Chapter Twenty-Four. The nature of bone—the female pelvis and fetal skull
The nature of bone: function and structure
Functions of bone
Bone is a highly vascular, constantly changing, hard mineralised connective tissue (Guyton & Hall 2006) which contains depositions of calcium and phosphorus. It performs important functions for the body:
• Support and protection of the soft organs.
• Movement by acting as anchorage for muscles and levers.
• Storage of fat.
• Large reservoir of calcium and phosphorus.
• Storage of smaller amounts of potassium, sulphur, magnesium and copper.
• Blood cell formation.
Structure of bone
Bone is a living matrix consisting of three basic components: an organic matrix of collagen known as osteoid, a cartilage-like material differing from cartilage in that calcium salts are readily deposited in it, a mineral matrix of calcium and phosphorus and bone cells which include osteoblasts, osteoclasts and osteocytes. Calcium (Ca 2+), the most common mineral in the body, and phosphorus are present in bone as crystals of hydroxyapatite, (Ca 3(PO 4) 2) 3·Ca(OH) 2, attached to collagen fibres. This results in the hardness of bone. Bone is continually being remodelled as osteoblasts deposit new bone and osteoclasts reabsorb it. Calcium and phosphorus are slowly exchanged between bone and extracellular fluid (ECF). Bone can be divided into compact (lamellar) bone and spongy (trabecular) bone (Guyton & Hall 2006).
Bone cells
• Osteoblasts are present on all bone surfaces in single layers next to the unmineralised osteoid of newly forming bone. They may be differentiated from haemopoietic stem cells. They are uniformly sized and linked together by cytoplasmic processes. Osteoblasts synthesise and secrete the constituents of the organic matrix and promote mineralisation.
• Osteocytes are derived from osteoblasts that have become trapped in lacunae. They maintain the bone matrix and if they die the surrounding matrix is absorbed.
• Osteoclasts reabsorb bone and are found on or near surfaces undergoing erosion. They may have developed separately to osteoblasts and derive from monocytes. They vary greatly in size and nuclear form and are very mobile. Osteoclasts contain both proteolytic enzymes and acids such as lactic acid and citric acid which remove both the organic and mineral matrix.
Compact bone
Compact bone forms the outer rim or cortex of all bones and consists of osteons or Haversian systems. There is a central Haversian canal oriented to the long axis of the bone. Running at right-angles to the long axis of the bone are secondary canals called perforating or Volkmann’s canals which carry nerves, blood vessels and lymphatic vessels. Around the central canal are concentric hollow tubes of bone called lamellae. Each lamella has small concavities at its junctions with others called lacunae which contain the spider-shaped osteocytes. Hair-like canals called canaliculi connect the lacunae to each other and to the central canal, linking all the osteocytes in an osteon together. This facilitates exchange of nutrients and removal of waste products.
Spongy bone
Spongy bone contains far fewer Haversian systems and is made up of a lattice of trabeculae with red or fatty bone marrow filling the cavities (Figure 24.1 and Figure 24.2). Trabeculae are only a few cell layers thick and contain irregularly arranged lamellae and osteocytes connected by canaliculi. There are no osteons present. Nutrients arrive at the osteocytes by diffusing through narrow spaces between bony spicules. The tiny struts of bone are arranged to combat the stress placed on the bone during activity.
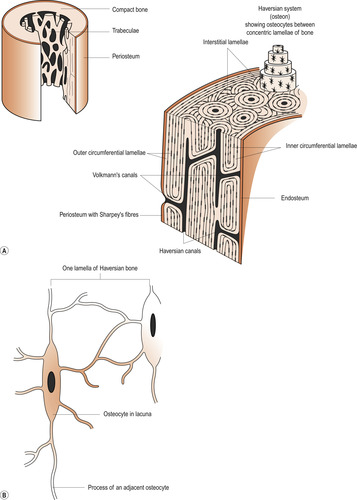 |
| Figure 24.1 Structure of compact bone. (From Hinchliff S M, Montague S E 1990, with permission.) |
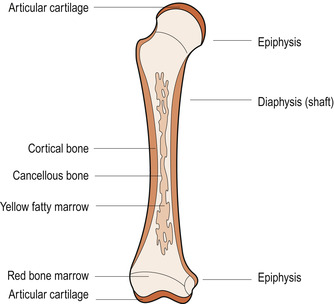 |
| Figure 24.2 Anatomical features of a long bone. (From Hinchliff S M, Montague S E 1990, with permission.) |
Periosteum and endosteum
Most bones have a tough outer covering of fibrous connective tissue, the periosteum, which does not cover the articular surfaces of joints. Periosteum transmits blood vessels and acts as an attachment surface for ligaments and muscles. It is supplied abundantly with nerve fibres. Beneath this is a layer of osteoblasts. Lining the marrow cavity is the endosteum, a layer of tissue containing the osteoblasts and osteoclasts.
Calcium and phosphorus metabolism
There are about 1000 g of calcium in an adult, of which the skeleton contains 99%, leaving only 10 g available for other cellular processes (Hinson et al 2007). The small amount of calcium found in body fluids and cells plays an important part in metabolic processes and is maintained within narrow limits. Phosphorus is also crucial to body function and the skeleton contains 85%. The normal plasma concentration of calcium is 2.10–2.70 mmol/L and of phosphate 0.70–1.40 mmol/L.
Functions of calcium
Calcium is an intracellular and extracellular ion with many functions. It is present in ECF in two forms: half is bound to the proteins albumin and globulin and half is in an ionised form (Ca 2+) which is important in many cell activities (Hinson et al 2007):
• Nerve and muscle function.
• Hormonal actions.
• Blood clotting.
• Cell motility.
• A secondary messenger between environmental stimulus and cell function by modulation of enzyme response when bound to the protein calmodulin.
Functions of phosphorus
Phosphorus in the form of phosphates plays a large role in cellular function:
• As a component of nucleic acids.
• By regulating energy storage as adenosine triphosphate (ATP).
Hormonal control of calcium and phosphorus metabolism
Regulation of calcium balance is closely associated with that of phosphate. There is continuous exchange of calcium between different sites (calcium pools) in the body. Three hormones control calcium and phosphorus metabolism by maintaining the concentration of calcium in ECF. These are parathyroid hormone (PTH), vitamin D and calcitonin. Plasma inorganic phosphate is more loosely controlled than calcium (Hinson et al 2007).
If there is no change in the amount of skeletal calcium, ECF calcium level depends on the balance between calcium absorption in the gut and its excretion in urine and faeces. About 50% of calcium in the blood passing through bone capillaries is exchanged in a single passage and about 300 mmol of calcium is involved in calcium exchange between blood and bone every day.
Parathyroid hormone
Four parathyroid glands which are embedded in the thyroid gland secrete parathyroid hormone (PTH). PTH increases the concentration of Ca 2+ in blood and depresses plasma phosphate concentration by acting on bone and kidneys. PTH increases osteocyte reabsorption of bone with a rapid release of calcium and phosphorus into the blood. Calcium reabsorption in the kidney tubules is increased but the excretion of phosphate is increased. This results in a rise in plasma calcium and a fall in plasma phosphate. PTH activity is directly related to serum calcium concentration. When plasma calcium level rises, PTH production falls, resulting in calcium deposition in bone, and vice versa.
Vitamin D
The D vitamins are steroid substances formed from ergosterol in plants and 7-dehydrocholesterol in animals. Ultraviolet radiation modifies these to ergocalciferol (vitamin D 2) and cholecalciferol (vitamin D 3). Humans can either ingest vitamin D from plants and animals or manufacture it by the action of sunlight on skin to form cholecalciferol. Vitamin D has to be further metabolised by adding hydroxyl groups before it can become active. The liver first converts it to 25-hydroxycholecalciferol and the kidney produces the active form 1,25-dihydroxycholecalciferol (calcitriol) in response to PTH stimulation. Calcitriol is released into the circulation and transported to its target organs of intestine, bone and kidneys (Hinson et al Chew 2007).
Calcitonin
Calcitonin is secreted by the parafollicular cells ( clear or C cells) of the thyroid gland. Its main effect is opposite to PTH, causing a fall in plasma calcium and phosphate concentrations. This hormone may play a part in skeletal growth in children but appears to have no role in adults other than in pregnant women. Calcitonin secretion is directly related to plasma calcium concentration.
The pelvic girdle
The pelvic girdle offers attachment for the lower limbs and for support of the pelvic and, to some extent, the abdominal organs. In an upright posture the pelvic girdle transmits the weight of the trunk to the legs, so the sacroiliac joints must be strong and stable. The size, shape and rigidity of the pelvic girdle is related directly to bipedal locomotion and the human pelvis compared to other primates is short, squat and basin-shaped (Trevathan et al 1999).
The mammalian spine is highly efficient for walking on four legs as the abdominal organs are suspended from a single horizontal arch (the backbone). This single arch is present in the human neonate but when babies sit up their spines develop a forward curve near the top. When babies stand their spines develop a second forward curve near the base. Both curves are essential for maintaining an upright posture.
The evolving changes in pelvic shape placed limits on the baby’s head size, limiting human gestation length and resulting in an immature baby (Morgan 1990), a feature referred to as altricial (see Ch. 57). The gynaecoid pelvis is adapted for giving birth to a comparatively large-headed baby but mechanisms of labour are necessary to facilitate descent of the head through the pelvis. These include passive alterations to fetal position and moulding of the fetal skull.
Pelvic bones
Although diagrams and text can illustrate features of the pelvis there is no substitute for handling a life-size model. Familiarity with the shape and size of the pelvis may enable life-saving decisions to be made. During vaginal examinations relevant pelvic features must be identified in vivo.
The pelvis is made up of four irregularly shaped bones: two innominate bones forming the lateral and anterior walls, and the sacrum and coccyx forming the posterior wall. Each innominate bone consists of three fused bones: the ilium, ischium and pubis. These were formed as cartilage in the fetus and their ossification centres begin to fuse at puberty and is completed about age 25. The description of these bones is mirrored to the left and right of the pelvis.
The ilium
The ilium has an upper flat plate of bone and forms part of the acetabulum below (Figure 24.3 and Figure 24.4). The external part of the plate of bone is curved and has a roughened surface for attachment of the gluteal muscles which form the buttocks. The inner surface forms the iliac fossa which is smooth and concave. The iliacus muscle, which forms a platform on which the abdominal organs rest, originates from this surface. The upper ridge of the ilium is called the iliac crest and is S-shaped. The muscles of the abdominal wall have attachments to this surface.
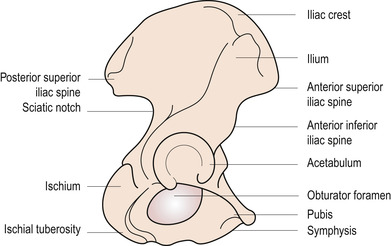 |
| Figure 24.3 The outer or lateral surface of the right innominate bone. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
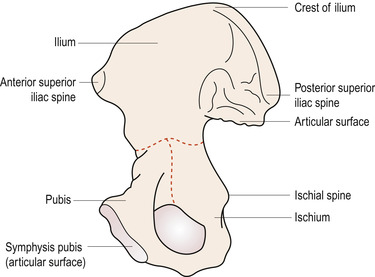 |
| Figure 24.4 The inner or medial surface of the right innominate bone. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
At the anterior end of the iliac crest is the anterior superior iliac spine, which can be identified under the skin. At the posterior end is the posterior superior iliac spine, marked externally by a dimple at the level of the second sacral vertebra. Two inferior iliac spines, anterior and posterior, can be found below the superior spines. The lower margin of the ilium forms two-fifths of the acetabulum where it fuses with the ischium and pubis. Behind the acetabulum the ilium forms the greater sciatic notch, through which nerves from the sacral plexus pass. Above the greater sciatic notch is the area of the ilium which articulates with the sacrum at the sacroiliac joint.
The ischium
The ischium forms the lowest aspect of the innominate bone. The upper part forms two-fifths of the acetabulum, where it fuses with the ilium and pubis. Below the acetabulum, a thick buttress of bone called the ischial tuberosity takes the weight of the seated body. The hamstring muscles of the thigh arise from this bone. Passing upwards and inwards from the ischial tuberosity, a shaft of ischium meets the inferior ramus of the pubic bone to form the pubic arch.
The ischium also forms the lower border of the obturator foramen, a large opening in the lower part of the innominate bone below the acetabulum. On its internal surface, protruding from its posterior edge and about 5 cm above the tuberosity is the ischial spine, an important landmark to be found on virginal examination. The ischial spine separates the greater sciatic notch from the lesser sciatic notch.
The pubis
This square-shaped bone forms the anterior aspect of the innominate bone. The two pubic bones articulate medially to form a joint called the symphysis pubis. Laterally, the superior ramus of the pubic bone forms one-fifth of the acetabulum. The superior ramus also forms the upper boundary of the obturator foramen. The inferior ramus passes downwards and outwards to join the ischium and form the pubic arch. The upper surface of the pubis forms the pubic crest ending laterally in the pubic tubercle.
The sacrum
The sacrum is a shield-shaped mass of bone formed from five fused sacral vertebrae (Fig. 24.5). It articulates with the two innominate bones at the sacroiliac joints. The anterior surface is smooth and concave, both from above downwards and from side to side, forming the hollow of the sacrum. The first sacral vertebra overhangs the sacral hollow and the central point of this projection is called the sacral promontory. Through the centre of the bone, sacral and coccygeal nerves pass in the sacral canal.
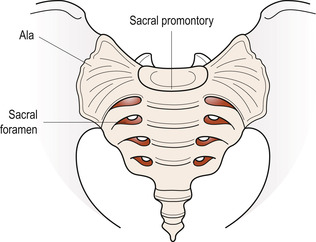 |
| Figure 24.5 The sacrum. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
Four pairs of foramina (openings) are present anteriorly between the five fused sacral vertebrae where sacral nerves exit to form the sacral plexus. Posteriorly, posterior branches of the sacral nerves pass through eight small foramina to supply the skin of the buttocks and the muscles of the lower back. On its upper surface a smooth oval area forms an articular surface for the fifth lumbar vertebra to form the lumbosacral joint. Lateral masses of bone on either side of the sacrum are called the wings of the sacrum or sacral alae.
The coccyx
This small triangular bone with its base uppermost is made of four fused coccygeal vertebrae. The first coccygeal vertebra articulates with the lower end of the sacrum to form the sacrococcygeal joint. The rudimentary vertebrae forming the rest of the coccyx are smooth on their inner surface and support the rectum. The external anal sphincter is attached to the lowest point.
Pelvic joints
There are four pelvic joints: one symphysis pubis, two sacroiliac and one sacrococcygeal joint:
• The symphysis pubis consists of an oval disc of fibrocartilage about 4 cm long lying between the two pubic bones. The joint is reinforced by ligaments crossing from one pubic bone to the other.
• The sacroiliac joints are synovial joints with a cavity filled with synovial fluid, a capsule formed of synovial membrane and tough external supporting ligaments. There are very strong posterior ligaments which transmit the weight of the trunk, head and arms to the legs. Movement of these joints is slight but increases in range during pregnancy when relaxin softens the ligaments.
• The sacrococcygeal joint lies between the sacrum and coccyx. There is sometimes a small synovial joint cavity present. Slight movement can occur backwards and this is increased greatly when the baby’s head passes through the pelvis in labour.
Pelvic ligaments
Besides the ligaments supporting the pelvic joints, there are three other pairs of ligaments:
• The sacrotuberous ligament crosses from the posterior superior iliac spine and the lateral borders of the sacrum and coccyx to the ischial tuberosity. It bridges the greater and lesser sciatic notches.
• The sacrospinous ligament passes in front of the sacrotuberous ligament from the side of the sacrum and coccyx, crosses the greater sciatic notch and attaches to the ischial spine.
• The inguinal ligament (Poupart’s ligament) runs from the anterior superior iliac spine to the pubic tubercle and forms the groin.
Regions of the pelvis
There is a clear line of bone called the pelvic brim separating the upper flare of the iliac fossae which is the false pelvis from the basin-shaped part of the pelvis which is the true pelvis. The true pelvis has a cavity and outlet through which the fetus passes during birth.
The pelvic brim
Landmarks are identifiable on the pelvic brim (inlet) and important measurements are made between them. In the normal gynaecoid (female) pelvis the brim is oval in shape with the anteroposterior diameter reduced by the sacral promontory. Starting at the centre of the sacral promontory and tracing the brim round to the symphysis pubis, the landmarks are (Fig. 24.6):
• The sacral promontory.
• The sacral ala.
• The upper border of the sacroiliac joint.
• The ileopectineal line.
• The ileopectineal eminence.
• The inner upper border of the superior pubic ramus.
• The inner upper border of the body of the pubis.
• The inner upper border of the symphysis pubis.
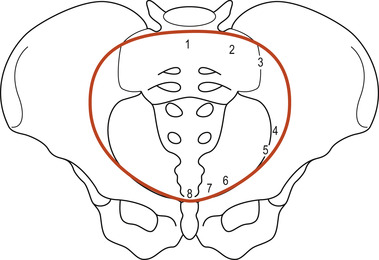 |
| Figure 24.6 The pelvic brim. 1, sacral promontory; 2, sacral ala; 3, sacroiliac joint; 4, ileopectineal line; 5, ileopectineal eminence; 6, superior pubic ramus; 7, body of pubic bone; 8, symphysis pubis. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
If a piece of paper is placed across the landmarks, an imaginary flat surface is formed. This is called a plane and the concept is also applied to the cavity and outlet. The pelvic diameters are measured from landmarks across the planes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


