15 The pancreas and spleen
The pancreas
Surgical anatomy
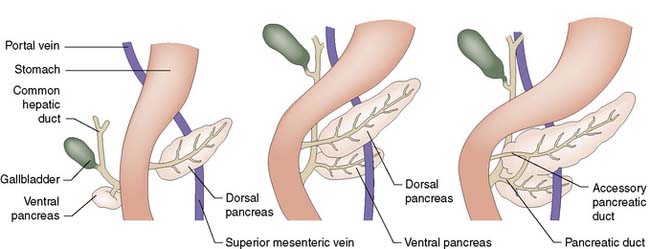
The pancreas develops from separate ventral and dorsal buds of endoderm that appear during the fourth week of fetal life. The ventral pancreas develops in association with the biliary tree, and its duct joins the common bile duct before emptying into the duodenum through the papilla of Vater (Fig. 15.1). During gestation, the duodenum rotates clockwise on its long axis, and the bile duct and ventral pancreas pass round behind it to fuse with the dorsal pancreas. Most of the duct that drains the dorsal pancreas joins the duct draining the ventral pancreas to form the main pancreatic duct (of Wirsung); the rest of the dorsal duct becomes the accessory pancreatic duct (of Santorini) and enters the duodenum 2.5 cm proximal to the main duct. In fetal life, the common bile duct and main pancreatic duct are dilated at their junction to form the ampulla of Vater. In extra-uterine life, only 10% of individuals retain this ampulla, although most retain a short common channel between the two duct systems.
The pancreas lies retroperitoneally, behind the lesser sac and stomach. The head of the gland lies within the C-loop of the duodenum, with which it shares a blood supply from the coeliac and superior mesenteric arteries (Fig. 15.2). The superior mesenteric vein runs upwards to the left of the uncinate process, and joins the splenic vein behind the neck of the pancreas to form the portal vein. The body and tail of the pancreas lie in front of the splenic vein as far as the splenic hilum, and receive arterial blood from the splenic artery as it runs along the upper border of the gland. The intimate relationship of the friable pancreas to these major blood vessels is the reason that bleeding is problematic after pancreatic trauma. The close association between the common bile duct and the head of pancreas explains why obstructive jaundice is so common in cancer of the head of the pancreas, and why gallstones frequently give rise to acute pancreatitis.
Pancreatitis
Acute pancreatitis
Aetiology
Conditions associated with the development of acute pancreatitis are listed in Table 15.1 – gallstones and alcohol are by far the most important.
Table 15.1 Causes of acute pancreatitis
| Class | Specific causes |
|---|---|
| Toxic | Alcohol Medication Tropical |
| Genetic | Cystic fibrosis Hereditary pancreatitis SPINK1 mutation |
| Metabolic | Hypercalcaemia Hyperlipidaemia |
| Obstructive | |
| Inflammatory | |
| Physiological | Sphincter of Oddi dysfunction |
Gallstone pancreatitis
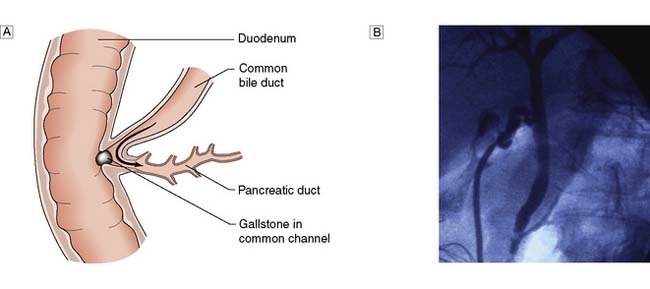
Gallstones are present in some 40% of patients in the UK who develop acute pancreatitis, but tiny gallstones or even microscopic crystals (so called microlithiasis) are thought to account for the majority of ‘idiopathic’ cases. Transient impaction of a gallstone within the common channel between the common bile duct and pancreatic duct causes obstruction of the pancreatic duct (Fig. 15.3) and a sequence of events within the pancreatic acinar cells resulting in intracellular activation of pancreatic enzymes, acinar cell damage and pancreatic inflammation.
Diagnosis
Radiology
Initial diagnosis of acute pancreatitis is based on clinical features combined with serum amylase levels. The role of radiology in initial assessment is confined to cases where there remains diagnostic doubt, as when serum amylase is non-diagnostic or where the clinical history or examination findings are atypical (for example when there is evidence of generalized peritonitis). In these cases urgent contrast-enhanced CT is mandatory. In patients with acute pancreatitis, changes will be identified ranging from mild peripancreatic oedema through to extensive pancreatic necrosis (Fig. 15.4) but more importantly at this stage, other diagnoses which require urgent operative intervention, such as mesenteric ischaemia or perforated viscus, will be excluded.
Management
Conservative treatment
• Pain relief. Severe pain requires the administration of opiates; there is no evidence to support the use of pethidine rather than morphine.
• Fluid resuscitation. Patients with severe acute pancreatitis often require large volumes of fluid to maintain adequate urine output and blood pressure. Adequate early resuscitation in such cases is the most important consideration in early management and where systemic organ dysfunction is present will necessitate invasive monitoring of venous and arterial pressure. Patients with MODS or SIRS will need oxygen therapy and continuous monitoring of oxygen saturation as well as urine output.
• Suppression of pancreatic function. There is no evidence that suppression of pancreatic function improves the outcome in acute pancreatitis. Nasogastric tubes are not routinely used. Fluids and diet are withheld until nausea and vomiting settle and in cases where systemic complications or other factors prevent recommencement of normal diet, nasoenteric feeding is commenced at an early stage. Suppression of pancreatic secretion by drugs such as octreotide or somatostatin is of no benefit in acute pancreatitis.
• Prevention of infection. Antibiotic prophylaxis has been advocated by some as a means of reducing the risk of infected pancreatic necrosis. Others have been concerned that the more widespread use of antibiotics will result in an increased incidence of severe fungal infection. The most recent consensus is that there is no evidence that prophylactic antibiotics reduce the incidence of infected pancreatic necrosis or mortality (EBM 15.1). It is important to recognize that patients with severe acute pancreatitis often have evidence of SIRS and the presence of a fever and raised white cell count are to be expected, even in the absence of infection. The only definite indication for early antibiotic therapy is when patients are suspected of having cholangitis, which may co-exist with gallstone pancreatitis. Jaundiced patients with SIRS are therefore managed with appropriate broad spectrum antibiotics while arrangements are made for urgent ERCP as described below.
• Inhibition of inflammatory response. Severe acute pancreatitis is one of many conditions where systemic organ dysfunction is driven by the systemic inflammatory response and there has been much experimental and clinical interest in the role of down-regulation of this response as a potential treatment for acute pancreatitis. The only agent that has been studied in large, prospective clinical trials was the platelet-activating factor (PAF) antagonist, lexipafant. Despite encouraging experimental data and promising results from initial clinical trials, a large international trial, recruiting 1500 patients, showed no difference in mortality.
• Nutritional support. Patients with severe acute pancreatitis who are unable to resume normal diet within 48–72 hours require nutritional support. This is best delivered by an enteral rather than parenteral route as meta-analyses of randomized trials (EBM 15.2) have demonstrated that TPN has a higher rate of complications and mortality. There are also sound experimental reasons to believe that enteral nutrition has additional benefits by potentially reducing the risk of bacterial translocation from the gut. There is no evidence that nasojejunal feeding is better or safer than nasogastric feeding but the nasojejunal route will be required where gastric stasis or outlet obstruction prevent effective nasogastric delivery.
• Other measures. A recent randomized trial assessed the role of probiotic therapy as an adjunct to early enteral feeding in the hope that this might reduce bacterial translocation from the gut more than enteral nutrition alone, thus potentially preventing later septic complications. Unfortunately, probiotic therapy actually increased mortality due to gut ischaemia and should no longer be used in these patients. Other proposed treatments which have been found to be of no benefit in prospective clinical trials include antiprotease therapy and peritoneal lavage.
15.1 Prophylactic antibiotics in severe acute pancreatitis
Bai Y, Gao J, Zou DW, Li ZS. Prophylactic antibiotics cannot reduce infected pancreatic necrosis and mortality in acute necrotizing pancreatitis: evidence from a meta-analysis of randomized controlled trials. Am J Gastroenterol 2008; 103(1):104–110.
Endoscopic treatment
Gallstone pancreatitis is due to the transient impaction of a stone at the papilla causing pancreatic duct obstruction. There is good experimental evidence that the duration of this obstruction is an important determinant of the severity of an attack and so early removal of an impacted gallstone by ERC and sphincterotomy has long been proposed as a potential treatment option for patients. Unfortunately the results from randomized trials have been conflicting, and differences in study design have made direct comparisons difficult. Patients with evidence of obstructive jaundice and SIRS within the first 24 hours are suffering from or are at least at risk of developing cholangitis and there is broad consensus that these patients should have urgent ERC with sphincterotomy. However the majority of patients will pass the gallstone spontaneously and in this situation ERC carries additional risk and no potential benefit (EBM 15.3). The most recent meta-analysis of randomized trials shows no benefit from early ERC in patients with severe acute pancreatitis where cholangitis is not present. Early ERC with stone removal can however be life-saving in the patient with cholangitis and it is important to be alert to this possibility in patients diagnosed as having severe acute pancreatitis. Our own practice is to perform urgent ERC and sphincterotomy only in patients with acute pancreatitis associated with obstructive jaundice and SIRS but there is considerable variation in practice across the UK.
Surgical treatment
1. Where an alternative diagnosis is suggested by CT following initial assessment.
2. Where gallstones are considered the likely cause, cholecystectomy is carried out after recovery from the acute attack. In patients with mild acute pancreatitis this is best carried out during the index hospital admission but following a severe attack, cholecystectomy is delayed until resolution of the inflammatory process. Even after severe acute pancreatitis it is usually possible to perform cholecystectomy by the laparoscopic route. In patients who have had no prior imaging of the common bile duct by MRCP or ERC, it is important to carry out operative cholangiography to exclude bile duct stones. In patients considered unfit for cholecystectomy, ERC with endoscopic sphincterotomy is carried out to protect against further attacks.