The Bassini Operation
Oreste Terranova
Luigi De Santis
Flavio Frigo
Edoardo Bassini (1844–1924)
Born in Pavia in 1844, Bassini was from a wealthy family of estate owners; he grew up in close contact with the land and its workers, living a comfortable life but without luxuries. The love for land and agricultural laborers remained in his heart throughout his life, even though his surgical career kept him a long way from his people and his land. Later in his life, he gave the poor workers the land that they worked.
Bassini received a degree in medicine at the University of Pavia when he was 22 years old. We do not know whether at this stage he had already decided to undertake a career as a surgeon. As a young man, he sympathized with liberal and patriotic ideas (at this time, northern Italy was under Austrian dominion) and he took part in demonstrations and riots. He was seriously wounded by a sharp weapon on his right iliac fossa. He was not subjected to any surgical care because the surgeons considered him completely inoperable. Fortunately, he survived, but he developed a stercoraceous fistula. He was then referred to the surgical authority of his native city, Professor Porta of Pavia. During the long stay in the surgical ward, the growing friendship and mutual esteem with Professor Porta were instrumental in persuading Bassini to begin a surgical career. He was warmly encouraged by Porta, who had early understood his gift for surgery while discussing complex and unresolved surgical problems. He was probably already considering new solutions to the still-unresolved problem of inguinal hernia.
Bassini was a direct, no-nonsense person. After refusing an academic chair in Parma because of irregularities, he was temporarily sent by Porta to practice in La Spezia Hospital. After becoming a professor the University of Padua, he dedicated himself enthusiastically to the study of inguinal and femoral hernias, changing the vision of the field from descriptive anatomy to clinical and surgical anatomy, and performing experimental cadaveric dissections and surgery.
On Christmas Eve 1884, he operated on and cured a patient suffering from inguinal hernia, a success he repeated during the next 2 years in a number of patients. In 1887, he wrote his Nuovo Metodo Operativo per la Cura Radicale dell’Ernia Inguinale, finally published in 1889. In this classic study, 262 cases of hernias (251 uncomplicated and 11 strangulated) were operated on with low mortality and few recurrences (5 of 251).
Fifty years after the first operation, his disciples, Fasiani and Catterina, wrote: “Half a century has gone by and Bassini’s method still remains as a definitive conquest that has survived all criticisms, all attempts at change and the daily verification repeated countless times all over the world.” Bassini’s greatness must not be limited to his inguinal hernia repair technique; he also proposed other important surgical techniques such as nephropexy, subtotal hysterectomy, ileocolostomy, the cravat incision of the neck for thyroid operations (usually called a Kocher incision), suprapubic cystostomy, hip disarticulation, intrascapular-thoracic amputation, and the technique for femoral hernia repair.
The etymology of the word hernia seems uncertain; its Greek root means protrusion. The Latin meaning more strongly suggests laceration, rupture, and giving way. Known since ancient medicine, its history represents the history of surgery and is characterized by practice, rationality, intuition, and ingenuity. Edoardo Bassini was one of the founding fathers of modern surgery and became famous after introducing a new technique for the treatment of inguinal hernia. This technique spread quickly and, in a short time, became the preferred treatment for that problem, enduring 150 years of leadership. Bassini should be credited for understanding the importance of the posterior wall of the inguinal canal and the need for restoring the physiologic mechanism associated with the obliquity of the inguinal canal and the misalignment of deep and superficial inguinal rings.
The author asserted: Hernia is a mechanical disease caused by an error of placing or of moving of the abdominal bowels; now, it is indispensable to restore the hernia to a condition in which it is able to regain its natural healthy state. The inguinal canal, as anyone can easily remember, acts physiologically by giving way to the spermatic cord and, at the same time, containing the bowels, due to its two walls and oblique position. It is constituted by two openings, an abdominal one and a subcutaneous one, and by two walls, a posterior one and an anterior one and between them the spermatic cord courses obliquely. Now, to obtain a radical cure, I deem necessary that the inguinal canal should be restored to its physiologic structure. The use of my technique satisfies and ensures both the mechanical condition and the function of the inguinal canal. To obtain a correct performance of the hernial repair, the cremaster muscle must be dissected, the transversalis fascia must be cut from the deep inguinal ring to the pubic tubercle, and the reconstruction of the inguinal canal must be performed by two planes: a deep one and a superficial one.
In the deep plane, a row of interrupted sutures must be placed at 1-cm intervals, beginning at the pubic tubercle and traversing to the deep inguinal ring. Medially, it includes the triple layer formed by the internal oblique muscle, the abdomen’s transverse muscle, and the transversalis fascia; laterally, it includes the iliopubic tract and the inguinal ligament. The sutures must not allow a too large or deep inguinal ring so as to avoid the risk of recurrence; on the other hand, it must not be too tight to avoid circulatory trouble caused by the pressure on the spermatic vessels. The spermatic cord is laid on this new wall, and the superficial plane is reconstructed using the external oblique aponeurosis.
“After trials on cadavers and with a good knowledge of anatomy and inguinal hernia, it was easy for me to devise the operative method, in a plain manner, without difficulties and in such a way as to satisfy and to allow healing without making use of hernia belt.”
His technique succeeded in decreasing the high percentage of recurrences at that time, from more than 30% to under 10%. At the beginning of the 1950s, Dr. Shouldice of Toronto and his co-workers suggested a modification of the original Bassini technique that mainly consists in the use of two separate, continuous sutures on the deep planes. The former encompasses fascia transversalis and iliopubic tract; the latter includes fascia transversalis, conjoint tendon, and inguinal ligament in such a way as to create a multiple layered suture of fascia transversalis. As admitted by the surgeons of the Shouldice Clinic, it may be described
as a variant of the Bassini technique, with modifications and innovations on the field of tissue-suturing, that trimmed down dramatically the percentage of recurrence to a slender 0.8% to 1%.
as a variant of the Bassini technique, with modifications and innovations on the field of tissue-suturing, that trimmed down dramatically the percentage of recurrence to a slender 0.8% to 1%.
In the past years, the unceasing evolution of surgical techniques, with the introduction of new treatments, has led to the gradual disuse of these methods of repair. Today, hernia surgery has been revolutionized by the techniques employing the use of prosthetic synthetic materials. These operations offer several advantages: easy learning curve, quick and simple performance, favorable postoperative course, and a recurrence rate under 0.2%.
Indications
The anterior approach without opening of fascia transversalis, proposed by Bassini, is still used in most of the tension-free techniques, especially in cases of primary hernias. Techniques such as those of Bassini and Shouldice that entail the use of sutures to close and reinforce the defect may be suggested in the event of intolerance of prosthetic material and in young patients (<20 y). In fact, we do not really know the long-term effects of prostheses.
Anesthesia
A good knowledge of pharmacology and toxicology of local anesthetics is mandatory for the surgeon to ensure a correct choice and a safe utilization. Local anesthetics inhibit depolarization of the nerve membrane, thus blocking the propagation of the action potential and, therefore, the transmission of sensations. Their efficacy is correlated to the type and concentration of the anesthetic and to the diameter of the nervous fibers. Type C fibers, which transmit pain and temperature sensations, small and unmyelinated, are the first to be blocked.
Bassini’s operation can be safely performed under local anesthesia because of several advantages over general, spinal, and epidural anesthetics, both during the operation and postoperatively. The postoperative course is usually very favorable, with low mortality, even in elderly and high-risk patients, and low morbidity with great reduction of deep venous thrombosis and pulmonary atelectasis. There is, actually, no reduction of pulmonary ventilation and the patient is able to ambulate soon after surgery because analgesia lasts long after the end of surgery.
Nausea, vomiting, oropharyngeal pains, urine retention, and headache, effects that are common after other types of anesthesia, do not occur after local anesthesia. The patient cooperates during surgery. He or she may be requested to increase abdominal pressure by coughing or contracting the abdominal and thoracic muscles, facilitating the search of parietal defect, and by allowing a stress test on the repair at the end of the operation.
The persistence of a normal muscular tone allows a correct appreciation of parietal tension and can sometimes suggest to the surgeon the performance of a relaxing incision on the rectal sheath. Local anesthesia requires accurate knowledge of regional anatomy, a meticulous dissection of surgical planes, and a careful attention to preventing unwanted trauma. These are the postulates of good surgery. Local anesthesia is not recommended in the patients younger than 12 to 13 years, nor in uncooperative patients or patients with serious mental illness. Obesity and large inguinal-scrotal hernias make local anesthesia technically more difficult and require a greater quantity of drugs. Nonetheless, these conditions do not absolutely preclude local anesthesia. Allergy to local anesthesia, actually very uncommon, obviously precludes the technique.
Surgical Technique
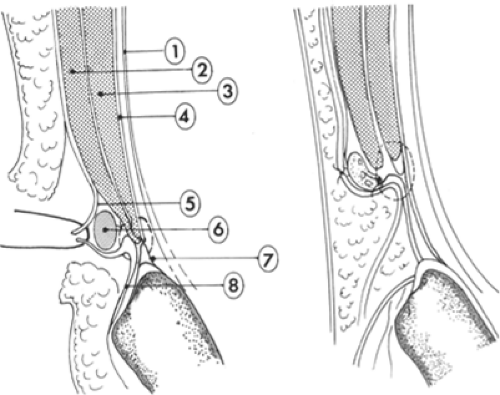
The repair is performed by suturing, superiorly, the triple layer, consisting of the internal oblique muscle, the transverse abdominal muscle, and the transversalis fascia (Fig. 1) and, below, the inguinal ligament and the iliopubic tract (Thomson ligament). The direct anterior approach to the inguinal region, historically the first, is still widely used, especially in the cases of primary hernias (Fig. 1), both for direct suturing and prosthetic techniques, and can be easily used under local anesthesia.
For an effective parietal reconstruction, careful knowledge and exposure of the anatomic structures is necessary. In this fashion, accidental lesions of the local nervous structures and of the funicular elements are avoided.
Incision of the Cutis and the Superficial Planes
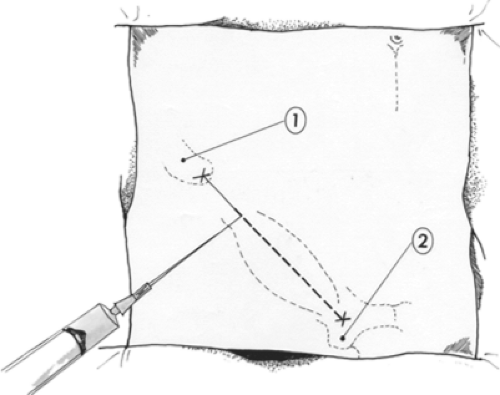
The points of reference are the anterior-superior iliac spine and the pubic tubercle, which lie lateral to the pubic symphysis; the line joining the two points parallels the inguinal ligament. If the procedure is performed under local anesthesia, first the skin and subcutaneous tissue are infiltrated along the incision line, starting from the subdermal layer, where the danger of damaging important vessels and of direct vascular injecting of the drug are minimal. A 25-gauge spinal needle is introduced subdermally and pushed slowly, while the anesthetic solution is injected. The anesthesia obtained in this way is nearly immediate.
The coetaneous incision starts at the pubic tubercle and continues 8 to 10 cm to the anterior-superior iliac spine along the inguinal ligament (Fig. 2). In the subcutaneous tissue, small arterial vessels are electrocoagulated. One should inject a small amount of local anesthetic nearby because of the
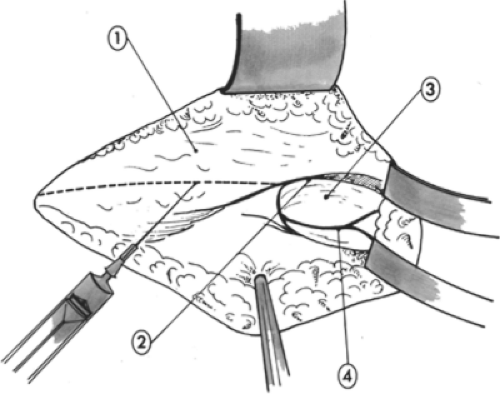
presence of neighboring small and sensitive nerves (Fig. 3). Then the deep subcutaneous tissue is injected with a shorter, 21-guage needle. It is wise to aspirate before injecting because the superficial epigastric vessels are easily found at this level. At this stage, 10 to 12 mm of 0.75% ropivacaine or 2% mepivacaine are usually sufficient.
presence of neighboring small and sensitive nerves (Fig. 3). Then the deep subcutaneous tissue is injected with a shorter, 21-guage needle. It is wise to aspirate before injecting because the superficial epigastric vessels are easily found at this level. At this stage, 10 to 12 mm of 0.75% ropivacaine or 2% mepivacaine are usually sufficient.
One must also ligate and divide the superficial epigastric veins (collateral affluents of the greater saphenous vein). The superficial Scarpa fascia is cut short in the upper part of the incision to expose the external oblique aponeurosis. Then 8 to 10 mm of local anesthetic is injected under the aponeurosis to initiate the block of the regional sensitive nerves, thus reducing the pain caused by the division of the medial subcutaneous tissue.
The external oblique fascia is completely exposed and separated from the innominate fascia, which connects to the external spermatic fascia, made of loose cellular tissue that connects to the external spermatic fascia. The superficial inguinal ring is freed. The dissection of the inguinal canal is eased by the infiltration of the anesthetic solution, which separates the aponeurosis from the underlying elements.
Using the scissors, the cribriform femoral fascia is dissected, freeing the inferior surface of the inguinal ligament. This surgical maneuver, done after infiltrating a few milliliters of anesthetic solution, starts medially, near the pubic tubercle, and goes laterally to the femoral vein, the position of which can be easily noted by the pulsation of the adjacent femoral artery.
This maneuver permits not only better mobilization of the inguinal ligament, but also the exploration with a finger for a possible associated femoral hernia.
Incision of the External Oblique Aponeurosis
The aponeurosis is incised along the course of its fibers starting from the upper side of the superficial inguinal ring and exceeding the deep inguinal ring. The superior side of the external oblique aponeurosis is separated by blunt dissection from the internal oblique muscle. The inferior side is detached from the spermatic cord in male patients or the round ligament in female patients.
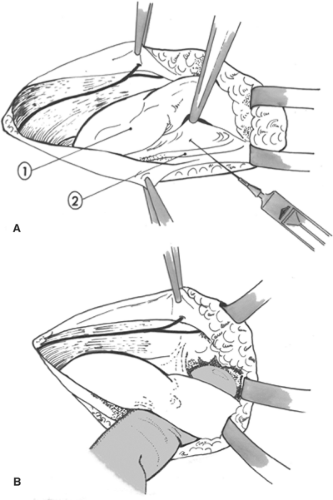
During this maneuver, two important nerves of the inguinal region, the iliohypogastric and the ilioinguinal, are located. The iliohypogastric nerve runs on the internal oblique muscle, parallel and superior to the spermatic cord, leaving the inguinal canal through a small opening that is medially located superior to the superficial inguinal ring. The ilioinguinal nerve runs among the fibers of the cremaster muscle on the anterior-lateral side of the spermatic cord. Both are sensitive nerves and must be identified to be blocked selectively with anesthesia (Fig. 4) and to prevent accidental injury or entrapment while performing the repair. Their injury may cause undue postoperative pain; and the selective blocking by a few milliliters of anesthetic solution injected close to the nerves usually grants an effective and long-lasting analgesia.
Isolation of the Spermatic Cord
The spermatic cord is isolated from the posterior wall of the inguinal canal. Before mobilizing the spermatic cord, it is necessary to infiltrate the inguinal ligament and the posterior wall of the inguinal canal near the pubic tubercle to make this maneuver less painful (Fig. 5A). The isolation starts at the pubic tubercle by sliding a finger along the groove formed by the inguinal ligament from the upper side to the lower.
After having been completely freed, the spermatic cord is loaded with a string and pulled forward so that it is easily possible to detach the cord from the posterior wall consisting of the transversalis fascia (Fig. 5B).
Finally, the spermatic cord is completely freed from the deep inguinal ring to the pubic tubercle. Now the internal oblique muscle is visible above superiorly, the transversalis fascia is visible deeply, and the inguinal ligament lies below.
Finally, the spermatic cord is completely freed from the deep inguinal ring to the pubic tubercle. Now the internal oblique muscle is visible above superiorly, the transversalis fascia is visible deeply, and the inguinal ligament lies below.
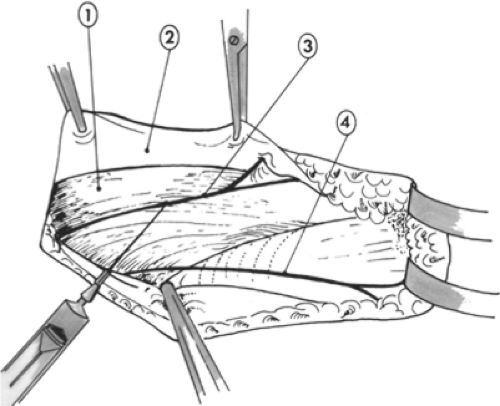 Fig. 4. Selective blocking of the ilioinguinal and iliohypogastric nerves. 1, Internal oblique muscle; 2, external oblique aponeurosis; 3, iliohypogastric nerve; 4, ilioinguinal nerve. |
Resection of the Cremaster Muscle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree