I. INORMAL MICROSCOPIC ANATOMY. The wall of the urinary bladder is formed by four layers (e-Fig. 22.1).* The thickness of the innermost layer, the urothelium, depends on the degree of bladder distension, and the shape of its constituent urothelial cells ranges from smaller cuboidal cells at the base to larger polyhedral cells toward the surface. Umbrella cells, the most superficial cells, have abundant eosinophilic cytoplasm and are often binucleated. The underlying lamina propria is separated from the urothelium by a thin basement membrane and is composed of loose connective tissue with blood vessels, nerves, adipose tissue, and a variable number of smooth muscle fibers forming a discontinuous muscularis mucosae. Aggregates of urothelium termed von Brunn nests (e-Fig. 22.2) are often seen as invaginations or separate clusters in the lamina propria. The term cystitis cystica is used when these nests become prominent and undergo cystic change (e-Fig. 22.3). Cystitis glandularis is similar to cystitis cystica except that the cells lining the cysts are mucin-secreting cuboidal or columnar cells, or true goblet cells, in which case the term cystitis glandularis with intestinal metaplasia is used (e-Fig. 22.4). These proliferative lesions, although sometimes seen associated with local inflammation, represent variants of normal histology. Their main importance lies in the fact that they can occasionally cause visible lesions simulating a bladder neoplasm. The third layer, the muscularis propria or detrusor muscle, is composed of large bundles of muscle fibers and is covered by the outermost adventitial layer, including perivesical adipose tissue. It is important to note that adipose tissue can also be found in the lamina propria and wall (e-Fig. 22.5), so identification of fat does not equate to a specific layer of the bladder wall.
II. GROSS EXAMINATION AND TISSUE SAMPLING OF THE BLADDER. The most common samples submitted for surgical pathology examination include small biopsies, larger transurethral resection specimens, and partial and radical (complete) cystectomies.
A. Biopsy specimens. These are usually obtained without cautery (“cold-cup”) and should be immediately immersed in formalin. If multiple biopsies are submitted separately, as in mapping procedures, they should be processed separately. After gross examination, bladder biopsies should be marked with ink or hematoxylin, then placed in a cassette after being put in a fine mesh envelope, wrapped in lens paper, or sandwiched between sponge pads. After processing, three hematoxylin and eosin (H&E)-stained slides should be prepared, each with a strip of three to four levels.
B. Transurethral resection of bladder specimens. These specimens are usually obtained with the aid of thermal cautery, often for the transurethral resection of bladder tumors (TURBT). Because of the significant prognostic and therapeutic implications for the presence of muscularis propria invasion by the bladder neoplasms, it is often necessary to process all of the submitted tissue to ensure that such foci of invasion are not overlooked.
C. Partial cystectomy specimens. Partial or segmental cystectomy is indicated in only a minority of bladder cancer patients, typically those who suffer a first time tumor recurrence with a solitary tumor, and tumor location that allows for a 1- to 2-cm margin of resection, such as at the dome. Urachal carcinomas at the
dome and above, with extension toward the umbilicus, may also be treated by partial cystectomy, as can carcinoma in a bladder diverticulum. Carcinoma in situ elsewhere in the bladder (or multifocal tumors) is an absolute contraindication. The specimens usually consist of a sheet-like portion of tissue that should be pinned down and fixed overnight. In addition to describing and sampling any gross tumor(s) as described for cystectomy specimens, the status of the margins is very important; these can be shaved off or sampled by perpendicular sections, depending on their relationship and proximity to the tumor(s). Frozen section of the mucosal margin may be requested.
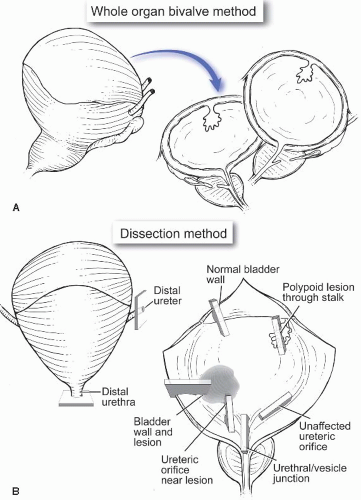
D. Total cystectomy and cystoprostatectomy specimens. Radical cystoprostatectomy in men and anterior exenteration in women, along with pelvic lymphadenectomy, are standard surgical approaches for muscle wall-invasive bladder carcinoma in the absence of metastatic disease. Cystectomy may be performed in some cases for nonmuscle wall-invasive bladder carcinoma, if the bladder is nonfunctional, or for high-grade pT1 carcinoma that is not responsive to intravesical therapy. If not sampled separately, a request to perform frozen sections on the ureteric and urethral margins may be received (Arch Pathol Lab Med. 2005;129: 1585-1601). After orientation and inking, one of two methods can be used to fix the specimen. The first entails filling the bladder with formalin (through the urethra, or by using a large bore needle through the dome) and fixing overnight; the second entails opening the bladder (usually through the urethra extending upward on the anterior surface) and pinning it flat, then fixing overnight. After opening the bladder (in the fresh or fixed state), the mucosa is examined for tumors(s) and, if present, the size, location, pattern of growth (exophytic, endophytic, and/or ulcerated), and depth of invasion are recorded. The mucosa of the adjacent bladder should also be examined for areas of hemorrhage and discoloration that may represent areas of carcinoma in situ. In addition to sampling of any tumor(s) (three to four sections of each), representative sections need to be submitted from the different areas of the bladder including the trigone; posterior, lateral, and anterior walls; and the dome (Fig. 22.1). If ureteric and urethral shave margins were not submitted for frozen section examination, they should be sampled for permanent sections, as should any possible lymph nodes identified in the perivesical fat. In cystoprostatectomy specimens, additional blocks from the prostate and seminal vesicles should be submitted, the extent of which depends on whether a preoperative diagnosis or suspicion of prostatic carcinoma exists (see Chap. 29). When the bladder (with or without the prostate) is removed as part of larger pelvic exenteration specimens (that may include portions of the rectum and/or the gynecological tract in females), it then becomes imperative to document the presence or absence of involvement of these additional organs by preferentially sampling suspicious areas, as well as by sampling the resection margins of these organs.
III. DIAGNOSTIC FEATURES OF COMMON DISEASES OF THE BLADDER
A. Congenital malformations
1. Urachal abnormalities. The urachus is a vestigial structure that connects the dome of the bladder to the umbilicus; it normally closes by the fourth month of fetal life. Persistence or malformations of the urachus can present in childhood and occasionally in adulthood; they include urachal remnants (e-Fig. 22.6), patent urachus, urachal cysts, and urachal sinuses, all of which can result in secondary infection or development of secondary tumors, most frequently adenocarcinoma (e-Fig. 22.7).
2. Exstrophy. This is a rare congenital anomaly characterized by failure of development of the anterior wall of the bladder and abdominal wall, usually resulting in severe secondary infection if left untreated.
B. Inflammatory conditions. Cystitis most frequently has an infectious etiology. There are, however, specific variants of cystitis that produce somewhat
characteristic cystoscopic and/or microscopic appearances. The latter include hemorrhagic, granulomatous, eosinophilic, and interstitial variants, as well as malakoplakia.
1. Infectious cystitis. Acute and chronic cystitis is most frequently secondary to bacterial infection (usually by enteric organisms). The incidence is higher in females, and when intermittent urinary obstruction or stasis is present. Biopsy
during active infection is contraindicated, but biopsy may be performed in cases of chronic cystitis to rule out neoplasia, especially carcinoma in situ. The histopathologic features include a nonspecific acute and/or chronic inflammatory infiltrate occasionally with lymphoid aggregates/follicles (follicular cystitis) (e-Fig. 22.8), and a variable degree of lamina propria edema. Of note, similar findings may be seen in the absence of infection such as following radiation or cytotoxic chemotherapy. Other infections can produce specific histologic findings such as viral inclusions (polyoma and herpesviruses) or granulomas (tuberculosis, fungal infections, and schistosomiasis).
2. Granulomatous cystitis. As noted above, bacterial, fungal, or parasitic infections can lead to granuloma formation. The most frequent cause, however, is iatrogenic, either secondary to intravesical Bacille Calmette-Guerin (BCG) immunotherapy for urothelial CIS and superficially invasive carcinoma (e-Fig. 22.9), or following TURBT (e-Fig. 22.10).
3. Hemorrhagic cystitis. This is an uncommon side effect of cyclophosphamide therapy that results in extensive ulceration and hemorrhage that, if severe, may require cystectomy. Adenovirus infection (in immunocompromised individuals) may also produce the same pattern.
4. Papillary and polypoid (bullous) cystitis. These related forms of cystitis are characterized by finger-like (papillary) or broad (polypoid) projections of edematous, variably inflamed lamina propria covered by reactive nonneoplastic urothelium (e-Fig. 22.11). These forms of cystitis are most frequently seen with prolonged indwelling catheter use. The presence of such an inflammatory component in papillary cystitis can help in making the occasionally difficult distinction from a low-grade papillary urothelial neoplasm.
5. Eosinophilic cystitis. This is characterized by dense infiltration of eosinophils in the bladder lamina propria (e-Fig. 22.12) and/or wall. Such infiltrates are most frequently seen adjacent to invasive urothelial carcinoma, but they also occur in patients with allergic conditions and in patients with parasitic infections, both often in association with peripheral eosinophilia.
6. Interstitial cystitis. This is an uncommon inflammatory disorder that predominantly affects middle-aged and elderly women and results in severe intractable symptoms of culture-negative cystitis. Petechial submucosal hemorrhages or ulcers (termed Hunner ulcers) are usually evident cystoscopically. The microscopic features are nonspecific and include a mixed inflammatory infiltrate in the lamina propria, often with an increased number of mast cells that can also involve the muscularis propria (e-Fig. 22.13) and nerves. Clinical correlation is required in these cases because the histological findings are, at most, consistent with the clinical impression of interstitial cystitis.
7. Malakoplakia. This is an uncommon form of cystitis characterized by the presence of soft yellowish mucosal plaques composed of inflammatory cells including abundant epithelioid histiocytes (known as von Hansemann histiocytes) (e-Fig. 22.14) that have granular eosinophilic cytoplasm, and characteristic 3- to 10-micron rounded basophilic intracytoplasmic inclusions (Michaelis-Gutmann bodies) that contain iron and calcium, best demonstrated by Prussian blue and von Kossa special stains, respectively. The condition is thought to result from a defect in the ability of histiocytes to degrade phagocytosized bacteria. Control of urinary tract infection can help control the disease.
C. Reactive and metaplastic urothelial lesions
1. Squamous metaplasia. This can be of two types, nonkeratinizing and keratinizing. The former is considered a normal finding in the trigone and bladder neck of females but can rarely be seen in males receiving estrogen treatment for prostate cancer. In contrast, keratinizing squamous metaplasia is more common in males in association with chronic irritation and is considered
a significant risk factor for the subsequent development of carcinoma (Eur Urol. 2002;42:469 and Am J Surg Pathol. 2006;20:883).
2. Intestinal metaplasia. In addition to the intestinal metaplasia occasionally seen in cystitis glandularis, intestinal metaplasia in the presence of a chronically irritated bladder can involve the bladder mucosa and lamina propria in a focal or diffuse manner, resulting in an appearance almost indistinguishable from colonic mucosa.
3. Nephrogenic metaplasia (adenoma). This is a benign epithelial proliferation composed of cells resembling renal tubular epithelium (hence the name), which usually arises in the setting of chronic irritation or injury such as infection or calculi (Adv Anat Pathol. 2006;13:247). The lesion was believed to be metaplastic, but more recent evidence has demonstrated that, at least in renal transplant recipients, nephrogenic metaplasia is derived from shed renal tubular epithelial cells that may attach to areas of prior injury. Although most frequently seen in the bladder, it is also quite common in the urethra, and less so in the ureters and renal pelvis. Nephrogenic metaplasia is usually an incidental finding, but it may also present as a mass lesion simulating cancer. Histologically, papillae (e-Fig. 22.15), small tubules (e-Fig. 22.16), or cystically dilated tubules (e-Fig. 22.17) lined by cuboidal, low-columnar, or flattened hobnail cells are seen. The importance of nephrogenic metaplasia lies in the fact that in the bladder it can be confused with adenocarcinoma (especially clear-cell adenocarcinoma) and glandular variants of urothelial carcinoma (Mod Pathol. 2009;22:S37-S52); in the urethra it can be confused with prostatic adenocarcinoma. The immunohistochemical reactivity of nephrogenic metaplasia with cytokeratin 7, α-methylacyl coenzyme A racemase (AMACR), PAX2, and PAX8 antibodies and the lack of reactivity with high-molecular-weight cytokeratin (e.g., 34βE12) and prostate-specific antigen (PSA) antibodies help in distinguishing it from its mimics.
4. Urothelial hyperplasia. An increase in the thickness of the urothelium (>7 layers) is usually reactive and most frequently seen secondary to chronic inflammatory conditions. Flat urothelial hyperplasia (e-Fig. 22.18) is more common than papillary urothelial hyperplasia, which some authors have also found to be associated with papillary urothelial neoplasms.
5. Pseudocarcinomatous epithelial hyperplasia. This change may be seen after radiation therapy, chemotherapy, or unassociated with either therapy (Arch Pathol Lab Med. 2010;134:427). The light microscopic appearance is of pseudoinfiltrative nests of urothelium in the lamina propria (e-Fig. 22.19), sometimes with squamous metaplasia. Nuclear atypia may be detected, secondary to therapy or irritation/ischemia. The irregular nests and aggregates may appear to wrap around ecstatic vessels with fibrin thrombi, which is a useful diagnostic finding.
6. Reactive urothelial atypia. Usually seen in a setting of acute and/or chronic inflammation, reactive atypia may be associated with hyperplastic or thin urothelium. Nuclear enlargement, often with vesicular chromatin and a single prominent nucleolus, is the most prominent finding (e-Fig. 22.20). Mitotic figures may be increased and cell crowding may be observed; however, polarity, cell uniformity, and maturation are usually well preserved. Acute or chronic inflammation is often identified.
D. Miscellaneous nonneoplastic conditions
1. Endometriosis. Most frequently seen on the serosal aspect of the bladder in women with a previous history of pelvic surgery, foci of endometriosis can also involve the lamina propria or muscularis propria and may be visible cystoscopically. As elsewhere, at least two of the three histologic features of endometriosis—endometrial glands, endometrial stroma, and hemosiderinladen macrophages—are required for the diagnosis (e-Fig. 22.21).
2. Endocervicosis and endosalpingiosis. These are characterized by the presence of glands within the bladder wall lined by columnar endocervical-type mucinous cells or ciliated tubal epithelial cells, respectively. When both are present with endometriosis, the term “Müllerianosis” has been used. Lack of significant nuclear atypia, mitoses, and a stromal tissue reaction help distinguish these benign lesions from invasive adenocarcinoma.
3. Diverticula. These outpouchings of mucosa through the muscularis propria are mostly due to increased pressure. Diverticula are frequently complicated by secondary inflammation, squamous metaplasia, and lithiasis, and in <10% of cases by secondary neoplastic development.
4. Amyloidosis. The bladder may rarely be involved by systemic amyloidosis, or by a primary localized form of amyloidosis limited to the bladder.
5. Ectopic prostatic tissue. These are usually small polypoid projections most frequently seen in the trigone area. They are composed of benign prostatic
epithelium (very similar to so-called “prostatic urethral polyps” of the urethra).
TABLE 22.1 WHO Histologic Classification of Tumors of the Urinary Tract (Including Bladder)
Urothelial tumors
Infiltrating urothelial carcinoma
With squamous differentiation
With glandular differentiation
With trophoblastic differentiation
Nested
Microcystic
Micropapillary
Lymphoepithelioma-like
Lymphoma-like
Plasmacytoid
Sarcomatoid
Giant cell
Undifferentiated
Noninvasive urothelial neoplasias
Urothelial carcinoma in situ
Noninvasive papillary urothelial carcinoma, high grade
Noninvasive papillary urothelial carcinoma, low grade
Noninvasive papillary urothelial neoplasm of low malignant potential
Urothelial papilloma
Inverted urothelial papilloma
Squamous neoplasms
Squamous cell carcinoma
Verrucous carcinoma
Squamous cell papilloma
Glandular neoplasms
Adenocarcinoma
Enteric
Mucinous
Signet-ring cell
Clear cell
Villous adenoma
Neuroendocrine tumors
Small cell carcinoma
Paraganglioma
Carcinoid
Melanocytic tumors
Malignant melanoma
Nevus
Mesenchymal tumors
Rhabdomyosarcoma
Leiomyosarcoma
Angiosarcoma
Osteosarcoma
Malignant fibrous histiocytoma
Leiomyoma
Hemangioma
Other
Hematopoietic and lymphoid tumors
Lymphoma
Plasmacytoma
Miscellaneous tumors
Carcinoma of Skene, Cowper, and Littre glands
Metastatic tumors and tumors extending from other organs
From: Eble JN, Sauter G, Epstein JL, et al., eds. World Health Organization Classification of Tumors. Pathology and Genetics. Tumours of the Urinary System and Male Genital Organs. Lyon: IARC Press; 2004. Used with permission.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Urinary Bladder
The Urinary Bladder
Omar Hameed
Peter A. Humphrey