Chapter 37 Thyroid hormones, antithyroid drugs
• Thyroid hormones (thyroxine/levothyroxine T4, liothyronine T3).
• Use of thyroid hormone: treatment of hypothyroidism.
• Antithyroid drugs and hyperthyroidism: thionamides, drugs that block sympathetic autonomic activity, iodide and radio-iodine 131I, preparation of patients for surgery, thyroid storm (crisis), exophthalmos.
• Drugs that cause unwanted hypothyroidism.
Thyroid hormones
L-Thyroxine (T4 or tetra-iodo-l-thyronine) and lio-l-thyronine (T3 or tri-iodo-l-thyronine) are the natural hormones of the thyroid gland. T4 is a less active precursor of T3, which is the major mediator of physiological effect. In this chapter, T4 for therapeutic use is referred to as levothyroxine (the rINN; see p. 69).
Levothyroxine for hypothyroidism
Levothyroxine is used in some countries for the treatment of non-toxic nodular goitre, on the assumption that nodular thyroid tissue growth is dependent on TSH. The treatment is not curative. Levothyroxine should not be used to treat obesity (see Obesity, p. 602).
Antithyroid drugs and hyperthyroidism
Drugs used for the treatment of hyperthyroidism include:
• Thionamides, which block the synthesis of thyroid hormone.
• Iodine: radioiodine, which destroys the cells that make thyroid hormone; iodide, an excess of which reduces the production of thyroid hormone temporarily (it is also necessary for the formation of hormone, and both excess and deficiency can cause goitre).
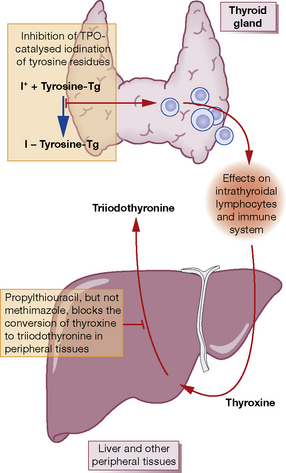
Thionamides (thiourea derivatives) carbimazole, methimazole, propylthiouracil
Mode of action (Fig. 37.1)
Propylthiouracil
(PTU) differs from other members of the group in that it also inhibits peripheral conversion of T4 to T3, but only at high doses used in treatment of thyroid storm (see p. 594). PTU differs from the other thionamides in its apparent radio-protective effect when used prior to radioiodine treatment.
Doses
• Carbimazole 40 mg total/day is given orally (or methimazole 30 mg) until the patient is euthyroid (usually 4–6 weeks). Then either titrate (titration regimen) by decrements initially of 10 mg every 4–6 weeks to a maintenance dose of 5–10 mg/day, or continue (block–replace regimen) 40 mg once daily, and add levothyroxine 100 micrograms/day, with monitoring of free T4 and TSH.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree