cord injuries occur in males between the ages of 15 and 35 years; about 5% occur in children. Mortality is higher in pediatric spinal cord injuries.
COMPLICATIONS
Spinal cord injury
Autonomic dysreflexia
Spinal shock
Neurogenic shock
SIGNS AND SYMPTOMS
The most obvious symptoms of spinal injury are muscle spasm and back pain that worsen with movement. In cervical fractures, pain may produce point tenderness; in dorsal and lumbar fractures, it may radiate to other body areas such as the legs. After mild injuries, symptoms may be delayed for several days or weeks. If the injury damages the spinal cord, clinical effects range from mild paresthesia to quadriplegia and shock.
DIAGNOSIS
The diagnosis is typically based on the patient’s history, physical examination, X-rays, computed tomography (CT) scan, and magnetic resonance imaging (MRI).
The patient history may reveal a traumatic injury, a metastatic lesion, an infection that could produce a spinal abscess, or an endocrine disorder. The physical examination (including a neurologic evaluation) locates the level of injury and detects cord damage.
Spinal X-rays, the most important diagnostic measure, locate the fracture. In spinal compression, a lumbar puncture may show increased cerebrospinal fluid pressure from a lesion or trauma; a CT scan or MRI can locate a spinal mass.
TREATMENT
The primary treatment after a spinal injury is immediate immobilization to stabilize the spine and prevent cord damage; other measures are supportive. Cervical injuries require immobilization, using a type of cervical immobilization device (CID) on both sides of the patient’s head, a hard cervical collar, or skeletal traction with skull tongs or a halo device.
Treatment of stable lumbar and dorsal fractures consists of bed rest on firm support (such as a bed board), analgesics, and muscle relaxants until the fracture stabilizes (usually in 10 to 12 weeks). Later measures include exercises to strengthen the back muscles and use of a back brace or other device to provide support while walking.
An unstable dorsal or lumbar fracture requires a plaster cast, a turning frame and, in severe fracture, a laminectomy and spinal fusion.
When the spinal injury results in compression of the spinal column, neurosurgery may relieve the pressure. If the cause of compression is a metastatic lesion, chemotherapy and radiation may relieve it. Surface wounds accompanying the spinal injury require tetanus prophylaxis unless the patient has been immunized recently.
SPECIAL CONSIDERATIONS
In all spinal injuries, suspect cord damage until proven otherwise.
During the initial assessment and X-ray studies, immobilize the patient on a firm surface with CID. Tell him not to move, and avoid moving him yourself because hyperflexion can damage the cord. If you must move the patient, get at least three other members of the staff to help you logroll him to avoid disturbing body alignment.
Throughout assessment, offer comfort and reassurance. Remember, the fear of possible paralysis will be overwhelming. Talk to the patient quietly and calmly. Allow a family member who isn’t too distraught to accompany him.
If the injury requires surgery, administer prophylactic antibiotics as ordered. Catheterize the patient as ordered to avoid urine retention, and monitor bowel elimination patterns to avoid impaction.
Explain traction methods to the patient and his family. Reassure them that traction devices
don’t penetrate the brain. If the patient has a halo or skull-tong traction device, clean pin sites daily, trim hair short, and provide analgesics for persistent headaches. During traction, turn the patient often to prevent pneumonia, embolism, and skin breakdown; perform passive range-of-motion exercises to maintain muscle tone. If available, use a CircOlectric bed or Stryker frame to facilitate turning and to avoid spinal cord injury.
Turn the patient on his side during feedings to prevent aspiration. Create a relaxed atmosphere at mealtimes.
Suggest appropriate diversionary activities to fill the patient’s hours of immobility.
Watch closely for neurologic changes. Immediately report changes in skin sensation and loss of muscle strength—either of which might indicate pressure on the spinal cord, possibly as a result of edema or shifting bone fragments.
Help the patient walk as soon as the physician allows; he’ll probably need to wear a back brace.
Before discharge, instruct the patient about continuing analgesics or other medication, and stress the importance of regular follow-up examinations.
To help prevent a spinal injury from becoming a spinal cord injury, educate firemen, policemen, paramedics, and the general public about the proper way to handle such injuries.
THORAX
Blunt chest injuries
Chest injuries, including blunt chest injuries, consist of myocardial contusion as well as rib and sternal fractures that may be simple, multiple, displaced, or jagged. Such fractures may cause potentially fatal complications, such as hemothorax, pneumothorax, hemorrhagic shock, and diaphragmatic rupture.
CAUSES AND INCIDENCE
Motor vehicle accidents cause two thirds of major chest injuries in the United States. Other common causes include sports and blast injuries and cardiopulmonary resuscitation. About 50% of these injuries affect the chest wall; 80% of those with significant blunt chest trauma also have extrathoracic injuries.
Chest injuries account for 70% of all trauma-related deaths in the United States.
COMPLICATIONS
Hemothorax
Hemorrhagic shock
Pneumothorax
Tension pneumothorax
Diaphragmatic rupture
Liver laceration
Myocardial tears
Cardiac tamponade
Pulmonary artery tears
Ventricular rupture
Rupture of the aorta
Bronchial, tracheal, or esophageal tears
SIGNS AND SYMPTOMS
Rib fractures produce tenderness, slight edema over the fracture site, and pain that worsens with deep breathing and movement; this painful breathing causes the patient to display shallow, splinted respirations that may lead to hypoventilation. Sternal fractures, which are usually transverse and located in the middle or upper sternum, produce persistent chest pains, even at rest. If a fractured rib tears the pleura and punctures a lung, it causes pneumothorax. This usually produces severe dyspnea, cyanosis, agitation, extreme pain and, when air escapes into chest tissue, subcutaneous emphysema.
Multiple rib fractures within two or more places may cause flail chest, in which a portion of the chest wall “caves in,” causing a loss of chest wall integrity and preventing adequate lung inflation. (See Flail chest: Paradoxical breathing.)
Signs and symptoms of flail chest include bruised skin, extreme pain caused by rib fracture and disfigurement, paradoxical chest movements, tachycardia, hypotension, respiratory acidosis, cyanosis, and rapid, shallow respirations. Flail chest can also cause tension pneumothorax, a condition in which air enters the chest but can’t be ejected during exhalation. This life-threatening thoracic pressure buildup causes lung collapse and subsequent mediastinal shift. The cardinal symptoms of tension pneumothorax include severe dyspnea, absent breath sounds (on the affected side), agitation, jugular vein distention, tracheal deviation (away from the affected side), cyanosis, and shock.
Hemothorax occurs when a rib lacerates lung tissue or an intercostal artery, causing blood to collect in the pleural cavity, thereby
compressing the lung and limiting respiratory capacity. It can also result from rupture of large or small pulmonary vessels.
compressing the lung and limiting respiratory capacity. It can also result from rupture of large or small pulmonary vessels.
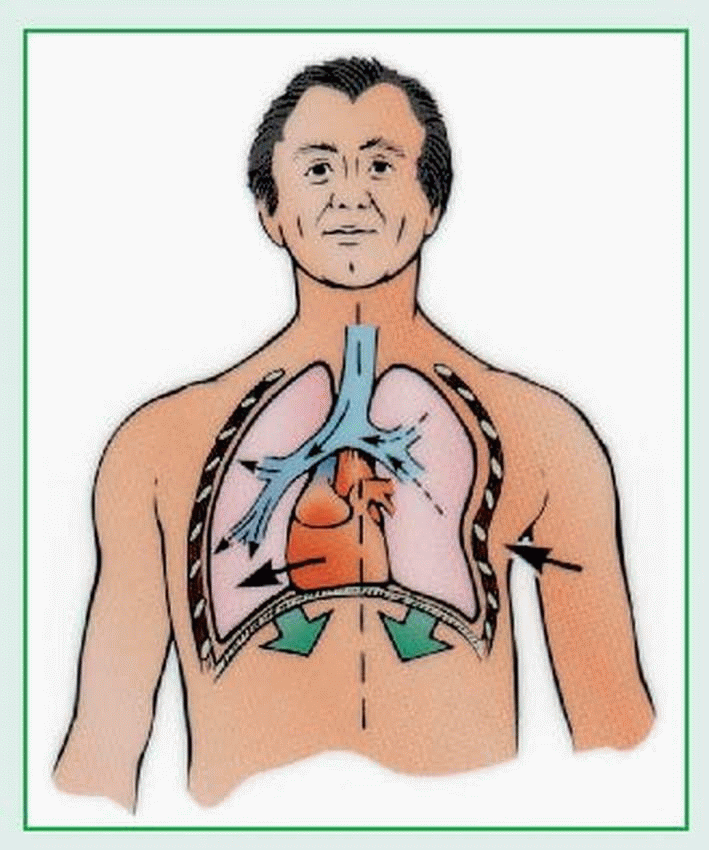
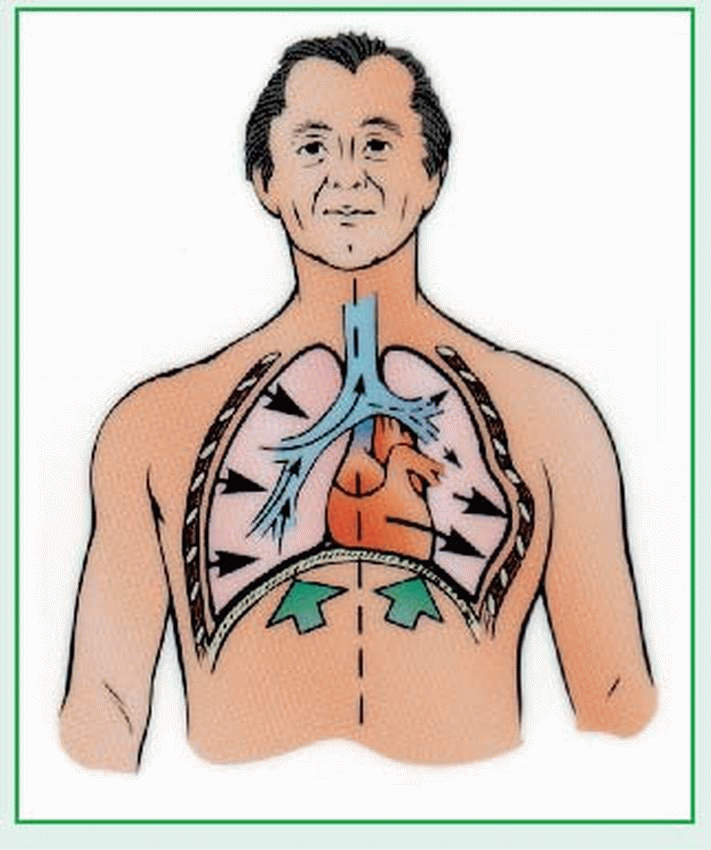
Flail chest: Paradoxical breathing
A patient with a blunt chest injury may develop flail chest, in which a portion of the chest “caves in.” This results in paradoxical breathing, described below.
Massive hemothorax is the most common cause of shock after a chest injury. Although slight bleeding occurs even with mild pneumothorax, such bleeding resolves very quickly, usually without changing the patient’s condition. Rib fractures may also cause pulmonary contusion (resulting in hemoptysis, hypoxia, dyspnea, and possible obstruction), large myocardial tears (which can be rapidly fatal), and small myocardial tears (which can cause pericardial effusion).
Myocardial contusions—actual bruising of the heart muscle—produce electrocardiographic (ECG) abnormalities. Laceration or rupture of the aorta is almost always immediately fatal. Because aortic laceration may develop 24 hours after blunt injury, patient observation is critical. Diaphragmatic rupture (usually on the left side) causes severe respiratory distress. Unless treated early, abdominal viscera may herniate through the rupture into the thorax (with resulting bowel sounds in the chest), compromising both circulation and the lungs’ vital capacity.
Other complications of blunt chest trauma may include cardiac tamponade, pulmonary artery tears, ventricular rupture, and bronchial, tracheal, or esophageal tears or rupture.
DIAGNOSIS
A history of trauma with dyspnea, chest pain, and other typical clinical features suggest a blunt chest injury. To determine its extent, a physical examination and diagnostic tests are needed.
In hemothorax, percussion reveals dullness. In tension pneumothorax, it reveals tympany. Auscultation may reveal a change in position of the loudest heart sound.
Chest X-rays may confirm rib and sternal fractures, pneumothorax, flail chest, pulmonary contusions, lacerated or ruptured aorta, tension pneumothorax, diaphragmatic rupture, lung compression, or atelectasis with hemothorax.
With cardiac damage, the ECG may show abnormalities, including unexplained tachycardias, atrial fibrillation, bundle-branch block (usually right), ST-segment changes, and ventricular arrhythmias such as multiple premature ventricular contractions.
Serial aspartate aminotransferase, alanine aminotransferase, lactate dehydrogenase, creatine kinase (CK), and CK-MB levels are elevated. However, cardiac enzymes fail to detect up to 50% of patients with myocardial damage.
Retrograde aortography, computed tomography angiography, and transesophageal echocardiography reveal aortic laceration or rupture.
Contrast studies and liver and spleen scans detect diaphragmatic rupture.
Echocardiography, computed tomography scans, and cardiac and lung scans show the injury’s extent.
TREATMENT
Blunt chest injuries call for immediate physical assessment, control of bleeding, maintenance of a patent airway, adequate ventilation, and fluid and electrolyte balance.
SPECIAL CONSIDERATIONS
Check all pulses and level of consciousness. Evaluate skin color and temperature, depth of respiration, use of accessory muscles, and length of inhalation compared to exhalation.
Check pulse oximetry values for adequate oxygenation.
Observe tracheal position. Look for distended jugular veins and paradoxical chest motion. Listen to heart and breath sounds carefully; palpate for subcutaneous emphysema (crepitation) or a lack of structural integrity of the ribs.
Obtain a history of the injury. Unless severe dyspnea is present, have the patient locate the pain, and ask if he’s having trouble breathing. Obtain laboratory studies (arterial blood gas analysis, cardiac enzyme studies, complete blood count, type, and crossmatch).
For simple rib fractures, have the patient cough and breathe deeply to mobilize secretions while splinting to decrease pain. Give adequate analgesics, encourage bed rest, and apply heat. Don’t strap or tape the chest.
More severe fractures may require administration of intercostal nerve blocks. (Obtain X-rays before and after the nerve blocks to rule out pneumothorax.) Intubate the patient with excessive bleeding or hemopneumothorax. Chest tubes may be inserted to treat hemothorax and to assess the need for thoracotomy. To prevent atelectasis, turn the patient frequently and encourage coughing and deep-breathing exercises.
Pneumothorax may require placement of a chest tube anterior to the midaxillary line at the fourth intercostal space to aspirate as much air as possible from the pleural cavity and to re-expand the lungs. When time permits, insert chest tubes attached to water-seal drainage and suction.
For flail chest, place the patient in semi-Fowler’s position. Re-expanding the lung is the first definitive care measure. Administer oxygen at a high flow rate under positive pressure. Suction the patient frequently, as completely as possible. Maintain acid-base balance. Observe carefully for signs of tension pneumothorax. Start I.V. therapy, using lactated Ringer’s or normal saline solution. Beware of both excessive and insufficient fluid resuscitation.
For hemothorax, treat shock with I. V. infusions of lactated Ringer’s or normal saline solution. Administer packed red blood cells for blood losses greater than 1,500 ml or circulating blood volume losses exceeding 30%. Administer oxygen. The patient may need insertion of chest tubes in the fourth intercostal space anterior to the midaxillary line to remove blood. Monitor and document vital signs and blood loss. Watch for and respond immediately to falling blood pressure, rising pulse rate, and hemorrhage—all require a thoracotomy to stop bleeding.
For a pulmonary contusion, give limited amounts of colloids (such as salt-poor albumin, whole blood, or plasma) as appropriate to replace volume and maintain oncotic pressure. Give analgesics as necessary. Monitor blood gas levels to ensure adequate ventilation; provide oxygen therapy, mechanical ventilation, and chest tube care.
For suspected cardiac damage, close intensive care or telemetry may detect arrhythmias and prevent cardiogenic shock. Impose bed rest in semi-Fowler’s position (unless the patient requires shock position); administer oxygen, analgesics, and supportive drugs to control heart failure or supraventricular arrhythmias as needed. Watch for cardiac tamponade, which calls for pericardiocentesis. (Provide essentially the same care as you would for a patient with a myocardial infarction.)
For myocardial rupture, septal perforation, and other cardiac lacerations, immediate surgical repair is mandatory. Less severe ventricular wounds require use of a digital or balloon catheter; atrial wounds require a clamp or balloon catheter
For patients with aortic rupture or laceration, immediate surgery is mandatory, using synthetic grafts or anastomosis to repair the damage. Give large volumes of I. V. fluids (lactated Ringer’s or normal saline solution) and whole blood, along with oxygen at very high flow rates;
then transport the patient promptly to the operating room.
then transport the patient promptly to the operating room.
For tension pneumothorax, the patient may need insertion of a 14G to 16G angiocatheter in the second intercostal space at the midclavicular line to release pressure in the chest. After this, insert a chest tube to normalize pressure and re-expand the lung. Administer oxygen under positive pressure along with I.V. fluids
♦ For a diaphragmatic rupture, insert a nasogastric tube to temporarily decompress the stomach, and prepare the patient for surgical repair.
Penetrating chest wounds
Depending on their size, penetrating chest wounds may cause varying degrees of damage to bones, soft tissue, blood vessels, and nerves. Mortality and morbidity from such wounds depend on the wound’s size and severity. Gunshot wounds are usually more serious than stab wounds because they cause more severe wounds with rapid blood loss. Ricochet within a gunshot wound commonly damages large areas and multiple organs. Despite prompt, aggressive treatment, up to 90% of patients with penetrating chest wounds die.
CAUSES AND INCIDENCE
Stab wounds from a knife or an ice pick are the most common penetrating chest wounds; gunshot wounds are a close second. Wartime explosions or firearms fired at close range are the usual sources of large, gaping wounds.
Penetrating chest injuries cause one in every four deaths in the United States. Many patients with this type of injury die after reaching the hospital.
COMPLICATIONS
Arrhythmias
Cardiac tamponade
Mediastinitis
Subcutaneous emphysema
Bronchopleural fistula
Myocardial rupture
Pneumothorax
Rib and sternal fractures
Shock
Tears and lacerations of the tracheobronchial tree
SIGNS AND SYMPTOMS
In addition to the obvious chest injuries, penetrating chest wounds can also cause:
a sucking sound as the diaphragm contracts and air enters the chest cavity through the opening in the chest wall
tachycardia due to anxiety and blood loss
weak, thready pulse due to massive blood loss and hypovolemic shock
varying levels of consciousness, depending on the injury’s extent. If the patient is awake and alert, the severe pain will make him splint his respirations, thereby reducing his vital capacity
Penetrating chest wounds may also cause lung lacerations (bleeding and substantial air leakage through the chest wall), arterial lacerations (loss of more than 100 ml blood/hour through the chest tube), exsanguination, pneumothorax (air in pleural space causes loss of negative intrathoracic pressure and lung collapse), tension pneumothorax (intrapleural air accumulation causes potentially fatal mediastinal shift), and hemothorax. Other effects may include arrhythmias, cardiac tamponade, mediastinitis, subcutaneous emphysema, esophageal perforation, bronchopleural fistula, and tracheobronchial, abdominal, or diaphragmatic injuries.
DIAGNOSIS
An obvious chest wound and a sucking sound during breathing confirm the diagnosis of a penetrating chest wound. Consider any lower thoracic chest injury a thoracoabdominal injury until proven otherwise.
Baseline tests include:
pulse oximetry and arterial blood gas analysis to assess respiratory status
chest X-rays before and after chest tube placement to evaluate the injury and tube placement (However, in an emergency, don’t wait for chest X-ray results before inserting the chest tube.)
complete blood count, including hemoglobin (Hb) level, hematocrit (HCT), and differential (Low Hb level and HCT reflect severe blood loss; in early blood loss, these values may be normal.)
palpation and auscultation of the chest and abdomen to evaluate damage to adjacent organs and structures
TREATMENT
Penetrating chest wounds require immediate support of respiration and circulation, prompt surgical repair, and measures to prevent complications.
SPECIAL CONSIDERATIONS
Immediately assess airway, breathing, and circulation. Establish a patent airway, support ventilation, and monitor pulses frequently.
Place an occlusive dressing over the sucking wound. Watch for signs of tension pneumothorax (respiratory distress, tachycardia, tachypnea, and diminished or absent breath sounds on the affected side [tracheal shift]); if tension pneumothorax develops, temporarily remove the occlusive dressing to create a simple pneumothorax.
Control blood loss (remember to look under the patient to estimate loss), type and crossmatch blood, and replace blood and fluids as necessary.
Assist with chest X-ray and placement of chest tubes (using water-seal drainage) to re-establish intrathoracic pressure and to drain blood in a hemothorax. A second X-ray will evaluate the position of tubes and their function.
Emergency surgery may be needed to repair the damage caused by the wound.
Throughout treatment, monitor central venous pressure and blood pressure to detect hypovolemia, and assess vital signs. Provide analgesics as appropriate. Tetanus and antibiotic prophylaxis may be necessary.
Reassure the patient. Report the incident to the police in accordance with local laws. Help contact the patient’s family, and offer them reassurance as well.
ABDOMEN
Blunt and penetrating abdominal injuries
Blunt and penetrating abdominal injuries may damage major blood vessels and internal organs. Their most immediate life-threatening consequences are hemorrhage and hypovolemic shock; later threats include infection. The prognosis depends on the extent of the injury and the specific organs damaged, but it’s usually improved by prompt diagnosis and surgical repair.
CAUSES AND INCIDENCE
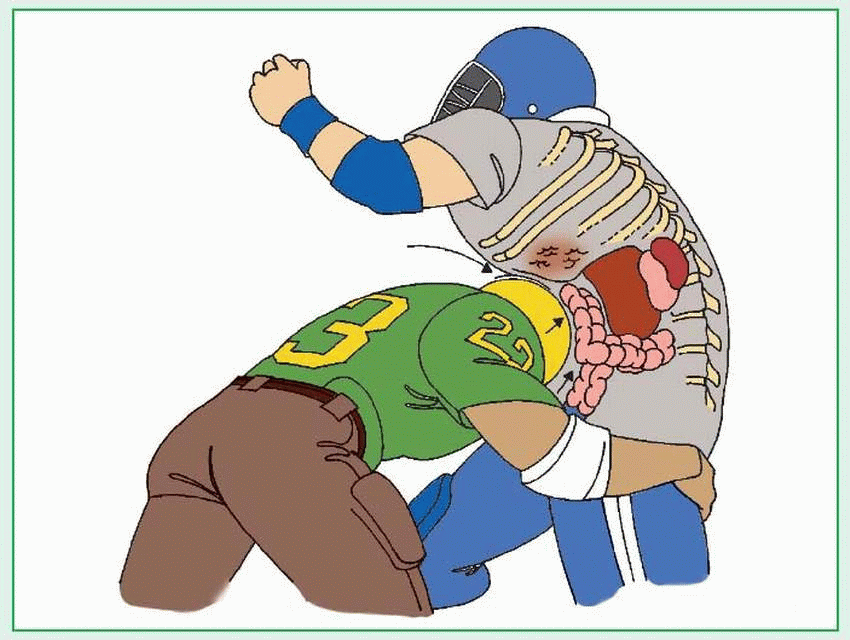
Blunt (nonpenetrating) abdominal injuries usually result from automobile accidents, falls from heights, or sports injuries; penetrating abdominal injuries, from stab and gunshot wounds.
The most commonly injured organs associated with penetrating abdominal trauma are the small intestine (29%), liver (28%), and colon (23%). Penetrating abdominal trauma affects 35% of those admitted to urban trauma centers and 1% to 12% of those admitted to suburban and rural centers.
COMPLICATIONS
Hemorrhage
Hypovolemic shock
Infection
Dysfunction of major organs such as liver, spleen, pancreas, and kidneys
SIGNS AND SYMPTOMS
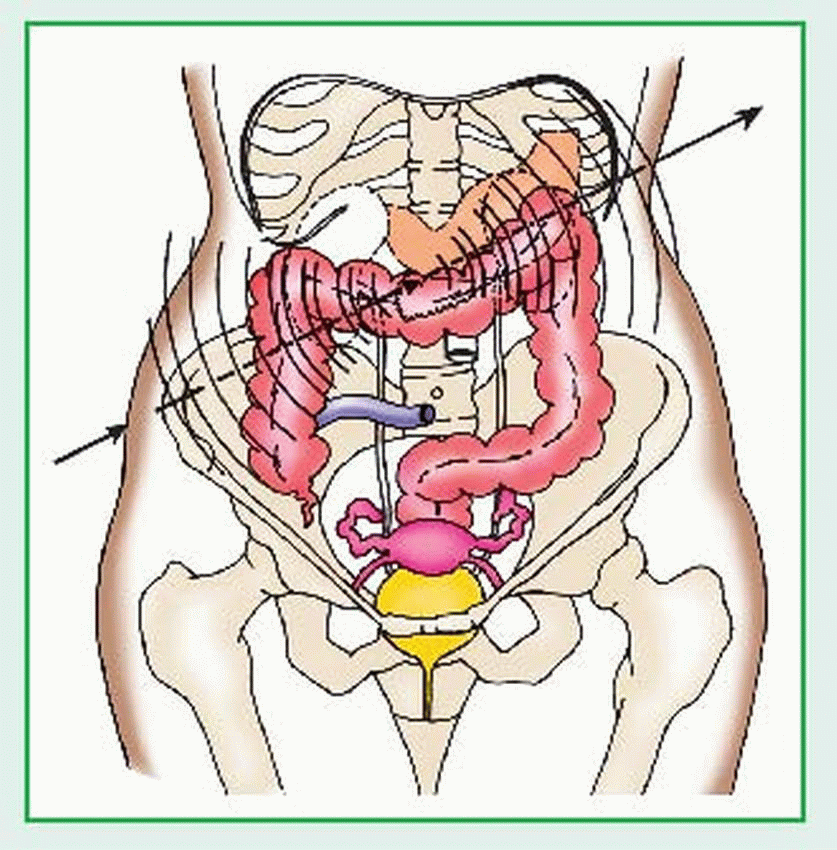
Symptoms vary with the degree of injury and the organs damaged. Penetrating abdominal injuries cause obvious wounds (gunshots commonly produce both entrance and exit wounds) with variable blood loss, pain, and tenderness. They commonly result in pallor, cyanosis, tachycardia, shortness of breath, and hypotension. (See Projectile pathway.) Blunt abdominal injuries cause severe pain (which may radiate beyond the abdomen to the shoulders), bruises, abrasions, contusions, or distention. They may also result in tenderness, abdominal splinting or rigidity, nausea, vomiting, pallor, cyanosis, tachycardia, and shortness of breath. Rib fractures commonly accompany blunt injuries. (See Effects of blunt abdominal trauma.)
In both blunt and penetrating injuries, massive blood loss may cause hypovolemic shock. Damage to solid abdominal organs (liver, spleen,
pancreas, and kidneys) generally causes hemorrhage. Damage to hollow organs (stomach, intestine, gallbladder, and bladder) causes rupture and release of the organs’ contents (including bacteria) into the abdomen, which in turn produces inflammation and, possibly, infection.
pancreas, and kidneys) generally causes hemorrhage. Damage to hollow organs (stomach, intestine, gallbladder, and bladder) causes rupture and release of the organs’ contents (including bacteria) into the abdomen, which in turn produces inflammation and, possibly, infection.
DIAGNOSIS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree