Maria Arlene Gapac Lemin
Thoracic Surgery
Thoracic surgery, like other specialties, has evolved with the increased understanding of pathophysiology, and development of improved surgical techniques and treatments. The thoracic specialty extends beyond the surgical arena into infectious disease, trauma, and oncology. Improved technology and the determination to treat diseases previously considered untreatable with operative and other invasive procedures continue to improve the recovery rate for patients experiencing thoracic diseases. As the ability to treat thoracic disease has improved, the responsibilities of the perioperative nurse have expanded, resulting in accomplishments throughout the years that have provided an extensive knowledge base and specialized perioperative practitioners.
Surgical Anatomy
The skeletal framework of the thorax is formed anteriorly by the sternum and costal cartilages, laterally by the 12 pairs of ribs, and posteriorly by the 12 thoracic vertebrae (Figure 23-1). This airtight compartment is enclosed in the root of the neck by Sibson fascia and is separated from the abdomen by the diaphragm.
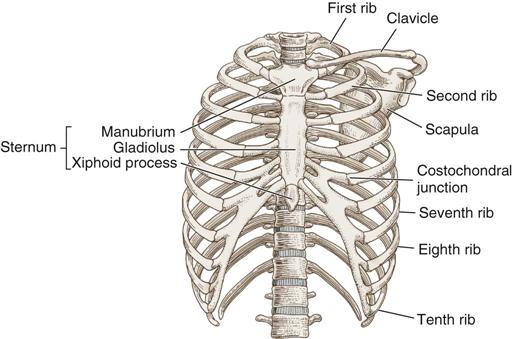
The sternum forms the anterior thoracic wall in the midline. It consists of three parts: (1) the upper part, or manubrium; (2) the body, or gladiolus; and (3) the lower cartilage, or xiphoid process. The manubrium articulates with the clavicles and the first two ribs on each side; the gladiolus articulates with the remaining true ribs by separate costal cartilages; and the xiphoid fuses with the gladiolus in early development and is attached to the diaphragm by the substernal ligament.
Normally the lateral walls of the thorax are formed by the 12 pairs of ribs. Posteriorly, each pair of ribs articulates with its corresponding thoracic vertebrae. Anteriorly, the first seven ribs articulate with the sternum. The eighth, ninth, and tenth ribs articulate with the costal cartilages of the rib above; however, the eleventh and twelfth ribs are not fixed to the costal arch (see Figure 23-1).
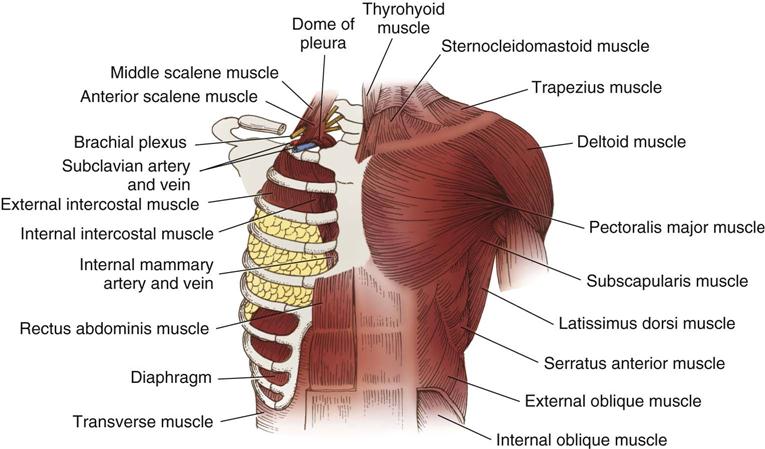
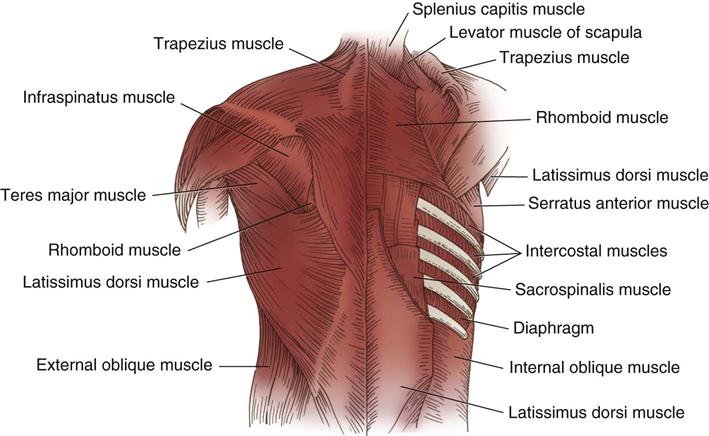
The muscles of each hemithorax (Figures 23-2 and 23-3) include the 11 external and 11 internal intercostal muscles, which fill the spaces between the ribs. An intercostal artery, vein, and nerve accompany each intercostal muscle. The arteries communicate with the internal thoracic artery anteriorly and arise from the aorta posteriorly. The intercostal veins follow the course of the arteries and communicate with the mammary veins anteriorly and with the azygos and hemiazygos veins posteriorly.
During surgery great care is taken to prevent injury to the intercostal nerve, which passes forward and alongside the posterior intercostal artery and shares the intercostal groove on the inferior edge of the corresponding rib with the superior branch of the artery. When the nerve must be disturbed, an anesthetic agent may be injected to prevent postoperative pain.
The thoracic outlet is a junction bound anteriorly by the manubrium, anterolaterally by the first ribs, and posteriorly by the first thoracic vertebrae and posterior angles of the first ribs of the space. The great vessels of the head, neck, and arm pass through this space. Compression of these structures may cause thoracic outlet syndrome.
The mediastinum is divided into anterior, middle, and posterior compartments. The anterior mediastinum is bound anteriorly by the sternum and posteriorly by the pericardium and great vessels. It contains the thymus gland, lymph nodes, and pericardial fat. The middle mediastinum is bound anteriorly by the pericardium and great vessels and posteriorly by the anterior border of the vertebral bodies. The posterior mediastinum is bound anteriorly by the vertebral bodies and extends posteriorly to the chest wall.
The chest cavity is subdivided into the right and the left pleural cavities, which contain the lungs separated by the mediastinum, which lies medially between the two pleural membranes. The parietal pleura, the membrane that lines the inner surface of each hemithorax, is adjacent to the inner surfaces of the ribs posteriorly and the mediastinum medially and covers the surface of the diaphragm except at the central portion. Part of the parietal membrane is reflected back at the root of each lung to form a sac around it. This reflection is called the visceral pleura. The pleural space normally holds about 50 mL of pleural fluid, a serous secretion that provides lubrication between these two membranes to minimize friction during inspiration and expiration (Brashers, 2012).
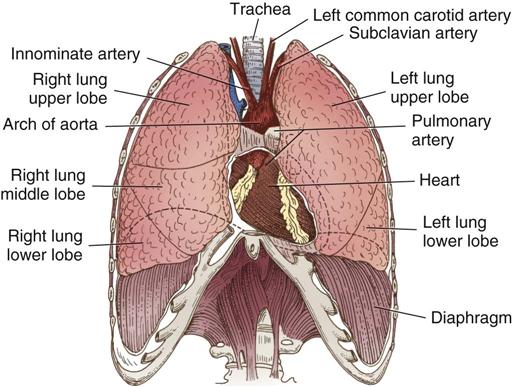
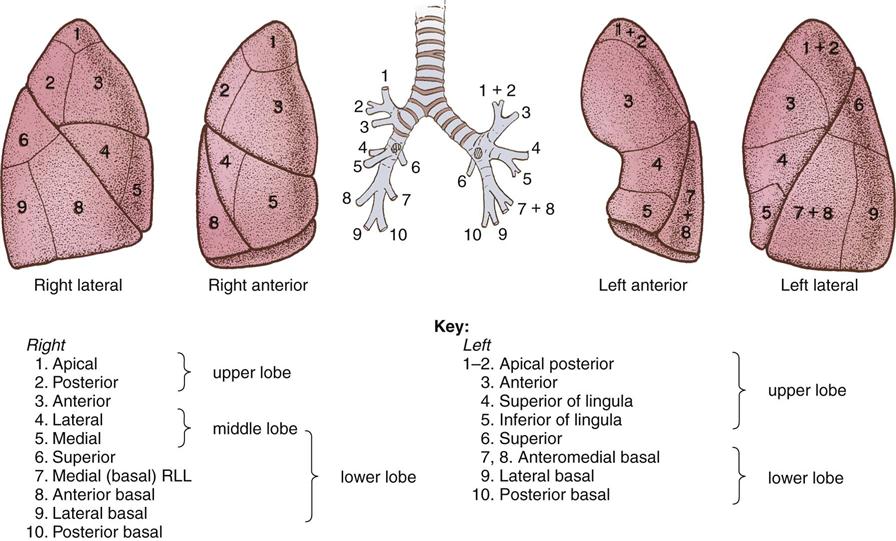
The lungs are the essential organs of respiration. The base of each lung rests on the diaphragm, whereas its apex (upper end) projects into the base of the neck at a level above the first rib. The bronchus, the nerves, the lymphatics, and the pulmonary and bronchial vessels enter and leave the lung on the mediastinal surface in a structure known as the hilum, or root, of the lung. Deep fissures divide the spongy, porous lung into lobes. The primary bronchi divide and then subdivide into each lobe and eventually become bronchioles. The right lung has an upper, a middle, and a lower lobe; the left lung has only an upper and a lower lobe (Figure 23-4). However, the lungs are similar in that each is composed of 10 major segments (Figure 23-5). Each segment extends to the pleural surface, expanding in volume from its center to its peripheral edges. Each segment also has its own bronchus and branches of the pulmonary artery and vein.
The bronchial arteries, arising from the aorta, supply nourishment to the lungs. They vary in their number and course. The arrangement may include two branches to the left lung and one branch to the right lung, which later branches into two, or there may be one or two branches for each lung. The pulmonary arteries carry the blood to the pulmonary parenchyma, and the pulmonary veins transport the oxygenated blood to the left atrium.
The nerves of the lungs are a part of the autonomic nervous system (see Chapter 21). They regulate constriction and relaxation of the bronchi and of the blood vessels within the lungs.
Although the thoracic cavity is an airtight space, the lungs receive outside air through the nasal passages, trachea, and bronchi. The main function of the lungs is to exchange carbon dioxide for oxygen. Normally, as the thorax expands, the lungs also expand as air is drawn in; during expiration, the thorax relaxes and the lungs passively contract as air is forced out. Inspiration normally takes place when the intrathoracic pressure is slightly below atmospheric pressure (76 cm Hg, or 760 mm Hg) and when a partial vacuum exists between the parietal and visceral pleural (intrathoracic) surfaces. As the muscles of inspiration contract to enlarge the chest cage, the lungs passively follow the diaphragm and chest wall because of decreased intrathoracic pressure. The acts of inspiration and expiration are the result of air moving in and out of the lung, causing pressure to equalize with that of the atmosphere at the end of expiration.
The normal intrapleural pressure varies from –9 to –12 cm H2O during inspiration and from about –3 to –6 cm H2O during expiration. The greatest amount of air that can be expired after a maximum inspiration is termed the vital capacity, and the volume of gas remaining in the lungs after maximal expiration is residual volume. Size, age, gender, and pulmonary disease of the patient influence vital capacity. Any condition that interferes with the normally negative intrapleural pressure affects respiratory function.
Perioperative Nursing Considerations
Assessment
During assessment the perioperative nurse gathers information that is important to planning patient care. Signs and symptoms demonstrated by the patient are confirmed by the perioperative nurse during the admission assessment. The nurse may begin data collection by identifying the patient and confirming the correct surgical site. A thorough review of the patient’s medical record, including results of the history, physical examination, laboratory tests, other diagnostic workups, and the nursing history and assessment, is critical for subsequent care planning. It is valuable to assess the patient’s understanding of the disease process and of the anticipated procedure. In addition to assessing the patient’s knowledge and understanding of the proposed surgical procedure and outcomes, the perioperative nurse ensures that the patient has adequate support to assist the patient through the surgical experience and recovery. The nurse should also assess emotional status because patients with a possible diagnosis of carcinoma may be very anxious. A focused assessment of the respiratory system should be included during the physical assessment. The nurse questions the patient or otherwise confirms the presence of an increased frequency of cough, increase in sputum production, recurrent hemoptysis, malaise, shortness of breath, substernal chest discomfort, weight loss, poor appetite, status of nutrition, and hypoxia. The results of the physical examination of the chest should be reviewed; the perioperative nurse may auscultate the chest and confirm the presence of crackles or wheezes on inspiration or expiration, which should be documented on the medical record.
The review of diagnostic and laboratory tests may include the chest x-ray films, sputum analysis obtained during bronchoscopy, cytology reports, arterial blood gas (ABG) results (Appendix A), and pulmonary function studies (Table 23-1). Laboratory tests including the complete blood count (CBC) should be within normal limits but may indicate anemia. The chest x-ray film remains an indispensable diagnostic tool and is needed in the operating room (OR). This film outlines the lesion, if any is present, and defines its shape and space-occupying nature (e.g., tracheal shift). The presence of air in the hilar region, pleural effusion, or atelectasis may also be confirmed by radiologic evidence. Sputum analysis for culture and sensitivity may alert the perioperative nurse to an infectious process; cytologic examination may confirm a malignancy. The patient may have already undergone diagnostic bronchoscopy or mediastinoscopy; if so, the findings for acid-fast bacillus smear, culture, bronchial washing, and biopsy should be reviewed. Pulmonary function tests with a forced expiratory volume in 1 second (FEV1) less than 1 L indicate the patient is at extremely high risk for pulmonary complications in the postoperative period. Computed tomography (CT) scans of the chest, as well as of the brain, liver, and abdomen, may reveal the presence or absence of metastasis, pleural calcification, thickening, or plaque. Radioisotope scans may have been done for similar reasons as the CT. Magnetic resonance imaging (MRI) detects vascular relationships to masses or vascular lesions. Positron emission tomography (PET) is a noninvasive study demonstrated to be highly accurate in diagnosing malignant pulmonary nodules and lymphadenopathy. MRI and PET are sometimes performed to rule out metastasis of the lesion. Transbronchial needle aspiration is useful in diagnosing mediastinal lymphadenopathy and staging lung cancer. Ventilation and perfusion studies show the distribution of each function in the lung. These results assist the perioperative nurse in collaborating with the surgical team to maintain effective gas exchange during the surgical intervention. The results are also valuable in predicting postoperative respiratory function and metabolic responses. Patients hospitalized for surgery related to carcinoma may have received chemotherapy or radiation therapy before surgery. Assessment of the skin and the patient’s general condition is important in preventing perioperative complications. The nurse should also assess the patient’s pain tolerance to determine necessary teaching or tools that will assist in achieving positive postoperative outcomes.
TABLE 23-1
| Test | Purpose |
| FVC (forced vital capacity): Records maximum amount of air that can be exhaled as quickly as possible after maximum inspiration | Provides an indication of respiratory muscle strength and ventilatory reserve. Often reduced in obstructive disease (because of air trapping) and in restrictive disease |
| FEV1 (forced expiratory volume in 1 second): Records maximum amount of air that can be exhaled in first second of respiration | Effort dependent and declines with age; reduced in certain obstructive and restrictive disorders |
| FEV1/FVC: Ratio of expiratory volume in 1 second to FVC | Provides a more sensitive indicator of obstruction to airflow. Ratio is normal or increased in restrictive disease, but decreased in obstructive disease. |
| FEF25-75%: Records forced expiratory flow over 25%-75% volume (middle half) of FVC | This measure provides a more sensitive index of obstruction in smaller airways. |
| FRC (functional residual capacity): Amount of air remaining in lungs after normal expiration | Increased FRC indicates hyperinflation or air trapping, which may result from obstructive disease. |
| TLC (total lung capacity): Amount of air remaining in lungs at end of maximum inhalation | Increased TLC indicates air trapping associated with obstructive pulmonary disease. Decreased TLC indicates restrictive disease. |
| RV (residual volume): Amount of air remaining in lungs at end of a full, forced exhalation | RV is increased in obstructive pulmonary disease, such as emphysema. |
| DLco (diffusion capacity of carbon monoxide): Reflects surface area of alveolocapillary membrane | DLco is reduced when alveolocapillary membrane is diminished, such as in emphysema, pulmonary hypertension, and pulmonary fibrosis. |
From Pagana KD, Pagana TJ: Mosby’s diagnostic and laboratory test references, ed 10, St Louis, 2012, Mosby; Rees HC: Assessment of the respiratory system. In Ignatavicius DD, Workman ML, editors: Medical-surgical nursing: patient-centered collaborative care, ed 7, St. Louis, 2013, Saunders.
The nurse should assess the patient’s smoking history (including the use of cigars, pipes, tobacco, or controlled substances) and any exposure to secondhand smoke within the home and workplace. The nurse should also reinforce the need to abstain from tobacco following surgery (Rees, 2013). Patients might be sensitive about smoking history because of the assumed relationship between smoking and lung disease. The nurse should phrase questions in a way that will not result in guilt about smoking habits or assumptions that the diagnosed condition is associated with smoking.
After a general and focused review of the patient’s medical record and patient interview, the perioperative nurse formulates nursing diagnoses. These statements reflect problems that require perioperative nursing intervention, either independently or collaboratively with other members of the surgical team. Nursing diagnoses should be individualized and prioritized for each patient.
Nursing Diagnosis
Nursing diagnoses related to the care of patients undergoing thoracic surgery might include the following:
Outcome Identification
Outcomes identified for the selected nursing diagnoses could be stated as follows:
Planning
A Sample Plan of Care for a patient undergoing thoracic surgery is shown below.
Implementation
During implementation of the plan of care the perioperative nurse is concerned with both preparatory patient considerations (e.g., procedure explanation and teaching for the patient; verification of the patient, surgical procedure, and site; positioning; presurgical diagnostic interventions; draping) and the requirements of the surgical intervention (e.g., medication delivery; instrumentation equipment, and supply availability). These patient care needs are coordinated with the other nursing interventions identified in the specific patient’s plan of care.
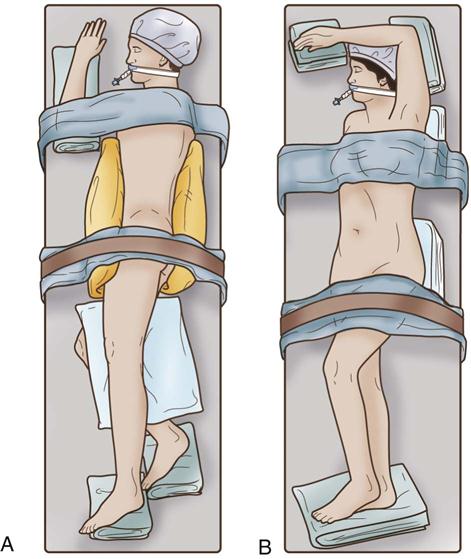
Positioning.
The type of position used in thoracic surgery is determined by the operative procedure planned. Bronchoscopy is usually performed in the supine position, commonly with a shoulder roll. Thoracotomy can be performed with the patient in one of three common positions: (1) lateral for the posterolateral approach, (2) semilateral for the anterolateral approach (Figure 23-6), and (3) supine for the median sternotomy approach. Arms are placed on padded armboards with the palms up and fingers extended. Armboards are maintained at less than a 90-degree angle to prevent brachial plexus stretch. If there are surgical reasons to tuck the arms at the side, the elbows are padded to protect the ulnar nerve, the palms face inward, and the wrist is maintained in a neutral position (Denholm, 2009). A drape secures the arms. It should be tucked snuggly under the patient, not under the mattress. This prevents the arm from shifting downward intraoperatively and resting against the OR bed rail. A beanbag can be used to support the patient in the lateral decubitus position.
The prone position also can provide access in some procedures (see Chapter 6 for safe positioning interventions). Adequate padding and safe transfer should be implemented to prevent pressure injury.
Draping.
Draping may be minimal for bronchoscopic procedures. The principles of draping for other procedures (see Chapter 4) are followed in all other thoracic procedures. Drapes may consist of a fenestrated sheet or single sheets surrounding the incision site. To prevent instruments from falling from the field, the scrub person may place a magnetic pad on the drapes below the incision site when the patient is placed in lateral position. The perioperative nurse ensures a forced-air warming blanket is placed on the patient before draping to maintain normothermia. Intermittent pneumatic compression devices are often applied also to prevent the development of deep vein thrombosis (DVT).
Instrumentation.
Bronchoscopy instruments are designed to directly inspect and observe the larynx, trachea, and bronchi; to remove secretions; to obtain washings or tissue for bacterial and cytologic studies; or to remove tissue. They are also designed to remove foreign bodies. Both rigid and flexible bronchoscopes are available, with the rigid bronchoscope being better suited for removing foreign bodies. Instrumentation for thoracic surgery includes the laparotomy instrument set (see Chapter 11) and specialty items. Instruments used for a thoracotomy or chest procedure include a combination of delicate and heavy instruments. Stapling equipment is commonly used. These devices require staplers and staple reload of appropriate sizes. The delicate instruments are used to cut tissue and vessels or to clamp tissue in an atraumatic manner. The heavier instruments are used for bone cutting, dissecting, or retracting. Instrumentation must also be available for hemostasis and suturing of all types of tissue.
The scrub person, who may be a registered nurse or surgical technologist, should determine the arrangement of items on the instrument table and Mayo stand; this arrangement should be an effective standard method that applies principles of work simplification and thorough knowledge of procedures. The possibility always exists that any incision may need to be extended to accommodate a more extensive procedure than was originally planned. Therefore, the practice of performing an initial count is recommended for all procedures, including minimally invasive procedures such as laparoscopy or thoracoscopy (Association of periOperative Registered Nurses [AORN], 2013). Lengthy incisions are often required for thoracic procedures; therefore, it is critical that an instrument count be performed before closure.
Equipment.
In thoracic surgery a variety of equipment is used, including a forced-air warming unit, fiberoptic headlights, fiberoptic light sources, video equipment, intermittent pneumatic compression devices, and anesthesia supplies. To deflate the operative lung and ventilate the nonoperative lung, double-lumen endotracheal tubes are commonly used for thoracotomies.
The neodymium:yttrium-aluminum-garnet (Nd:YAG) or CO2 laser can be used for treating tracheobronchial lesions with use of a bronchoscope. Obstruction of the mainstem bronchus and trachea caused by benign and malignant lesions can also be effectively treated with laser therapy. Use of laser equipment requires a thorough understanding of the equipment, the safety issues, the responsibilities (see Chapter 8), and the planned surgical procedure.
Monitoring.
Monitored anesthesia care, local anesthesia, or topical anesthesia may be used during some bronchoscopic procedures. General anesthesia also may be used for bronchoscopic procedures as well as other thoracic procedures. Team members work in cooperation to constantly monitor laboratory results (e.g., ABGs), oxygenation, temperature, blood loss, and urine output. Monitoring intermittent pneumatic compression device settings and patient position also is important in providing safe patient care. Results are communicated with other team members and documented for continuity of care.
Blood Replacement.
Blood replacement therapy during or after the procedure may be required because of extensive tissue dissection in a highly vascular area. The patient may have autologous blood ordered; however, the diagnosis or urgency of the procedure may prohibit patient donation of his or her own blood. The patient’s blood type and amount of blood ordered should be noted before the procedure and its availability confirmed. During the procedure every effort should be made to control and monitor bleeding. If blood collection or reinfusion systems are used, the manufacturer’s instructions and institutional protocols should be followed. Bloodless surgery programs are available at some institutions and can help minimize the need for allogeneic or autologous blood use.
Chest Drainage Systems.
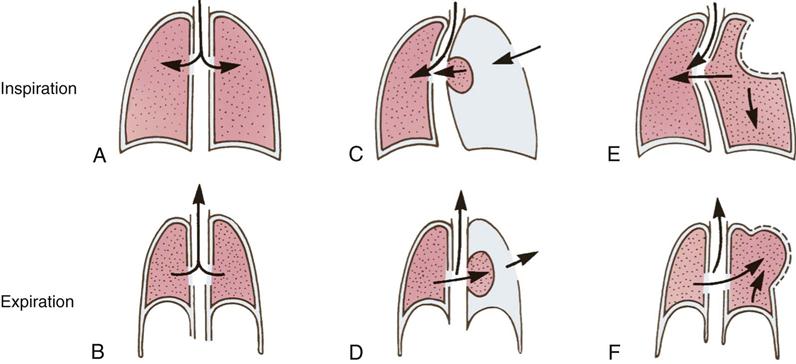
Chest tube and chest drainage system management represents an important intervention for perioperative nurses. In the presence of restrictive and obstructive pulmonary disease, the lung may not fully expand or contract, causing a reduction in alveolar ventilation with resultant hypoxia. Other conditions that interfere with respiratory function are excessive accumulation of mucus, pleural effusions, a foreign body in a bronchus, closed pneumothorax (simple and tension types), open pneumothorax, hemothorax, and multiple rib injuries that produce paradoxical motion of the thoracic cage, or flail chest (Figure 23-7).
The normal function of the lungs is supported by elasticity and negative intrapleural pressure. Collapse of the normal lung follows any condition that reduces or eliminates the negative intrapleural pressure if the lung is not adhering to the chest wall. When the pleural space is filled with air, the lung collapses due to the loss of negative pressure. This action may cause complete collapse if the pressure within the intrathoracic (pleural) space becomes positive.
A diminished negative pressure or the occurrence of actual positive pressure in one pleural space may cause the mediastinum or trachea to shift toward the opposite side. When this occurs, not only does the affected lung collapse because of a positive pressure in the pleural space, but also the function of the lung on the opposite side may be impaired as a result of compression by the mediastinal shift. Tension pneumothorax can produce serious effects as air continues to escape from the lung into the intrapleural space. The air cannot return to the bronchi to be exhaled, thereby increasing the intrapleural pressure. As the positive pressure continues to build, venous return to the heart is impaired and hemodynamic collapse may occur. When a large opening in the chest wall allows direct communication of the pleural space with atmospheric pressure, it may cause death if the mediastinum becomes mobile.
Paradoxical motion of the chest results from severe instability of the chest wall because of multiple and often bilateral rib fractures; with inspiration, partial collapse of the thoracic space occurs. The blunt injury that caused the multiple rib fractures also causes severe contusion of the lung itself. This contusion contributes to impairment of lung function by affecting gas exchange, which may result in severe, life-threatening hypoxia.
One or more chest catheters (tubes) may be inserted for postoperative closed-chest drainage. The chest tubes provide a conduit for drainage of air, blood, and other fluid from the intrapleural or mediastinal space and reestablishment of negative pressure in the intrapleural space (Patient Safety). Drainage systems use three mechanisms to drain fluid and air from the pleural cavity: positive expiratory pressure, gravity, and suction. The chest tubes are connected to a sterile water-seal or gravity drainage system. Water-seal suction may be necessary when a persistent air leak cannot be controlled by drainage alone. Several compact, disposable units are available. The disposable units have three or four compartments for drainage, water seal, and suction. The first chamber collects the drainage from the intrapleural space, the second chamber provides the water seal, and the third provides the suction control determined by the level of water (Figure 23-8). If two chest tubes are inserted, they may be attached by a Y connector to a single drainage unit or may be attached individually to two separate units. Chest tubes may be removed when the air leak has been resolved and the volume of drainage remains at an acceptable level for 24 hours (Nason et al, 2010).

Documentation.
The nurse’s documentation of perioperative care includes a summary of preoperative assessment information that supports formulated nursing diagnoses, nursing interventions, and postoperative evaluation. Documentation for a patient undergoing a thoracotomy specifically addresses patient assessment information related to position of the patient, positioning aids used, medications administered, results of laboratory tests completed, special equipment used, urine output, blood replacement, insertion of chest tubes and drainage systems, and postoperative evaluation of patient care outcomes.
Transfer Report.
The patient is transferred from the OR to the postanesthesia care unit (PACU) after thoracotomy. The report to the PACU nurse is often a collaborative effort of the nurse and anesthesia provider. The perioperative nurse reports the procedure performed, particularly if it varies from the anticipated or scheduled procedure, and describes the patient’s preoperative status, including anxiety level and understanding of the procedure, to assist the PACU nurse in meeting the emotional and educational needs of the patient. The nurse’s description of the patient’s position during the procedure provides criteria for assessment and evaluation of mobility. Results of immediate postoperative assessment, including skin integrity, location and type of dressing applied, location and type of drains, blood loss, fluid replacement, medications administered, and laboratory results obtained during the procedure, are reported by the nurse and anesthesia provider as a baseline control for assessment in the PACU. The perioperative care plan should be reviewed and patient outcomes reported.
Postprocedural Concerns.
The patient’s endotracheal tube may remain in place to maintain an adequate gas exchange. Gas exchange and effective ventilation are two immediate clinical needs after thoracotomy. Chest tubes are often connected to suction, except for post-pneumonectomy procedures. The thoracotomy is considered a painful procedure and, when coupled with muscle injury, affects functional capacity. Anesthesia providers frequently use postprocedure epidural catheters for pain management to improve the comfort level of the patient because postoperative activities are encouraged.
Fluid volume overload can lead to acute life-threatening respiratory disease syndrome that should be avoided. Monitoring urine output is important, but post-thoracotomy patients should be maintained in a state of hydration that does not require a fluid bolus for low urine output.
Patients are often anxious about their limitations, the environment, and the results of the procedure. Patients and families will benefit from preoperative teaching about pain management techniques and use of the institution’s pain assessment tool. Patients and families should also be encouraged to discuss their feelings and needs both before and after the surgical procedure. The perioperative nurse should facilitate notification of the patient’s status to the family members during and as soon as possible after the procedure.
Evaluation
At the completion of the surgical procedure, perioperative nursing goals are evaluated. They may be restated as brief outcomes. For the goals identified for the patient undergoing thoracic surgery, outcomes could be stated as follows:
Patient and Family Education and Discharge Planning
Discharge status is determined by the type of procedure being performed and the patient’s overall state of health. General patient concerns might include mobility and activity levels or restrictions, pain management, wound care, dietary recommendations, medication regimens, follow-up appointments, and any prescribed outpatient care or referrals. Both the patient and the family need specific instructions for discharge that relate to the specific procedure. Patients and their families are encouraged to partner with the healthcare team and to ask appropriate questions and establish lines of communication (Patient-Centered Care). The nurse fosters patient autonomy and reviews all information verbally and provides it in written form, with verification of understanding and time for questions and concerns.
Patients are discharged within hours of a bronchoscopy. Their main concerns might be the results of biopsy and diagnosis. The patient and family should be aware of the length of time until results will be available and the method used to obtain those results. Patients should also be reminded of the need to rest for 2 to 3 days after the procedure. Side effects might result from medications used for moderate sedation or untoward intraoperative outcomes (e.g., the patient may experience bloody sputum, difficulty breathing). In addition, patients should be reminded that their throats might feel numb 2 to 3 hours after the procedure and difficulty with swallowing will subside (Ambulatory Surgery Considerations).
After a surgical procedure such as thoracoscopy or thoracotomy, vigorous pulmonary toileting is encouraged, including use of a spirometer, deep breathing, and turning and coughing every 1 to 2 hours while awake. Patients will transfer to the chair or ambulate on the day of surgery; length of time until discharge might be a few days to 1 week or more. Patients who progress without difficulty after a thoracoscopy or thoracotomy will be monitored for drainage from the chest tubes and for pain management or complications. Postoperative air leaks or pulmonary infections will delay discharge from the healthcare setting.
In-home nursing care may be initiated to monitor oxygen levels, wound care needs, and pain management. The patient may be discharged with supplemental oxygen (Patient and Family Education). This requires that the patient be weaned and demonstrate satisfactory ambulatory SaO2 (i.e., percent saturation of arterial oxygen) rates of 88% to 90%, which will most likely be supervised by home-care nurses.