2 Transfusion of blood components and plasma products
Blood components
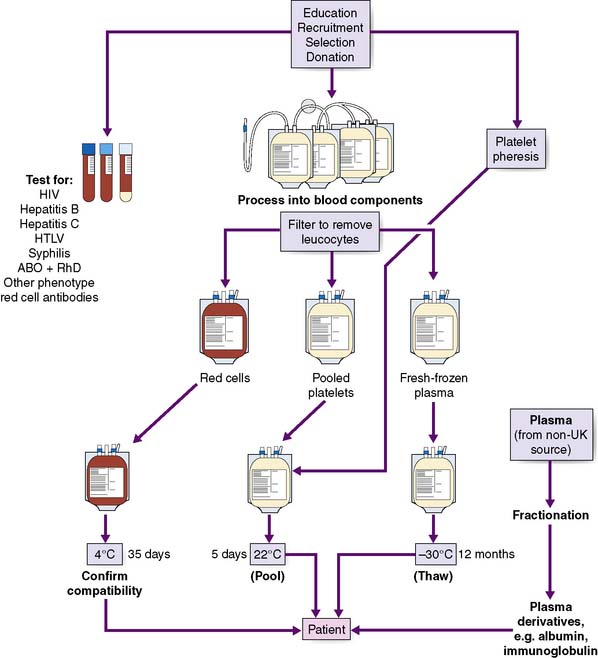
The components that can be prepared from donated blood are shown in Figure 2.1 and their descriptions follow.
Plasma products
Human albumin
Solutions of 4.5 or 5% are used to maintain plasma albumin levels in conditions where there is increased vascular permeability, e.g. burns, and are sometimes used in acute blood volume replacement, although crystalloid or non-plasma colloid solution would be the recommended first-line volume expander. Randomized controlled trials on the use of albumin suggest that there is no clear advantage from the use of albumin solutions in the treatment of hypovolaemia over judicious use of saline or colloid solutions. Resuscitation with crystalloid requires volumes of fluid three times greater than with colloid (see chapter 7).
Immunoglobulin preparations (90% IgG)
These are prepared from fractionation of large pools of plasma from unselected donors or from individuals known to have high levels of specific antibodies. Some products are administered intramuscularly. The indications for some of the more commonly used immunoglobulins are shown in Table 2.1 e.g. hyperimmune globulin against hepatitis B, herpes zoster, tetanus and RhD. Intravenous IgG was originally developed as replacement therapy for immunodeficiency states, but is also used to treat immune thrombocytopenia and other rare diseases such as Guillain–Barré syndrome.
Table 2.1 Indications and doses for the most commonly used specific immunoglobulins
| Problem | Patients eligible for IgG | Preparation | Dose |
|---|---|---|---|
| Hepatitis B | Needle-stick or mucosal exposure victims Should also be immunized | Hepatitis B IgG | 1000 iu for adults and 500 iu for children < 5 years |
| Tetanus-prone wounds | Non-immune patients with heavily contaminated wounds Toxoid should be administered with IgG | Tetanus IgG | 250 iu routine prophylaxis 500 iu if > 24 h since injury or heavily contaminated wound |
Red cell serology
ABO antigens
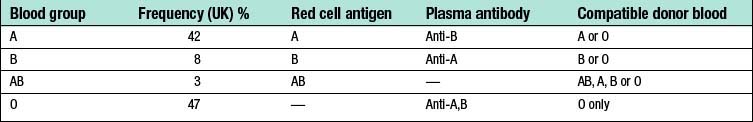
Nearly all deaths from transfusion error are due to ABO-incompatible transfusion. ABO are carbohydrate antigens present on the majority of cells of the body. Their presence depends on the pattern of inheritance of genes encoding glycosyltransferases. Since carbohydrate antigens are widely expressed by other organisms including bacteria, individuals who lack A or B antigens will produce anti-A and anti-B antibodies, respectively. These are usually IgM antibodies (naturally occurring) and are present from the age of 3–6 months. ABO antibodies can react at body temperature and activate complement, and are of major clinical significance as a cause of rapid intravascular haemolysis. For example, transfusion of group A blood to a group B patient results in haemolysis of the transfused red cells because of the anti-A antibodies present in the recipient. Similarly, group O individuals have both anti-A and anti-B antibodies in their plasma that will react with any red cells apart from group O (Table 2.2). Group O blood (Universal donor) can be used in the majority of recipients because it will not be destroyed by anti-A or anti-B antibodies and because processing removes most of the plasma from the unit and hence reduces the donor antibodies contained within.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree