■ Because there are few physical exam findings associated with GERD, the physical exam should focus on conditions that might suggest an alternative explanation for the patient’s symptoms. These include recent weight loss or progressive inability to tolerate solids and liquids (malignancy), atypical symptoms associated with exertion (coronary artery disease or asthma), or diarrhea (irritable bowel syndrome).
■ The presence of abdominal surgical scars or abdominal wall hernias is important to identify if laparoscopic LES augmentation surgery is being considered as they may make access to the peritoneal cavity and the gastroesophageal (GE) junction challenging.
■ Laparoscopic LES augmentation surgery, which involves placement of a magnetic device around the GE junction, is considered not safe for magnetic resonance imaging (MRI). Patients should be aware of this contraindication prior to surgery.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Establishing GERD as the etiology of the patient’s symptoms is critical before proceeding with any intervention. Patients may have subjective complaints of heartburn or dysphagia that are unrelated to their reflux disease. The four diagnostic tests that are most commonly used to establish a diagnosis are upper endoscopy, barium esophagram, pH testing, and manometry.
■ Upper endoscopy (esophagogastroduodenoscopy [EGD])
■ All patients undergoing an antireflux procedure should have an EGD.
■ EGDs can identify the presence of hiatal hernias and rule out other pathology, which may be contributing to the patient’s symptoms, such as peptic ulcer disease or malignancy.
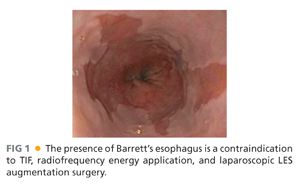
■ GERD-related complications such as esophagitis, Barrett’s esophagus, and esophageal strictures can also be identified (FIG 1).
■ Ambulatory pH testing
■ This is considered to be the gold standard test for diagnosing the presence of symptomatic GERD.
■ Patients should typically not be taking their antireflux medications when the study is performed.
■ pH testing can be performed via catheter-based systems (i.e., 24-hour pH probe testing) or wireless systems (i.e., 48-hour Bravo testing).
■ Both catheter-based and wireless systems allow for the quantification of six variables including total/upright/supine time that the pH is less than 4, number of reflux episodes, number of episodes longer than 5 minutes, and longest episode. These variables can be combined to calculate the “DeMeester score,” which is used by many surgeons as definitive evidence for the presence of GERD.1
■ Barium esophagram
■ This is a dynamic fluoroscopic study that characterizes both anatomic and functional aspects of the esophagus. It involves multiple swallows of barium and barium-coated solid food.
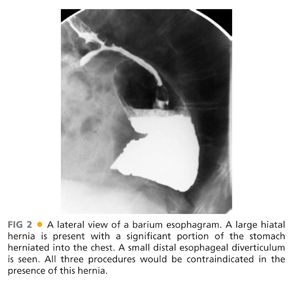
■ The two most important things to characterize with a barium esophagram are the position of the GE junction relative to the diaphragmatic hiatus and overall esophageal motility. The presence of a large hiatal hernia (FIG 2) or significant esophageal dysmotility is a contraindication for any of the three procedures.2
■ Esophagrams can also identify the presence of reflux that is characterized by the spontaneous reflux of barium back into the esophagus. However, they are less sensitive than pH studies and thus a negative finding here does not rule out GERD.
■ Video recording of this study is crucial because it allows the surgeon to actively assess esophageal peristalsis and the functional significance of hiatal hernias.
■ Manometry
■ Esophageal manometry uses pressure transducers within a transnasal catheter to provide data regarding the LES resting pressure, LES abdominal and total length, and adequacy of LES relaxation. It also characterizes esophageal motility by quantifying the amplitude, duration, and propagation of each contraction.
■ The presence of significant esophageal dysmotility is a contraindication for all three procedures.
■ Multichannel impedance testing and gastric emptying studies are also used on occasion to identify nonacidic GERD and assess gastric functionality, respectively.
TECHNIQUES
TRANSORAL INCISIONLESS FUNDOPLICATION
■ Approved by the U.S. Food and Drug Administration (FDA) in 2007, the only TIF device that is currently available for use in the United States is the EsophyX device (EndoGastric Solutions, Redmond, WA).
■ EsophyX re-creates the LES by plicating the distal esophagus and the gastric cardia together, thus creating an antireflux valve similar to that of a laparoscopic Nissen fundoplication.
■ The device consists of a handle, an 18-mm diameter shaft, a tissue invaginator composed of holes in the side of the device (which are connected to a suction device), an articulating arm, which approximates gastric and esophageal tissue and deploys the tissue fasteners, a helical screw, two stylets, and 20 polypropylene H-fasteners (10 plication sets) (FIG 3).

Preoperative Planning
■ At our institution, general anesthesia is administered and the procedure is performed in the operating room.
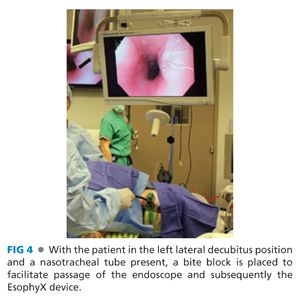
■ Nasotracheal intubation is performed so the oropharynx can be used entirely for the EsophyX device. A bite block is placed to protect the teeth from the device and scope.
■ Two physicians perform the procedure. One manipulates the endoscope while the other controls the device.
Positioning
■ After intubation, the patient is placed into the left lateral decubitus position with the head elevated slightly (FIG 4).
■ Prophylactic antibiotics are administered before the procedure begins because transluminal fasteners are placed, which may increase the risk of postoperative infections.
Placement of the Transoral Incisionless Fundoplication Device into the Stomach
■ Preprocedure endoscopy is performed to verify anatomic landmarks.
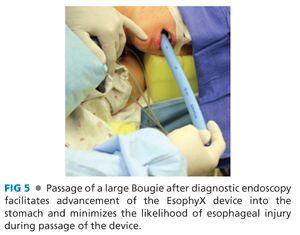
■ A 56-Fr bougie is inserted into the esophagus and then removed to facilitate subsequent passage of the EsophyX device (FIG 5).
■ The EsophyX device is lubricated and a standard endoscope is threaded through the device (FIG 6). Both are placed through a bite block and advanced through the esophagus into the stomach.
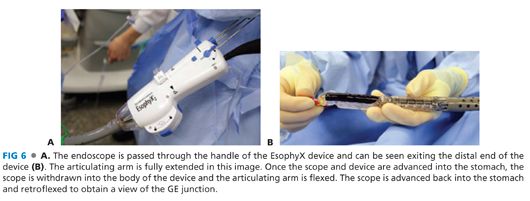
■ The scope is advanced into the gastric lumen and then retroflexed to examine the GE junction. Using a standard, high-flow insufflator, the stomach is insufflated with carbon dioxide to a pressure of 15 mmHg via the working channel of the endoscope. Once the articulating arm is visualized within the stomach, the scope is withdrawn into the device, the articulating arm is flexed, and the scope is then advanced back into the retroflexed position within the gastric lumen (FIG 7).

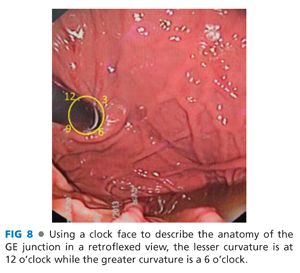
■ Using the retroflexed view, the GE junction is envisioned as a clock face with the 12 o’clock position located at the lesser curvature, the 6 o’clock position at the greater curvature, and the 9 o’clock position located along the posterior gastric wall (FIG 8).3
Anterior Rotational Plication Fasteners
■ The closed articulating arm is placed at the 12 o’clock position (FIG 9A). The helix retractor portion of the device is also at the 12 o’clock position and advanced into the squamocolumnar junction (FIG 9B). The entire device is then advanced distally a couple of centimeters and rotated clockwise on the screen. This allows the articulating arm to be opened and the helical retractor disengaged from the articulating arm.
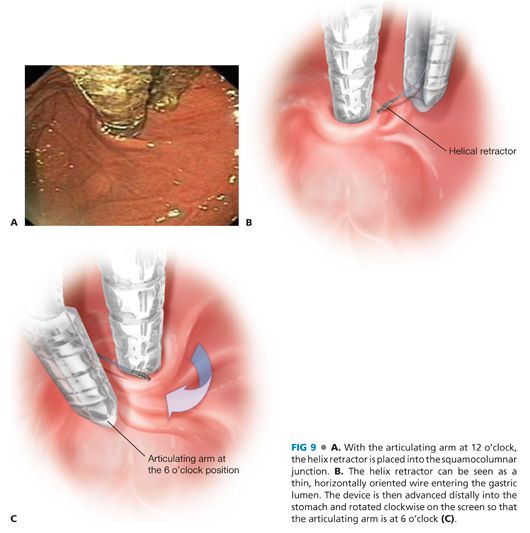
■ The articulating arm is then rotated back to the 6 o’clock position, partially closed, and pulled back 1 to 2 cm (FIG 9C). The GE junction is advanced caudally by applying tension to the helical retractor.
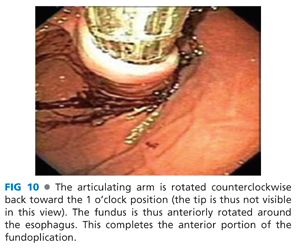
■ The stomach is then desufflated and the articulating arm is rotated toward the 1 o’clock position. This maneuver rotates the fundus anteriorly around the esophagus thereby initiating the fundoplication. Externally, the handle of the device is rotated approximately 180 degrees (FIG 10). This has been described in the literature as the “Bell Roll maneuver.”3
■ The helical retractor and articulating arm are secured in place and the suction is applied.
■ The first H-fastener set is then deployed.
■ The stomach is then reinsufflated to visualize deployment of a pair of H fasteners. Two sets of additional H fasteners are subsequently placed at varying distances from the GE junction.
■ This will result in the placement of six fasteners 1 to 3 cm above the squamocolumnar junction.
Posterior Rotational Plication Fasteners
■ The helix retractor portion of the device is maintained at the 12 o’clock position.
■ The articulating arm is rotated counterclockwise through the lesser curve to the 8 o’clock position, partially closed, and pulled back 1 to 2 cm. The GE junction is advanced caudally by applying tension to the helical retractor.
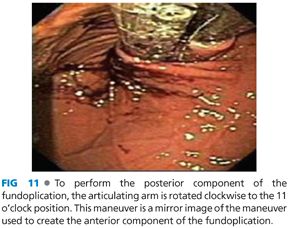
■ The “Bell Roll” maneuver is again performed, but this time in the clockwise direction (clockwise on the screen). The stomach is desufflated and the articulating arm is rotated clockwise to the 11 o’clock position. This maneuver rotates the fundus posteriorly around the esophagus (FIG 11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


