The Continent Ileostomy
Eric J. Dozois
Roger R. Dozois
Introduction
The continent reservoir ileostomy, commonly referred to as the Kock pouch, comprises an internal ileal reservoir that stores stool and gas between intubations, a stoma and outflow tract needed to intubate and evacuate the contents of the reservoir, and a surgically created biologic valve interposed between the other two components to act as a pressure barrier and provide continence. The major advantages of this operation over the conventional spout ileostomy are the elimination of the necessity for the patient to continually wear an external appliance and a much less conspicuous stoma.
Historical Background and Rationale
Although patients and their caregivers recognize the benefits of proctocolectomy and Brooke ileostomy, a curative operation that restores the patient’s health, it has become evident that for many ileostomates, the need to constantly wear an external appliance to collect the effluent of an incontinent stoma can interfere with some of their daily activities and their social life, and can be detrimental to their overall quality of life. Also, the material necessary to pouch the stoma is expensive. Although an incontinent Brooke-type stoma is acceptable to most ostomy patients, primarily because they regain their general health, as many as 40% of these patients long for a better alternative. By surgically devising an internal reservoir capable of collecting the bowel contents and by rendering it continent by adding a valve mechanism so that patients no longer have to wear an external appliance, Nils Kock of Göteborg, Sweden, revolutionized the concept of surgically created continence and unknowingly paved the way for the ileal pouch anal anastomosis.
The construction of an intestinal reservoir to substitute for the loss of rectal capacity evolved rapidly when a U-shaped, double-folded reservoir was designed by Kock and his colleagues. The means to achieve continence, however, were slower to evolve. At first, Kock hoped that continence could be achieved by external compression of the outflow tract brought through the rectus abdominis muscle, but this proved unreliable. Interposition of an antiperistaltic segment of ileum between the reservoir and the stoma also proved inefficient. In 1972, Kock ingeniously devised the intussusception ileal valve, the so-called nipple valve, using an isoperistaltic portion of the outflow tract, which resulted in a far more reliable continence mechanism.
A number of technical refinements were later added to compensate for the weaker mesenteric side of the intussuscepted ileal segment, including stripping off the peritoneum and defatting the mesentery of the valve, placement of “rotation” sutures, reinforcement by a mesenteric sling of synthetic mesh encompassing the outflow tract, and stapling the antimesenteric side of the valve to the side wall of the reservoir.
At the Mayo Clinic, the efforts to construct and perfect the continent ileostomy were spearheaded by Oliver H. Beahrs in the early 1970s. Initially, the valve was made 3 cm in length and anchored in place with through-and-through nonabsorbable silk sutures. Subsequently, and with the hope of reducing valve slippage and valve fistula, the nipple was made longer (5 cm), and was anchored in place with both absorbable sutures and staples, and then interrupted sutures were added between the base of the reservoir and the outflow tract to further anchor the intussusceptum. We have been reluctant to use Marlex mesh, which may result in fistula formation across the nipple valve.
Although the ileal pouch anal anastomosis is now preferred by most patients requiring proctocolectomy, the continent ileostomy remains a viable alternative to the Brooke ileostomy for certain categories of patients, which include (a) patients with an existing conventional Brooke ileostomy with no possibility of an ileal pouch anal anastomosis (no anal sphincter) who want to improve their quality of life, (b) patients requiring a proctocolectomy who wish to preserve continence but are not suitable candidates for an ileoanal anastomosis, most often because of poor anal sphincter function, (c) the rare patients whose daily work takes them away from toilet facilities for long periods of time and who prefer a continent ileostomy to an ileoanal anastomosis, and (d) patients with a failed ileoanal anastomosis who desire to preserve continence and avoid an external appliance if the failure is unrelated to Crohn disease or severe pouchitis.
Use of the Kock pouch should be discouraged in (a) older patients who may be more prone to postoperative complications, including valve dysfunction, and may not tolerate reoperation, (b) patients with Crohn disease, (c) obese patients, (d) critically ill patients such as those with toxic megacolon, (e) psychologically unfit patients who may not be able to intubate properly or tolerate complications and reoperations, and (f) patients in whom a significant amount of small intestine has already been removed.
The Operation
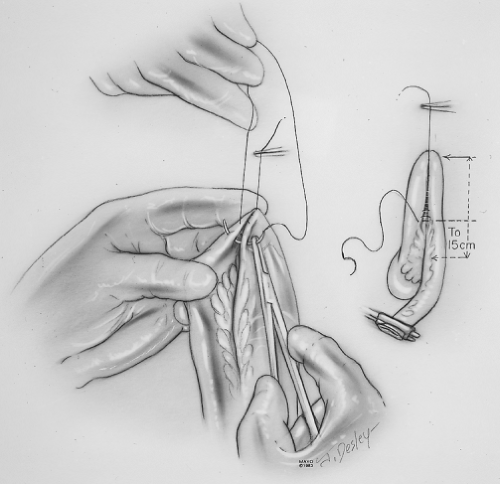
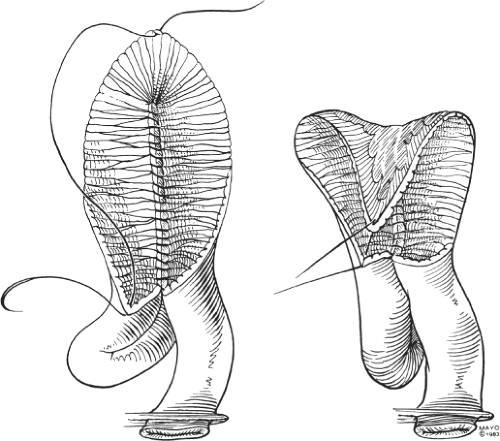
The distal 45 cm of the ileum is used to construct the reservoir, the valve, and the outflow tract (efferent limb). Beginning 15 cm from the cut end of the distal ileum, a 30-cm segment of ileum is measured and fashioned into a U (Fig. 1). The antimesenteric borders of the two 15-cm limbs of the U are approximated with continuous suture of 2-0 chromic catgut. The two limbs are then incised on their antimesenteric borders, with the incision extending 4 to 5 cm longer on the afferent limb than on the efferent limb so that the two limbs separate as the pouch is constructed. A second layer of continuous chromic catgut is used to approximate the mucosa and complete the posterior wall of the reservoir (Fig. 2).
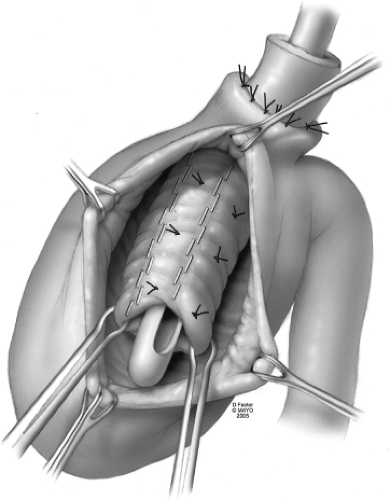
The valve is then fashioned. The serosal surface of the efferent limb of the ileum is scarified, with the electrocautery beginning at the pouch and extending for a distance of 10 cm toward the cut end. The peritoneum of that same segment is also stripped from the adjacent mesentery, which is also defatted. These maneuvers are designed to promote the adherence of the ileum and its mesentery when the efferent limb is intussuscepted into the pouch to fashion the valve.
The 10-cm efferent limb is intussuscepted into the pouch to form a nipple valve of <5 cm in length. The intussusceptum is fixed in place with through-and-through sutures of 2-0 Vicryl (polyglactin 910) and three cartridges of stainless steel staples along both sides of the mesentery, care being taken to avoid injury to the vascular
supply, and immediately opposite the mesentery using the GIA (U.S. Surgical Corp., Norwalk, CT, USA) autosuture apparatus (Fig. 3). The placement of the staples and sutures is facilitated by “stenting” the lumen of the intussusceptum with a No. 28 French catheter.
supply, and immediately opposite the mesentery using the GIA (U.S. Surgical Corp., Norwalk, CT, USA) autosuture apparatus (Fig. 3). The placement of the staples and sutures is facilitated by “stenting” the lumen of the intussusceptum with a No. 28 French catheter.
The bottom of the U is then folded over to construct the anterior wall of the reservoir, using two layers of continuous 2-0 chromic catgut (Fig. 2). The outflow tract is sutured to the base of the pouch with interrupted 3-0 nonabsorbable sutures at the exit of the limb from the pouch to further anchor the intussusceptum in place (Fig. 3).
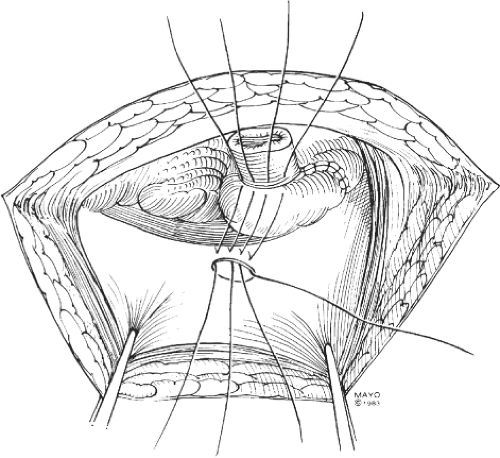
A circumferential defect is created through the abdominal wall just above the pubic hairline in the right lower quadrant, and the outflow tract is brought through the defect and amputated flush with the skin and matured into a stoma with interrupted 3-0 chromic catgut. The length of ileum between the pouch and the stoma should be kept short to avoid tortuosity and facilitate later intubation of the reservoir. This is aided by suturing the pouch to the undersurface of the anterior abdominal wall so that the nipple valve is perfectly aligned with the stoma (Fig. 4).
A No. 28 French catheter is passed through the stoma, efferent limb, and nipple valve, and its tip is positioned within the lumen of the pouch before the incision is closed. A suture of heavy silk is tied around the catheter at the level of the stoma so that the exact position of the catheter can easily be ascertained in the postoperative period. These precautions help prevent pouch perforation or tube slippage during postoperative recovery.
In the immediate postoperatiave days, the ileal pouch is irrigated with 25 mL of physiologic saline twice a day to maintain the patency of the catheter, which is connected to a drainage bag. When spontaneous bowel function returns, oral alimentation can be resumed. Before dismissal from the hospital, approximately 8 to 10 days postoperatively, patients are taught self-catheterization by the stoma therapist.
On leaving the hospital, patients are given a catheter designed to drain the pouch (either an ileostomy catheter, M8730 [Atlantic Surgical Co. Inc., Merrick, NY, USA], or an ileal pouch catheter [Dow-Corning Co., Midland, MI]). The Atlantic ileostomy
catheter has a diameter of ∼9 mm (No. 28 French) and a length of 30 cm, whereas the Dow-Corning ileal pouch catheter has a diameter of approximately 1 cm (No. 30 French) and a length of approximately 64 cm. Each catheter has a thin wall and large holes at the insertion end just proximal to its bullet-shaped blunt tip. The patient keeps the catheter in a small plastic case, which is carried at all times.
catheter has a diameter of ∼9 mm (No. 28 French) and a length of 30 cm, whereas the Dow-Corning ileal pouch catheter has a diameter of approximately 1 cm (No. 30 French) and a length of approximately 64 cm. Each catheter has a thin wall and large holes at the insertion end just proximal to its bullet-shaped blunt tip. The patient keeps the catheter in a small plastic case, which is carried at all times.
When the patient experiences a sensation of fullness, the pouch requires emptying. To empty the pouch, the patient passes the catheter through the stoma into the pouch, usually in the sitting position. The ileal contents spontaneously drain by gravity through the catheter directly into the toilet or another suitable receptacle. The Valsalva maneuver and direct manual compression of the abdomen over the pouch area may at times facilitate drainage, but routine irrigations are not required. The catheter then is removed from the pouch, rinsed clean, and replaced in its case for later use. A soft gauze pad with a waterproof surface is taped over the stoma to absorb any mucus secreted by the stoma. Patients rapidly become proficient at this procedure, which requires 5 to 10 minutes to complete. None of our patients has ever perforated the pouch with the catheter.
Some patients have found that partially digestible substances, such as seeds, apple skins, celery, and mushrooms, may plug the catheter, so they have avoided these foods. Others, however, have found that all foods can be eaten, provided they are thoroughly masticated before being swallowed.
Four to 6 weeks after operation, restrictions on physical activities are removed. Pregnancy is not contraindicated. Many patients who have undergone this procedure have become pregnant and have delivered healthy babies, either vaginally or by cesarean section.