Thoracic Outlet Syndrome
Robert W. Thompson
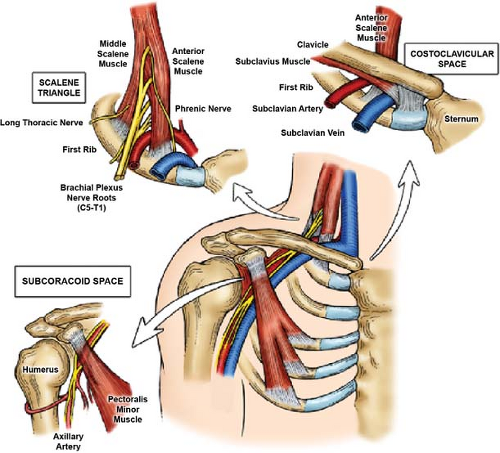
Thoracic outlet syndrome (TOS) is a group of conditions caused by compression of the neurovascular structures that serve the upper extremity. The thoracic outlet is located within the lower part of the neck, behind the clavicle and above the first rib, extending into the axilla, and it is often described by several closely related anatomic spaces, including the scalene triangle, the costoclavicular space, and the subcoracoid space (Fig. 1). Knowledge of these spaces and the structures that define them is critical toward understanding the clinical manifestations and optimal management of TOS.
Musculoskeletal Structures and Spaces of the Thoracic Outlet
The scalene fat pad lies deep to the platysma layer in the supraclavicular space of
the lower neck where it helps protect the deeper muscular and neurovascular structures of the thoracic outlet. It attaches adjacent to the internal jugular vein and the undersurface of the clavicle, and contains lymph nodes and lymphatic channels as well as small arteries and veins. The lateral part of the omohyoid muscle also passes through the scalene fat pad as it traverses the lower part of the neck. The anterior scalene muscle (ASM) lies directly behind the scalene fat pad, arising from the transverse processes of the cervical vertebrae and running vertically to attach to the top of the first rib. The middle scalene muscle (MSM) also arises from the cervical spine, runs vertically posterior to the ASM, and attaches to the top of the posterolateral first rib. The narrow vertical space formed between the ASM and MSM, with the first rib at the base, is called the scalene triangle. The major nerves and blood vessels serving the upper extremity lie within or adjacent to the scalene triangle as they pass through the upper part of the thoracic outlet. The area immediately between the first rib and the clavicle is the costoclavicular space. It is traversed by the subclavius muscle, which runs along the underside of the clavicle to attach to the first rib medial to the ASM. The subclavius muscle forms a band of dense connective tissue immediately lateral to and underneath the sternoclavicular joint, called the costoclavicular ligament. The subcoracoid space lies beyond the first rib and underneath the clavicle and is defined by the pectoralis minor muscle. This muscle lies deep to the pectoralis major muscle in the anterior upper chest, arising from the second, third, and fourth ribs. It runs upward to attach to a protrusion from the scapula known as the coracoid process, to which the long head of the biceps muscle tendon is also attached.
the lower neck where it helps protect the deeper muscular and neurovascular structures of the thoracic outlet. It attaches adjacent to the internal jugular vein and the undersurface of the clavicle, and contains lymph nodes and lymphatic channels as well as small arteries and veins. The lateral part of the omohyoid muscle also passes through the scalene fat pad as it traverses the lower part of the neck. The anterior scalene muscle (ASM) lies directly behind the scalene fat pad, arising from the transverse processes of the cervical vertebrae and running vertically to attach to the top of the first rib. The middle scalene muscle (MSM) also arises from the cervical spine, runs vertically posterior to the ASM, and attaches to the top of the posterolateral first rib. The narrow vertical space formed between the ASM and MSM, with the first rib at the base, is called the scalene triangle. The major nerves and blood vessels serving the upper extremity lie within or adjacent to the scalene triangle as they pass through the upper part of the thoracic outlet. The area immediately between the first rib and the clavicle is the costoclavicular space. It is traversed by the subclavius muscle, which runs along the underside of the clavicle to attach to the first rib medial to the ASM. The subclavius muscle forms a band of dense connective tissue immediately lateral to and underneath the sternoclavicular joint, called the costoclavicular ligament. The subcoracoid space lies beyond the first rib and underneath the clavicle and is defined by the pectoralis minor muscle. This muscle lies deep to the pectoralis major muscle in the anterior upper chest, arising from the second, third, and fourth ribs. It runs upward to attach to a protrusion from the scapula known as the coracoid process, to which the long head of the biceps muscle tendon is also attached.
Nerves of the Thoracic Outlet
The motor and sensory nerves serving the upper extremity arise from cervical nerve roots C5 through T1. After leaving the spine and passing into the scalene triangle, these nerve roots bundle together and interconnect to form the initial trunks of the brachial plexus. The three trunks of the brachial plexus include the upper trunk (formed by fusion of the C5 and C6 nerve roots), the middle trunk (composed of the C7 nerve root), and the lower trunk (formed by fusion of the C8 and T1 nerve roots). The brachial plexus nerves pass through the scalene triangle and over the lateral first rib, before passing underneath the clavicle and pectoralis minor muscle to the axilla. Further merging and branching results in formation of the divisions, cords, and terminal nerves of the brachial plexus, as well as the peripheral nerves of the upper extremity.
The phrenic nerve forms from C3, C4, and C5 at the lateral border of the ASM, then descends on the muscle surface in a lateral to medial direction. It passes behind the subclavian vein into the superior mediastinum, then on to innervate the ipsilateral hemidiaphragm. The long thoracic nerve arises from C5, C6, and C7 within the body of the MSM where its three components merge to form a single nerve. It passes through the MSM and over the posterolateral first rib, then descends to supply the serratus anterior muscle underneath the scapula. The cervical sympathetic chain passes vertically between the neck and the upper chest, lying along the posterior inner curve of the ribs. The sympathetic supply to the upper extremity arises from ganglia at T1 to T3, with several ganglia fused at the level of the first rib to form the large stellate ganglion that also supplies part of the face and eye.
Blood Vessels of the Thoracic Outlet
The subclavian artery arises from the innominate artery on the right and from the aorta on the left, in the upper chest and base of the neck. It passes up and over the first rib behind the ASM and immediately in front of the brachial plexus nerve roots, and is therefore within the scalene triangle. The vertebral artery and the internal thoracic artery arise from the subclavian artery proximal to the scalene triangle, and several smaller branches arise behind the ASM, including the transverse cervical and inferior thyroid arteries (often from a common origin). Beyond the first rib and clavicle, the subclavian artery becomes the axillary artery where it passes underneath the pectoralis minor muscle. The distal axillary artery has a number of branches that serve the shoulder girdle, including the subscapular artery and the (anterior and posterior) circumflex humeral arteries. After passing in front of the shoulder, the axillary artery becomes the brachial artery.
Blood returning from the arm passes through a number of superficial and deep veins, which combine underneath the pectoralis minor muscle to form the axillary vein. The axillary vein passes underneath the clavicle and is joined by the cephalic vein to become the subclavian vein. The subclavian vein crosses over the first rib in front of the ASM (and is therefore not within the scalene triangle). It then passes through the space between the anterior first rib, clavicle, subclavius muscle, and costoclavicular ligament. After passing over the first rib, the subclavian vein joins the internal jugular vein as it descends from the neck, forming the innominate (or brachiocephalic) vein behind the sternoclavicular joint. The innominate vein passes further underneath the sternum to join with its counterpart from the other side, forming the superior vena cava.
Anatomic Variations and Acquired Changes in the Thoracic Outlet
Many natural variations in anatomy are found in the thoracic outlet. The most obvious is a congenital cervical rib, which occurs in ∼0.5 percent of the population. Cervical ribs arise from the C7 transverse process and lie within the plane of the MSM. Osseous cervical ribs are readily detected by plain radiographs, but those composed of cartilage may not be easily identified. Complete cervical ribs attach directly to the first rib and act to displace the structures of the scalene triangle anteriorly. Partial cervical ribs can also occur, with a short segment of bony cervical rib and a ligamentous extension that attaches to the first rib; a wide C7 transverse process can also be associated with a ligamentous band in the same manner. Other rare bony anomalies include a partial first rib, an unusually high-lying first rib, or a fusion between the first and second ribs. Any of these anomalies may predispose to the development of neurovascular compression.
Soft tissues variations in the thoracic outlet are often too small to be detected by standard imaging (plain X-rays, CT, or MRI scanning), but are frequently seen at the time of surgery. For example, a scalene minimus muscle is a frequent variant in which muscle arising from the plane of the MSM passes between the nerve roots of the brachial plexus, and then joins with the ASM to attach to the first rib. A number of different ligamentous or fibrofascial bands may also be present in the thoracic outlet, which frequently pass in front of or between the brachial plexus nerve roots. One of the best described is a fibrous band that runs from the back of the first rib to the front, crossing over (and compressing) the lower nerve roots. Langer’s axillary arch is another anomalous fibrous band which extends from the latissimus dorsi muscle to the coracoid process. When present, any of these soft tissue structural variations can contribute to nerve or blood vessel compression.
Acquired changes in the anatomy of the thoracic outlet often contribute, either
directly or indirectly, to compression of the neurovascular structures. The most obvious examples are fractures of the first rib or clavicle. Fractures of the first rib are usually the result of considerable trauma associated with other severe injuries, but evidence of previous first rib fracture is occasionally observed during surgery for TOS where callous at the fracture site may act to compress the adjacent neurovascular structures. In contrast, fractures of the clavicle are relatively common and occur with lesser trauma. Most clavicular fractures heal without consequence, but a large callous from a healed (or unhealed) fracture can protrude posteriorly to compress the underlying neurovascular structures. Anatomic changes can also occur within the soft tissues of the thoracic outlet, particularly when the scalene muscles are subjected to previous stretch injury, chronic strain, and repetitive overuse. In these situations the scalene muscles undergo an inflammatory healing response that leads to fibrosis and other microscopic changes, making the muscles firm, prone to persistent spasm, and less resilient to positional changes. Localized healing responses can also lead to scarring and fibrosis directly around the brachial plexus nerve roots, which can subsequently contribute to nerve compression, irritation, and production of symptoms.
directly or indirectly, to compression of the neurovascular structures. The most obvious examples are fractures of the first rib or clavicle. Fractures of the first rib are usually the result of considerable trauma associated with other severe injuries, but evidence of previous first rib fracture is occasionally observed during surgery for TOS where callous at the fracture site may act to compress the adjacent neurovascular structures. In contrast, fractures of the clavicle are relatively common and occur with lesser trauma. Most clavicular fractures heal without consequence, but a large callous from a healed (or unhealed) fracture can protrude posteriorly to compress the underlying neurovascular structures. Anatomic changes can also occur within the soft tissues of the thoracic outlet, particularly when the scalene muscles are subjected to previous stretch injury, chronic strain, and repetitive overuse. In these situations the scalene muscles undergo an inflammatory healing response that leads to fibrosis and other microscopic changes, making the muscles firm, prone to persistent spasm, and less resilient to positional changes. Localized healing responses can also lead to scarring and fibrosis directly around the brachial plexus nerve roots, which can subsequently contribute to nerve compression, irritation, and production of symptoms.
The clinical presentation of patients with TOS depends on the specific structures compressed, giving rise to three distinct conditions: (a) Neurogenic TOS caused by compression of the brachial plexus nerves; (b) Venous TOS caused by compression of the axillary and/or subclavian veins; and (c) Arterial TOS caused by compression of the axillary and/or subclavian arteries. All three types of TOS are considered rare conditions, but clinical recognition and differentiation of these conditions is crucial in planning further steps in diagnosis and treatment.
Neurogenic Tos
Neurogenic TOS (85% to 95% of all patients with TOS) is characterized by compression of the brachial plexus nerve roots within the scalene triangle and/or subpectoralis space. This may be due to two factors: (a) variations in anatomy such as anomalous scalene musculature, aberrant fibrofascial bands, or cervical ribs and (b) neck or upper extremity injury that has resulted in scalene or pectoralis minor muscle spasm, fibrosis, and other pathological changes. The symptoms of brachial plexus nerve root compression consist of pain, numbness, and tingling (paresthesias) in the neck, shoulder, arm, and hand. These symptoms can be somewhat variable throughout the day and they may differ day-to-day, depending on levels of activity. The symptoms are also typically dynamic, with marked positional exacerbation during arm abduction, elevation, and other maneuvers. There is usually localizing tenderness and reproduction of symptoms on palpation over the scalene triangle and/or subpectoralis space. Patients with neurogenic TOS often have gradual development of symptoms, but can have acute exacerbations or a steady progression with increasing disability. The diagnosis of neurogenic TOS is difficult and often elusive, and may involve extensive testing, multiple specialist evaluations, and prolonged attempts at various forms of management.
Venous Tos
Venous TOS (10% to 15% of all patients with TOS) is characterized by subclavian vein compression between the clavicle, subclavius muscle, and first rib. Most patients present with abrupt spontaneous swelling of the entire arm, often with cyanotic (bluish) discoloration, heaviness, and pain, which form the characteristic features of axillary-subclavian vein “effort thrombosis.” Effort thrombosis (also known as the “Paget–Schroetter” syndrome) is distinct from more common forms of deep venous thrombosis (DVT) in that it occurs in young, active, and otherwise healthy individuals, with no underlying blood clotting disorder. The pathogenesis of effort thrombosis involves repetitive extrinsic compression of the subclavian vein during activities involving arm elevation or exertion, leading in time to chronic venous injury and progressive fibrous stenosis of the vein. This involves scar tissue formation and contraction around the outside of the vein, as well as fibrosis and wall thickening within the wall of the vein itself. The initial phase of venous TOS is usually asymptomatic due to simultaneous expansion of collateral veins passing around the narrowed subclavian vein, but stagnant blood within the subclavian vein eventually leads to thrombotic occlusion. Growth and extension of this clot into the axillary vein can then result in further obstruction of critical collateral veins, resulting in the acute clinical presentation. Pulmonary embolism from clot within the proximal subclavian vein may also occur, particularly with motion of the arm, but this is infrequent compared to DVT in the lower extremities.
Arterial Tos
Arterial TOS (2% to 5% of all patients with TOS) is caused by subclavian artery compression within the scalene triangle, leading to the development of subclavian artery occlusions or post-stenotic subclavian artery aneurysms. These lesions almost always occur in association with a congenital cervical rib or other bony anomaly. Ulcerative subclavian artery lesions and aneurysms are often accompanied by mural thrombus formation, and frequently complicated by distal thromboembolism with hand and/or digital ischemia. Patients with acute thromboembolism present with a sudden onset of hand pain and weakness, numbness and tingling, and cold and pale fingers. Those with more longstanding ischemia may present with chronic arm fatigue or claudication, non-healing wounds, or ulcerations in the fingers. Subclavian artery occlusions or aneurysms may also be asymptomatic. Occlusions may be identified by a significant blood pressure differential between arms, and aneurysms occasionally present as a nontender pulsatile mass in the lateral neck. A second form of arterial TOS is observed almost solely in overhead throwing athletes, associated with occlusive or aneurysmal lesions of the distal axillary artery. These lesions are caused by repetitive trauma from hyperextension during the throwing motion, in which the axillary artery can be compressed by forward motion of the head of the humerus. The complications of these lesions are similar to those of arterial TOS caused by subclavian artery lesions at the level of the first rib.
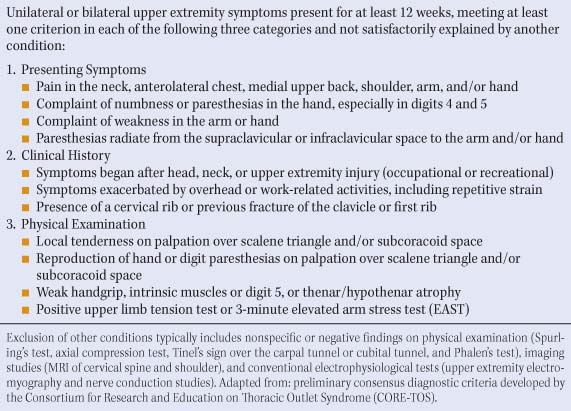
The diagnosis of neurogenic TOS is based on clinical evaluation according to the criteria listed in Table 1, supplemented by relevant testing procedures to exclude alternative conditions. The extent of brachial plexus compression attributable to either the scalene triangle or the subcoracoid space is characterized by physical examination. A chest X-ray can help determine the presence or absence of a cervical rib, but other imaging studies of the brachial plexus are usually not helpful. Although conventional electromyography and nerve conduction studies (EMG/NCS) are often performed to exclude peripheral nerve compression disorders or cervical radiculopathy, these tests are usually negative or non-specific in neurogenic TOS. Almost all patients with a suspected diagnosis of neurogenic TOS undergo an anterior scalene and/or pectoralis minor muscle block with
a short-acting local anesthetic, both to support the clinical diagnosis and to help predict the reversibility of symptoms with treatment.
a short-acting local anesthetic, both to support the clinical diagnosis and to help predict the reversibility of symptoms with treatment.
Table 1 Diagnostic Features of Neurogenic TOS | |
|---|---|
|
The diagnosis of venous TOS is based on the stereotypical clinical presentation of axillary-subclavian vein effort thrombosis. Upper extremity venous Duplex studies may confirm the presence of upper extremity DVT, but Duplex imaging of the subclavian vein is inaccurate and therefore cannot be used to exclude the diagnosis. More definitive information on the location and the extent of axillary-subclavian vein thrombosis is obtained by contrast-enhanced imaging studies, such as magnetic resonance angiography or catheter-based venography. When there is incomplete subclavian vein obstruction, these studies can also be performed with the arms at rest and in elevation. The advantage of using catheter-based upper extremity venography as the initial diagnostic step is that this can be followed immediately by thrombolytic therapy, with completion venograms typically revealing a focal area of residual subclavian vein stenosis or occlusion at the level of the first rib. Although blood coagulation testing is often performed in patients with upper extremity DVT, these tests are usually negative and add little to the initial diagnosis or management.
The diagnosis of arterial TOS is suspected by clinical findings and potentially confirmed by non-invasive vascular laboratory studies such as Duplex imaging and segmental arterial waveform analysis. Plain radiographs are also used to determine if a cervical rib or first rib anomaly is present. Positional angiography (with contrast-enhanced magnetic resonance imaging, computed tomography, or catheter-based arteriography) is often performed to determine the presence or absence of a subclavian artery aneurysm. Similar imaging studies are performed in the patients who have presented with upper extremity arterial thromboembolism to detect a proximal source of embolism in the subclavian or axillary artery.
Neurogenic TOS is initially treated with physical therapy to relieve scalene/pectoralis muscle spasm, improve postural disturbances, enhance functional limb mobility, strengthen associated shoulder girdle musculature, and diminish repetitive strain exposure in the workplace. It is important that the patient be referred to a therapist with experience, expertise, and interest in TOS since the management of this condition is different than that of other disorders affecting the neck, shoulder, spine, and upper extremity. Incorrect approaches to physical therapy can result in worsening of symptoms and premature failure of conservative management. After an initial 4- to 6-week course of physical therapy, significant improvement is observed in most patients with mild symptoms of neurogenic TOS or those in whom therapy has been started early after the onset of symptoms. Therapy is then continued with the expectation that continued benefits will preclude the need to consider surgical treatment. Because neurogenic TOS is considered a chronic condition subject to occasional “flare-ups” of more acute symptoms (often related to overuse activities or new injury), it remains important for the patient to continue regular physical therapy exercises and occasional therapist visits as needed during long-term follow-up.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree