Blood supply
The intercostal, subcostal and lumbar arteries pass forward in the neurovascular plane (see p. 11) to supply the flanks; the internal thoracic and the superior and inferior epigastric arteries supply the ventral midline tissues. From all these arteries cutaneous branches pass to the superficial fat and skin. The venous return from the subcutaneous tissue does not follow the arteries. The blood is collected by an anastomosing network of veins that radiate away from the umbilicus. Below this level they pass to the great saphenous vein in the groin; above the umbilicus they run up to the lateral thoracic vein and so to the axillary vein. From the umbilicus a few paraumbilical veins accompany the ligamentum teres and drain to the left branch of the portal vein; they may distend in portal obstruction, giving rise, if the distension spreads to the subcutaneous veins, to a pattern of dilated veins around the umbilicus, the caput Medusae. A longitudinal channel, the thoracoepigastric vein uniting the lateral thoracic vein with the superficial epigastric vein above the inguinal ligament, provides a communication between superior and inferior venae cavae and often becomes prominent in cases of obstruction of the inferior vena cava.
Lymph drainage
Lymphatic channels from the subcutaneous tissue and skin follow the veins to axillary and superficial inguinal nodes. From above the level of the umbilicus, lymph from the front of the body goes to the anterior (pectoral) group and from the back of the body to the posterior (scapular) group of axillary nodes. From the umbilicus downwards lymph from the anterior aspect of the abdominal wall and perineum goes to the medial group and from the lateral and posterior aspects of the abdominal wall to the lateral group of superficial inguinal nodes.
Nerve supply
Above the second rib and the manubriosternal joint the skin is supplied by supraclavicular branches of the cervical plexus (C4; see Fig. 1.7, p. 12). Below this level a midline and paramedian strip of skin is supplied by the anterior cutaneous branches of the spinal nerves from T2 to L1; the skin in the upper epigastric region is supplied by T7, in the umbilical region by T10 and suprapubic skin by L1. A broad lateral strip is supplied by the lateral cutaneous branches of the spinal nerves from T2 or 3 to L1; these branches emerge in the midaxillary line. The lateral cutaneous branches of T12 and the iliohypogastric nerve descend over the iliac crest to also supply the skin of the buttock. The ilioinguinal nerve has no lateral cutaneous branch; it is the collateral branch of the iliohypogastric, both coming from L1 nerve. A posterior strip of skin is innervated by the posterior rami of spinal nerves, by their medial branches in the upper thoracic and their lateral branches in the lower thoracic and lumbosacral parts (see Fig. 1.6, p. 12).
Part two. Thoracic wall and diaphragm
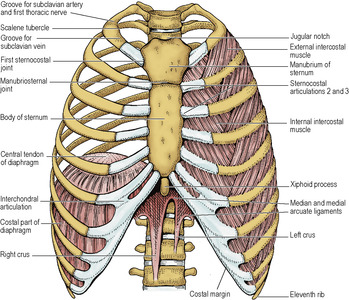
The skeleton of the thoracic wall consists of the 12 thoracic vertebrae, the 12 pairs of ribs and costal cartilages and the sternum. The thoracic cavity is roofed in above the lung apices by the suprapleural membrane and is floored by the diaphragm. The floor is highly convex (domes of the diaphragm), so that when the diaphragm is relaxed in expiration the volume of the thoracic cavity is much less than inspection of the bony cage would suggest. The liver and spleen and the upper parts of the stomach and both kidneys lie in the abdominal cavity wholly or partly covered by ribs.
At the back the ribs articulate with the vertebral column in two places: by their heads (joints of costal heads) and by their tubercles (costotransverse joints). Collectively these form the costovertebral joints. At the front the ribs join their costal cartilages (costochondral joints). The upper seven costal cartilages articulate with the sternum at the sternocostal joints, the next three articulate with each other (interchondral joints) and the eighth articulates with the seventh costal cartilage to complete the costal margin; the last two costal cartilages have free ends. The manubriosternal joint is a symphysis between the manubrium and body of the sternum, and the xiphisternal joint is a symphysis between the body and the xiphoid process.
Joints of costal heads
The head of a typical rib possesses two articular facets that slope away from each other, separated by a ridge. Each facet makes a small synovial joint with a demifacet of a vertebral body; the lower rib facet with the upper costal facet of its own vertebra, and the upper facet with the lower costal facet of the vertebra above (Fig. 4.2). The ridge between the two is attached to the intervertebral disc by the intra-articular ligament. The front of the joint capsule is reinforced by the radiate ligament which consists of three bands. The upper band passes to the body of the vertebra above, the lower band to the vertebra below, while the central band runs horizontally, deep to the anterior longitudinal ligament, and blends with the intervertebral disc. The first rib articulates with T1 vertebra only, never coming into contact with C7, and the last two ribs also articulate only with their own vertebrae.
Costotransverse joints
The tubercle of a typical rib (p. 218) has two facets. The medial facet, covered with hyaline cartilage, articulates with a facet near the tip of the transverse process of its own vertebra at a small synovial joint. The lateral facet (non-articular) gives attachment to the lateral costotransverse ligament which runs to the tip of the transverse process and is one of three ligaments helping to stabilize the joint. The other two are the costotransverse ligament, which occupies the space between the back of the neck of the rib and the front of the transverse process, and the superior costotransverse ligament, which passes as two laminae from the crest of the neck of the rib to the undersurface of the transverse process of the vertebra above (Fig. 4.2). The anterior lamina is continuous with the posterior intercostal membrane; the posterior is in the same plane as the external intercostal muscle. The fibres of these two laminae are at right angles to each other, in a similar manner to the fibres of the intercostal muscles. The lower two ribs do not possess tubercles and make no synovial joints with transverse processes.
Costochondral joints
Every rib makes with its costal cartilage a primary cartilaginous joint. The costal cartilage represents no more than the unossified anterior part of a rib.
Interchondral joints
Adjacent surfaces of costal cartilages 6 and 7, 7 and 8, and 8 and 9 are joined to each other by small synovial joints; 9 and 10 are connected by ligamentous fibres.
Sternocostal joints
The first costal cartilage articulates with the manubrium by a primary cartilaginous joint. Thus the manubrium and the first ribs are fixed to each other and move together as one.
The next six costal cartilages each articulate with the sternum by a synovial joint—a single cavity except in the case of the second, which articulates with the manubrium and body (Fig. 4.3).
Manubriosternal joint
At this symphysis between the manubrium and body of the sternum, the surfaces are covered by hyaline cartilage and there is an intervening disc of fibrocartilage which may become ossified in the elderly. Sometimes (30%) cavitation appears in the disc so that the joint may appear to be synovial, but this is simply a degenerative change that does not alter the fact that the joint is a symphysis.
Xiphisternal joint
This is another symphysis, between the body of the sternum and the xiphoid process. Ossification from middle age onwards is common.
Thoracic muscles
The muscles of the thoracic wall lie in the same three morphological layers as those of the abdominal wall (see p. 221), but in the thoracic region they have become divided up by the presence of ribs. They are innervated segmentally by anterior rami. In the outer thoracic layer the external intercostal muscles correspond to the external oblique in the abdomen and in the middle layer the internal intercostals correspond to the internal oblique. The inner layer is broken up into three muscles, the subcostals, innermost intercostals and the transversus thoracis. This incomplete layer corresponds to the transversus abdominis. Between it and the middle layer is the neurovascular plane, continuous with that of the abdominal wall; in it run intercostal vessels and nerves, with their collateral branches (see Fig. 1.5, p. 11).
Outer layer
Two small muscles of the external layer have migrated posteriorly, and lie on the surface of the erector spinae mass. They are the posterior serratus muscles and are supplied by anterior rami. Each arises from four spinous processes, two in the thorax and two beyond it, and each is inserted into four ribs.
Serratus posterior superior arises from the spinous processes of the lowest two cervical and the upper two thoracic vertebrae and is inserted just lateral to the angles of ribs 2–5. Many tendinous fibres in the sheet of muscle give it a characteristic glistening appearance which provides a useful landmark in exposures of this region. The dorsal scapular nerve and vessels run down on the posterior surface of the muscle, between it and the rhomboids (see Fig. 2.5, p. 41).
Serratus posterior inferior arises from the lower two thoracic and the upper two lumbar spinous processes and is inserted just lateral to the angles of the lowest four ribs.
The serratus posterior muscles are weak muscles of respiration. The superior muscle elevates the upper ribs (inspiration) while the inferior muscle depresses the lower ribs (expiration).
Although morphologically associated with the muscles of the back (see p. 428), the levator costae muscles are functionally classified as thoracic muscles. Each one of each of the 12 pairs is fan-shaped, spreading down from the tip of a transverse process (from C7 to T11 vertebra) to be inserted into the upper border of the rib below, lateral to its tubercle (see Fig. 6.82, p. 429), and presumably helps to elevate it. They are supplied by the posterior rami of spinal nerves (from C8 to T11).
The chief muscles of the outer layer are the external intercostals. The fibres of the external intercostal muscles pass obliquely downwards and forwards from the sharp lower border of the rib above to the smooth upper border of the rib below. Each muscle extends from the superior costotransverse ligament at the back of the intercostal space as far forwards as the costochondral junction; here it is replaced by the anterior intercostal membrane (see Fig. 1.5, p. 11). This extends to the side of the sternum. Between the bony ribs is muscle; between the costal cartilages is membrane.
Middle layer
This consists of the internal intercostal muscles. The fibres run downwards and backwards, from the costal groove to the upper border of the rib below (Fig. 4.4). Each muscle, unlike an external intercostal, extends as far forwards as the side of the sternum; it is replaced posteriorly by the posterior intercostal membrane, which extends from the angle of the rib to the superior costotransverse ligament at the posterior limit of the space (see Fig. 1.5, p. 11).
Inner layer
Of the three groups of muscles in this layer the innermost intercostals line the rib cage at the side, while the subcostals are at the back, and the transversus thoracis at the front. They cross more than one intercostal space.
Lying in the paravertebral gutter are the subcostal muscles attached to the inner surfaces of ribs. They are separated from the posterior border of the innermost intercostals by a space across which the intercostal nerves and vessels are in contact with the parietal pleura.
The innermost intercostal muscles (intercostales intimi) are attached to the inner surfaces of ribs on the lateral part of the thoracic wall.
Transversus thoracis arises from the posterior surface of the lower part of the sternum, whence digitations diverge on each side to the second to the sixth costal cartilages. This muscle was formerly called sternocostalis, which was a more exact name. The transversus thoracis group is the best inclusive name for all three muscles of the inner layer because it conforms with the transversus abdominis muscle.
Intercostal spaces
The intercostal spaces (between the ribs) are filled in by the muscles of the three layers described above. Running in the plane between the intermediate and inner layers are the intercostal nerves and vessels (Fig. 4.4). The vein, artery and nerve lie in that order from above downwards, under cover of the downward projection of the lower border of the rib. Thus a needle or trocar for pleural drainage (see p. 213) is inserted just above the rib that forms the lower boundary of the space, in order to avoid the main nerve and vessels that are at its upper boundary. The collateral branches of nerve and vessels that run along the upper border of a rib are small and can be ignored. A needle introduced to deliver an anaesthetic solution on an intercostal nerve is inserted just below the lower border of a rib.
Intercostal nerves
The mixed spinal nerve, having emerged from the intervertebral foramen and given off its posterior ramus, passes around in the neurovascular plane, between the internal intercostal and the transversus thoracis group of muscles (see Fig. 1.5, p. 11). This intercostal nerve gives off a collateral and a lateral cutaneous branch before it reaches the costal angle. The collateral branch runs along the inferior border of its space and supplies the muscles of the space, the parietal pleura and the periosteum of the ribs. The lateral cutaneous branch pierces the intercostal muscles and the overlying muscles of the body wall along the midaxillary line, and divides into an anterior and posterior branch to supply skin over the space. The intercostal nerve ends as an anterior cutaneous nerve, which in the upper six spaces passes anterior to the internal thoracic artery and pierces the intercostal muscles to reach the skin. In its course around the space the intercostal nerve lies below the vein and artery, but in its course around the body wall the main nerve lies in a wider circle that embraces the narrower circle of the vessels. Hence, at the back of the intercostal space where the nerve crosses the intercostal artery, the nerve lies behind the artery; at the front of the space the nerve crosses in front of the internal thoracic artery.
The lower five intercostal nerves and their collateral branches slope downwards behind the costal margin into the neurovascular plane of the abdominal wall, which they supply (see p. 224).
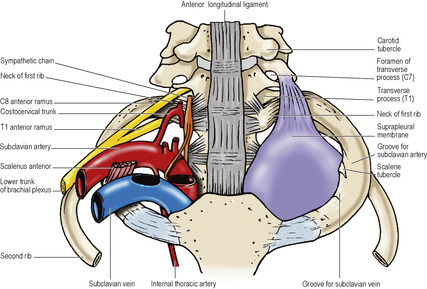
The anterior ramus of T1 ascends across the neck of the first rib to enter the brachial plexus. Before it does so it gives off the small first intercostal nerve, which courses around beneath the flat inferior surface of the first rib (see Fig. 6.9B, p. 347) and supplies the intercostal muscles of the first space, the adjacent pleura and rib periosteum. The lateral cutaneous branch of the second intercostal nerve crosses the axilla to the medial side of the arm as the intercostobrachial nerve (see p. 61).
The subcostal nerve (twelfth thoracic), although arising in the thorax, quickly leaves by passing behind the lateral arcuate ligament of the diaphragm into the abdomen, below the subcostal artery and vein.
Intercostal arteries
Arteries enter intercostal spaces at the back and front. At the back the upper two spaces are supplied by the superior intercostal artery. This is the descending branch of the costocervical trunk, which comes off from the second part of the subclavian artery behind scalenus anterior. It enters the thorax by passing across the front of the neck of the first rib; here it has the sympathetic trunk on its medial side, while the first thoracic nerve passes laterally across the first rib to join the brachial plexus (Fig. 6.9B). The small first posterior intercostal vein lies between the artery and the sympathetic trunk. At this point the first thoracic sympathetic ganglion is frequently fused with the inferior cervical ganglion to form the cervicothoracic (stellate) ganglion.
The remaining nine intercostal spaces are supplied each with a separate branch of the descending thoracic aorta; the nine right branches cross the front of the vertebrae and anterior longitudinal ligaments, behind the hemiazygos veins and thoracic duct. All 11 pairs of arteries constitute the posterior intercostal arteries. Each artery gives off a small collateral branch, which passes around in the neurovascular plane at a lower level than the main trunk.
At the front of the intercostal space the internal thoracic artery in the upper six spaces and the musculophrenic artery in the seventh, eighth and ninth spaces give off two anterior intercostal arteries that pass backwards and anastomose with the posterior vessels. There are no anterior intercostal arteries in the last two spaces.
Intercostal veins
In each space there are one posterior and two anterior intercostal veins, accompanying the arteries of the same names. The anterior veins drain into the musculophrenic and internal thoracic veins. The posterior veins are not regular. In the lower eight spaces they drain into the azygos system: the azygos vein on the right and the hemiazygos and accessory hemiazygos on the left. The first posterior intercostal vein opens either into the vertebral vein or the brachiocephalic vein of its own side. The second and third posterior intercostal veins, and sometimes the fourth, form a single trunk on each side, the superior intercostal vein. That on the right drains simply into the azygos vein (Fig. 4.12). That on the left runs forward over the arch of the aorta, lateral to the vagus nerve and medial to the phrenic nerve, to empty into the left brachiocephalic vein (Fig. 4.13).
Lymph drainage
The lymph vessels of the intercostal spaces follow the arteries. From the front of the space vessels pass to the anterior intercostal (parasternal) nodes that lie along the internal thoracic artery; from the back of the space they drain to posterior intercostal nodes.
Internal thoracic artery
From the first part of the subclavian artery, the internal thoracic artery (formerly the internal mammary) passes vertically downwards about 1cm lateral to the border of the sternum (Fig. 4.5). It gives off two anterior intercostal arteries in each intercostal space. At the costal margin it divides into the superior epigastric and musculophrenic arteries. The former passes between the xiphisternal and highest costal fibres of the diaphragm to enter the rectus sheath behind the muscle. The latter passes along the costodiaphragmatic gutter and gives off two anterior intercostal arteries in each space till it ends by piercing the diaphragm in the ninth space to ramify on its abdominal surface. The internal thoracic artery is accompanied by two venae comitantes that empty into the brachiocephalic vein.
The artery gives off a pericardiacophrenic branch that runs with the phrenic nerve and supplies branches to the nerve itself, pleura and fibrous and parietal pericardium.
Perforating branches emerge towards the surface from each intercostal space. They are especially large in the second, third and fourth spaces of the female for supply of the breast. Thus the internal thoracic artery supplies the anterior body wall from the clavicle to the umbilicus.
Suprapleural membrane
This is a rather dense fascial layer (Sibson’s fascia) attached to the inner border of the first rib and costal cartilage and the transverse process of C7 vertebra (Fig. 4.5). It is not attached to the neck of the first rib. It has the cervical dome of the pleura attached to its undersurface, and when traced medially it is found to thin out and disappear into the mediastinal pleura. It lies in the oblique plane of the thoracic inlet, and the subclavian vessels arch upwards and laterally over it. The membrane gives rigidity to the thoracic inlet and prevents the neck structures being ‘puffed’ up and down during respiration. Damage to the suprapleural membrane during surgical procedures at the root of the neck will usually result in the development of a pneumothorax on the same side.
Diaphragm
The diaphragm is a domed fibromuscular sheet that separates the thoracic and abdominal cavities. Its purpose is essentially for inspiration.
Morphologically the diaphragm is a derivative of the inner (transversus) layer of the muscles of the body wall, and its fibres arise in continuity with those of transversus abdominis from within the costal margin. It is completed behind the costal origin by fibres that arise from the arcuate ligaments and the crura. From the circumference of this oval origin the fibres arch upwards into a pair of domes and then descend to a central tendon which lies at the level of the xiphisternal joint. Viewed from in front the diaphragm curves up into right and left domes. The right dome of the diaphragm is higher than the left, ascending in full expiration as high as the nipple (fourth space), while the left dome reaches the fifth rib.
Viewed from the side the profile of the diaphragm resembles an inverted J, the long limb extending up from the crura (upper lumbar vertebrae) and the short limb attached to the xiphisternum (level of T8 vertebra). Viewed from above the outline is kidney shaped, in conformity with the oval outline of the body wall which is indented posteriorly by the vertebral column (see Fig. 1.5, p. 11).
The crura are strong tendons attached to the anterolateral surfaces of the bodies of the upper lumbar vertebrae. The right crus is fixed to the upper three lumbar vertebrae and the intervening discs; the left crus likewise to the upper two lumbar vertebrae. Muscle fibres radiate from each crus, overlap, and pass vertically upwards before curving forwards into the central tendon. Some of the fibres of the right crus pass up on the abdominal surface of fibres from the left crus and surround the oesophageal orifice in a sling-like loop (Fig. 4.6; see also Fig. 5.26, p. 251). Tendinous fibres from the medial edge of each crus unite with one another in front of the aorta at the level of T12 vertebra to form the median arcuate ligament. The medial arcuate ligament is a thickening in the psoas fascia. It extends from the side of the body of L1 or L2 vertebra to a ridge on the anterior surface of the transverse process of L1 vertebra, at the lateral margin of psoas. From here the lateral arcuate ligament extends across to the middle of the lower margin of the twelfth rib; it is a thickening in the anterior layer of the lumbar fascia on the front of quadratus lumborum. Further laterally a digitation arises from the internal surfaces of each of the lower six costal cartilages and ribs, interdigitating with the slips of origin of transversus abdominis. In front, the diaphragm arises from the back of the xiphisternum.
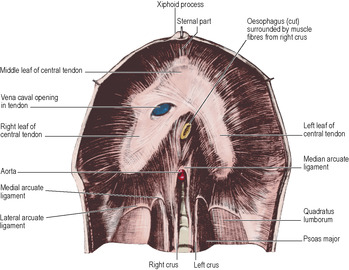 |
| Figure 4.6 |
The central tendon has a trefoil shape, having an anteriorly situated middle leaf fused on each side to lateral leaves that extend back towards the paravertebral gutters. The tendon is inseparable from the fibrous pericardium, both having the same embryological origin.
Openings in the diaphragm
For the passage of structures between thorax and abdomen there are three large openings in the diaphragm and several smaller ones.
The aortic opening is opposite T12 vertebra, in the midline, behind the median arcuate ligament. It transmits the aorta with the azygos vein to the right and the thoracic duct leading up from the cisterna chyli between them.
The oesophageal opening is opposite T10 vertebra, usually 2.5cm to the left of the midline behind the seventh left costal cartilage. It lies in the fibres of the left crus, but a sling of fibres from the right crus loop around it. The transversalis fascia on the undersurface of the diaphragm extends up through the opening, blends with the endothoracic fascia above the diaphragm, and is attached to the oesophagus about 2–3cm above the oesophagogastric junction. This fascial cone is the phreno-oesophageal ligament. It becomes stretched in the ‘sliding’ type of hiatus hernia (see p. 187). The vagal trunks and the oesophageal branches of the left gastric artery, veins and lymphatics accompany the oesophagus as it passes through the diaphragm. The venous drainage from this site passes caudally to the portal venous system and cranially to the azygos venous system, constituting a major site of portal–systemic anastomosis.
The vena caval foramen is opposite T8 vertebra just to the right of the midline, behind the sixth right costal cartilage. It lies between the middle and right leaves of the central tendon, the fibres of which fuse firmly with the adventitial wall of the inferior vena cava (Fig. 4.12). The right phrenic nerve passes through the central tendon alongside the inferior vena cava at this opening.
Other structures make their own smaller openings. The hemiazygos vein passes through the left crus. The greater, lesser, and least splanchnic nerves pierce each crus. The sympathetic trunk passes behind the medial arcuate ligament. The subcostal nerve and vessels pass behind the lateral arcuate ligament. The left phrenic nerve pierces the muscle of the left dome. The neurovascular bundles of the seventh to the eleventh intercostal spaces pass between the digitations of the diaphragm and transversus abdominis into the neurovascular plane of the abdominal wall. The superior epigastric vessels pass between the xiphisternal and costal (seventh) fibres of the diaphragm. Extraperitoneal lymph vessels on the abdominal surface pass through the diaphragm to lymph nodes lying on its thoracic surface, mainly in the posterior mediastinum.
At the posterior part of the diaphragm there may be a gap between the lowest costal fibres and those arising from the lateral arcuate ligament. The posterior surface of the kidney and its perirenal fascial covering is then separated from the pleura only by areolar tissue of the endothoracic fascia.
Blood supply
The costal margin of the diaphragm is supplied by the lower five intercostal and the subcostal arteries. The main mass of fibres rising up from the crura are supplied on their abdominal surface by right and left inferior phrenic arteries from the abdominal aorta (see Fig. 5.43, p. 275). The pericardiacophrenic and musculophrenic branches of the internal thoracic artery and the superior phrenic branches of the thoracic aorta make small contributions to the blood supply of the diaphragm.
Nerve supply
The motor nerve supply is solely from the phrenics (C3, 4, 5 but predominantly C4). Each half of the diaphragm is supplied by its own phrenic nerve and the fibres of the right crus that loop to the left around the oesophageal opening are supplied by the left phrenic. The lower intercostal nerves give proprioceptive fibres to the periphery of the diaphragm, proprioceptive supply to the central part coming from the phrenics. On reaching the abdominal surface of the diaphragm, both nerves divide into anterior, lateral and posterior branches which run radially, giving off branches that enter the muscle from below.
Associated with a lifetime of constant activity, about 55% of diaphragmatic muscle fibres (and 65% of intercostal muscle fibres) are of the slow twitch fatigue- resistant variety.
Actions
The major role of the diaphragm is inspiratory, but it is used also in abdominal straining.
Inspiration. When the fibres contract in tranquil inspiration only the domes descend; this sucks down the lung bases and does not disturb the mediastinum. In a deeper breath further descent of the domes, below the level of the central tendon, can depress the central tendon from T8 to T9 level. This stretches the mediastinum (traction on pericardium and great vessels) and no further descent of the tendon is possible. Further contraction of the muscle (maximum inspiration) now everts the ribs of the costal margin in a ‘bucket handle’-like movement with widening of the subcostal angle.
As the diaphragm contracts intra-abdominal pressure tends to rise, and the vena caval foramen (in the central tendon) is pulled widely open to assist venous return via the inferior vena cava. The oesophageal opening is held closed by the pinch-like action resulting from contraction of the muscle sling of the right crus, to discourage regurgitation of stomach contents. The aortic opening is unaffected.
Hiccup is a (repeated) spasmodic contraction of the diaphragm, its contraction being followed immediately by closure of the glottis and subsequent release of the trapped air to produce the characteristic sound.
Expiration. Whether expiration is tranquil or forced (coughing, sneezing, blowing, etc.) the diaphragm is wholly passive, its relaxed fibres being elongated by pressure from below.
Abdominal straining. For evacuation of a pelvic effluent (defecation, micturition, parturition) diaphragmatic contraction aids that of the abdominal wall in raising intra-abdominal pressure. It is much weaker than the powerful obliques, transversus and recti, so for maximum pressure a deep breath is taken, the glottis is closed and the diaphragm is prevented from undue elevation by being held down by a cushion of compressed air. Forcible escape of some of this air causes the characteristic grunt.
During heavy lifting in the stooping position abdominal straining is beneficial. With the breath held and intracoelomic pressure raised as above, the vertebral column cannot easily flex; it is as though an inflated football filled the body from pelvic brim to thoracic inlet. The weight of the stooping trunk is supported on the football, freeing erector spinae to use all its power to lift the weight. Such acts are similarly accompanied on occasion by the characteristic grunt.
Development
The diaphragm develops from four sources. The septum transversum (p. 24) gives rise to most of the central tendon. Prior to its descent from the neck the transverse septum becomes invaded by muscle cells derived from the third, fourth and fifth cervical myotomes. The muscle cells carry their own nerve supply with them, hence the motor supply from the phrenic nerves. Mesodermal folds, the pleuroperitoneal membranes, which close the connection between the thoracic and abdominal parts of the coelom, and the oesophageal mesentery also contribute to the development of the diaphragm. Failure of pleuroperitoneal membrane development is the most common cause of congenital diaphragmatic hernia. The defect (Bochdalek’s foramen) is posteriorly placed and clinically manifests more often on the left side, probably due to the presence of the liver on the right side. Another possible but smaller hernial site is at the junction of the costal and xiphoid origins—Morgagni’s foramen.
Diaphragmatic hernia
The congenital types of diaphragmatic hernia have just been mentioned. Of the acquired varieties, the most common is the sliding type of hiatus hernia, through the oesophageal opening. Here the oesophagogastric junction rises up into the thorax; this encourages gastro-oesophageal reflux. In the much rarer paraoesophageal (rolling) type, the oesophagogastric junction remains in the abdomen, but a pouch of peritoneum containing a part of the stomach projects upwards alongside the oesophagus; this compresses the lower oesophagus and the blood supply of the herniated stomach may be compromised.
Thoracic movements and respiration
The diaphragm is the main muscle of inspiration. The external intercostals are most active in inspiration and the internal intercostals in expiration, but the intercostals are more important for stiffening of the chest wall and preventing paradoxical movement of the interspaces. In expiration, elastic recoil of the lungs assisted by contraction of the muscles of the abdominal wall makes the relaxed diaphragm regain its domed form.
During maximal inspiratory efforts, other muscles too are active. The scalene muscles and sternocleidomastoid elevate the first rib and manubrium. The twelfth rib is fixed by quadratus lumborum and may even descend. The erector spinae extend the spine, and muscles connecting the trunk to the upper limbs, such as pectoralis major, contribute to chest expansion when the arms are fixed. In forced expiratory efforts, latissimus dorsi contracts, compressing the lower ribs.
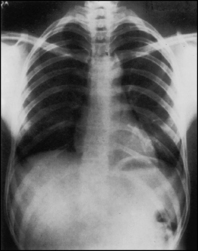
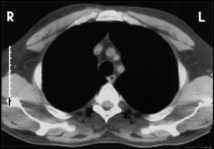
All three diameters of the thorax—anteroposterior, transverse and vertical—are increased during inspiration. The anteroposterior diameter increases because the sternum moves forwards as the ribs are raised since their anterior ends are at a lower level than their heads (see Fig. 4.33, p. 218). This sternal movement is facilitated by the hinge movement (up to about 7°) at the manubriosternal joint. If this joint becomes ankylosed, thoracic expansion due to sternocostal movement is virtually lost (as in emphysema) and only diaphragmatic respiration is possible. As each rib forms the arc of a circle, which is larger than that formed by the rib above, elevation of the ribs during inspiration increases the transverse diameter of the thorax. Change in the vertical extent of the thoracic cavity is due to diaphragmatic movement (Figs 4.7 and 4.8).
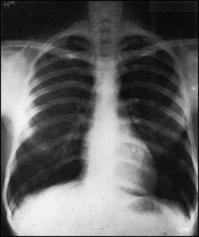 |
| Figure 4.8 Radiograph of the same thorax as in Figure 4.7 taken in full inspiration. The anterior ends of the ribs are elevated and the lower ribs everted. The descent of the domes of the diaphragm is greater than that of the central tendon. |
Movements of the abdominal wall
Since the volume of the abdominal cavity remains constant, the abdominal wall moves in accordance with changes in the thoracic cavity. Diaphragmatic inspiration and rib inspiration occur simultaneously, but each in itself produces opposite movements in the abdominal wall. In purely diaphragmatic breathing, with the ribs motionless, descent of the diaphragm is accompanied by passive protrusion of the relaxed abdominal wall. Ascent of the diaphragm is accompanied by retraction of the abdominal wall; indeed, it is the active contraction of the abdominal wall muscles that forces the relaxed diaphragm up. This to-and-fro movement of the abdominal wall is usually called ‘abdominal respiration’.
In ‘thoracic respiration’ the movements of the abdominal wall are purely passive. When the ribs are elevated in inspiration the diaphragm is elevated with the up-going costal margin and the abdominal wall is sucked in. With descent of the costal margin in expiration the abdominal wall moves forwards again.
The ordinary simultaneous rib and diaphragm movements can be so balanced that the abdominal wall does not move at all. Thus respiration may function quite well in tight corsets, plaster casts, etc. In children and many women thoracic movement is greater than diaphragmatic movement. In men diaphragmatic movement is greater, especially as the years go by.
Thoracotomy
Surgical access to thoracic structures involves some kind of thoracotomy. In the anterolateral or posterolateral type, skin and underlying muscles are incised along the line of the chosen rib (often fifth or sixth) and the periosteum stripped off the rib (keeping away from the intercostal nerve and vessels which run immediately below a rib). With or without resection of the rib, the periosteal bed of the rib is then incised to enter the pleural cavity. The nerve to serratus anterior may have to be sacrificed when incising that muscle in order to obtain the necessary exposure.
In anterior thoracotomy, or median sternotomy, the whole length of the sternum is split vertically in the midline, the sternal origin of the diaphragm detached, and the tissues behind the sternum freed by blunt dissection. Damage to the pleural sacs is avoided, remembering that the right pleura may extend a little to the left of the midline (see p. 213).
In the combined thoracoabdominal incision, the line of approach is through the eighth or ninth rib bed or intercostal space, dividing the cartilage at the costal margin and incising the anterior abdominal wall. The diaphragm is incised circumferentially near its periphery or radially towards the point of entry of the phrenic nerve, thus minimizing damage to the branches of the nerve (see p. 187).
Part three. Thoracic cavity
The cavity of the thorax is completely filled laterally by the lungs, each lying in its pleural cavity. The space between the pleural cavities occupying the centre of the thoracic cavity is the mediastinum. It contains the heart and great blood vessels, oesophagus, trachea and its bifurcation, thymus, thoracic duct, lymph nodes, phrenic and vagus nerves. The loose connective tissue between these structures connects freely with that of the neck. Mediastinitis may complicate infections in the neck.
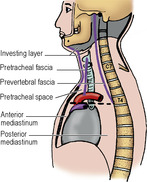
Divisions of the mediastinum
There is a plane of division to which the whole topography of the mediastinum can be related, namely a plane passing horizontally through the sternal angle (of Louis), i.e. the manubriosternal joint (Fig. 4.9). From the second costal cartilages, this plane passes backwards to the lower border of T4 vertebra. Above, between it and the thoracic inlet, lies the superior mediastinum. Below the plane, the inferior mediastinum is divided into three compartments by the fibrous pericardium: a part in front, the anterior mediastinum; a part behind, the posterior mediastinum; and the middle mediastinum in between containing the pericardium and heart together with the adjoining parts of the great vessels and the lung roots. The anterior and posterior mediastina are in direct continuity with the superior mediastinum; their separation from it is purely descriptive, not anatomical. The plane passes through the bifurcation of the trachea, the concavity of the arch of the aorta, and just above the bifurcation of the pulmonary trunk. On the plane the azygos vein enters the superior vena cava, and the thoracic duct reaches the left side of the oesophagus in its passage upwards from the abdomen. Also lying in the plane are the ligamentum arteriosum, with the left recurrent laryngeal nerve recurving below it, tracheobronchial lymph nodes, and the superficial and deep parts of the cardiac plexus.
The prevertebral and pretracheal fasciae extend from the neck into the superior mediastinum. The former fuses with the anterior longitudinal ligament over T4 vertebra; the latter blends with the pericardium over the front upper part of the heart. Thus, neck infection in front of the pretracheal fascia is directed into the anterior mediastinum, while infection behind the pre-vertebral fascia is imprisoned in the superior mediastinum in front of the vertebral bodies (Fig. 4.9). From elsewhere in the neck infection may extend through the superior into the posterior mediastinum.
Part four. Superior mediastinum
General topography
The superior mediastinum is wedge shaped (Fig. 4.9). The anterior boundary is the manubrium. The posterior boundary is much longer, due to the obliquity of the thoracic inlet. It consists of the bodies of the first four thoracic vertebrae; this wall is concave towards the mediastinum.
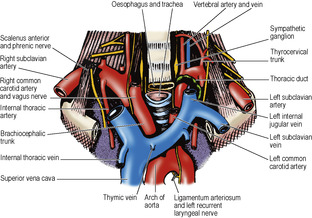
At the thoracic inlet (Fig. 4.10; and Fig. 6.9A, p. 347), often called clinically the thoracic outlet, the oesophagus lies against the body of T1 vertebra. The trachea lies on the oesophagus and may touch the jugular notch of the manubrium. The midline of the inlet is thus wholly occupied by these two tubes. At the inlet the apices of the lungs lie laterally, separated by the trachea and oesophagus and by vessels and nerves passing between the neck and the superior mediastinum. Below the inlet, the trachea slopes back and the manubrium slopes forward; the brachiocephalic trunk, the left brachiocephalic vein and the thymus occupy the space thus provided. The concavity of the arch of the aorta lies in the plane of the sternal angle, and the arch of the aorta lies wholly in the superior mediastinum, behind the manubrium. It arches over the beginning of the left bronchus and the bifurcation of the pulmonary trunk. The brachiocephalic trunk begins as a midline branch from the arch and diverges to the right as it ascends in front of the trachea (Fig. 4.10). The two other branches of the arch, the left common carotid and left subclavian arteries, pass upwards on the left side of the trachea (Fig. 4.11). These great arteries keep the left vagus nerve and apex of the left lung away from contact with the trachea (Fig. 4.13). On the right side there is no structure to separate the trachea from the right vagus (Fig. 4.12) and apex of the right lung.
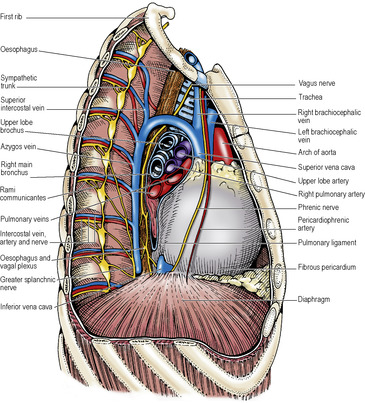 |
| Figure 4.12 |
The veins entering the superior mediastinum are the right and left brachiocephalic veins, each formed by the confluence of the internal jugular with the subclavian vein. They lie in front of the arteries and are asymmetrical. The right brachiocephalic vein passes vertically downwards; the left vein runs across the superior mediastinum, above the arch of the aorta, to join the right (Fig. 4.10). The confluence of the brachiocephalic veins produces the superior vena cava, which passes vertically downwards behind the right edge of the sternum, anterior to the right pulmonary hilum (Fig. 4.12). The right phrenic nerve descends in contact with the lateral aspect of the right brachiocephalic vein and superior vena cava.
Great vessels
Arch of the aorta
Emerging from the pericardium the ascending aorta approaches the manubrium and then at the level of the manubriosternal joint becomes the arch, which passes backwards over the left bronchus to reach the body of T4 vertebra just to the left of the midline. From its upper convexity, which reaches as high as the midpoint of the manubrium, arise the three great arteries for the head and upper limbs: the brachiocephalic trunk, and the left common carotid and left subclavian arteries (Figs 4.10 and 4.13). The arch is crossed on its left side by the phrenic and vagus nerves as they pass downwards in front of and behind the lung root respectively. Between them lie the sympathetic and vagus branches to the superficial part of the cardiac plexus. The left superior intercostal vein passes forwards across the arch superficial to the vagus, deep to the phrenic, to empty into the left brachiocephalic vein. The left recurrent laryngeal nerve hooks around the ligamentum arteriosum to pass upwards on the right side of the arch of the aorta, in the groove between the trachea and oesophagus. The pulmonary trunk bifurcates into right and left pulmonary arteries in the concavity of the arch. On the right side of the arch lie the trachea and oesophagus.
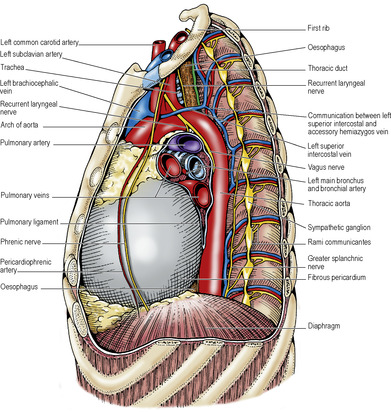 |
| Figure 4.13 |
The adventitial layer of the arch contains baroreceptors (like the carotid sinus in the wall of the internal carotid artery, see p. 343) innervated by vagal nerve fibres, which are concerned with the reflex control of the heart rate. Under the arch in the region of the ligamentum arteriosum there are some very small masses of tissue, the aortic bodies (also supplied by vagal fibres), which like the carotid bodies (see p. 343) are chemoreceptors concerned with respiratory reflexes.
The brachiocephalic trunk (innominate artery) arises in or a little to the left of the midline of the body. It slopes upwards across the trachea to the back of the right sternoclavicular joint, where it divides into the right common carotid and right subclavian arteries. It has no branches apart from the rare thyroidea ima artery, which may arise from it or directly from the arch of the aorta. The termination of the left brachiocephalic vein lies in front of the artery (Fig. 4.10).
The left common carotid artery arises just behind the brachiocephalic trunk from the upper convexity of the aortic arch. It passes straight up alongside the trachea into the neck (Fig. 4.13). It has no branches in the mediastinum.
The left subclavian artery arises just behind the left common carotid; the two run upwards together. The subclavian artery arches to the left over the pleura and the apex of the lung, which it deeply grooves. It moves away from the left common carotid at a point directly behind the left sternoclavicular joint. It has no branches in the mediastinum.
Ligamentum arteriosum
This is the fibrous remnant of the ductus arteriosus of the fetus, a channel that short-circuited the lungs. It passes from the commencement of the left pulmonary artery to the concavity of the aortic arch (Fig. 4.16), beyond the point where the left subclavian artery branches off. It lies almost horizontally. The left recurrent laryngeal nerve hooks around it. The superficial part of the cardiac plexus lies anterior to it, and the deep part is on its right, between the aortic arch and tracheal bifurcation.
Surgical approach. When the ductus persists after birth (patent ductus arteriosus) and requires surgical interruption the pleura over the aortic arch is incised behind the vagus nerve and upwards towards the origin of the left subclavian artery. The pleural flap is reflected forwards with the vagus and its left recurrent laryngeal branch to give sufficient access to the ductus. Video-assisted thoracoscopy is utilised for patent ductus arteriosus closure. The lumen of the ductus may also be obliterated by an occlusive device inserted by interventional radiology techniques.
Brachiocephalic veins
The brachiocephalic (innominate) veins are formed behind the sternoclavicular joints by confluence of the internal jugular and subclavian veins. In the neck the internal jugular vein lies lateral to the common carotid artery, in front of the upper part of scalenus anterior. The subclavian vein lies lateral to and then in front of the lower part of the muscle. Medial to scalenus anterior, these veins have joined to form the brachiocephalic vein, which lies in front of the first part of the subclavian artery. This part of each brachiocephalic vein thus receives tributaries corresponding to the branches of the first part of the subclavian artery (vertebral, inferior thyroid, internal thoracic and, on the left side only, superior intercostal).
The right brachiocephalic vein commences behind the right sternoclavicular joint and runs downwards. At its commencement it receives the right jugular, subclavian and bronchomediastinal lymph trunks separately or their confluent channel, the right lymphatic duct.
The left brachiocephalic vein passes to the right with a downward inclination, across the superior mediastinum, above the arch of the aorta, behind the thymus and the upper half of the manubrium. In the infant the left brachiocephalic vein projects slightly above the jugular notch, and may do so in the adult if the vein is distended, especially if the head and neck are thrown back. The vein is then vulnerable to suprasternal incisions (e.g. for tracheotomy). The commencement of the vein receives the thoracic duct, which often divides into two or three branches that join the vein separately. In addition to the vertebral and internal thoracic veins the left brachiocephalic vein receives most of the inferior thyroid veins, the left superior intercostal vein, and a large thymic vein (Figs 4.10 and 4.13).
The pretracheal fascia (see p. 331) passes down behind the vein and directs a retrosternal goitre into the space between the vein and the brachiocephalic trunk and trachea.
Superior vena cava
This vessel commences at the lower border of the first right costal cartilage by confluence of the two brachiocephalic veins (Figs 4.10 and 4.12). It passes vertically downwards behind the right border of the sternum and, piercing the pericardium at the level of the second costal cartilage, enters the upper border of the right atrium at the lower border of the third right costal cartilage. Behind the sternal angle it receives the azygos vein, which has arched forwards over the root of the right lung. There are no valves in the superior vena cava, the brachiocephalic veins or the azygos system of veins.