David Mee-Lee, MD, and Gerald D. Shulman, MA, MAC, FACATA
27
The ASAM Criteria—Treatment Criteria for Addictive, Substance-Related, and Co- Occurring Conditions was designed to help clinicians, payers, and regulators use and fund levels of care in a rational and individualized treatment manner. This involves moving the addiction treatment field away from fixed length of stay programs to an assessment-based, clinically driven, outcomes-oriented continuum of care. The ASAM Criteria represent a shift from:
1. One-dimensional to multidimensional assessment—from treatment based on diagnosis to treatment that is holistic addressing multiple needs
2. Program-driven to clinically and outcomes-driven treatment—from placement in a program often with fixed lengths of stay to person-centered, individualized treatment responsive to specific needs and progress and outcome in treatment
3. Fixed length of service to variable length of service, based on patient needs and outcomes
4. A limited number of discrete levels of care to a broad and flexible continuum of care
SELECTING APPROPRIATE SERVICES
In individualized, assessment-driven treatment, service priorities are identified in the context of the patient’s severity of illness and level of function. No single treatment or level of care matches for all individuals at all times.
The Concept of “Unbundling”
At present, most addiction treatment services are “bundled,” meaning that a number of different services are packaged together and paid for as a unit. Unbundling is a practice that allows any type of clinical service (such as psychiatric consultation) to be delivered in any setting (such as a residential program). The unbundling concept thus is designed to maximize individualized care, to reduce costs, and to encourage the delivery of necessary treatment in any clinically feasible setting.
A transition to unbundled treatment would require systems change in state program licensure and reimbursement. In terms of treatment, there would no longer be “programs” but rather a constellation of services to meet the needs of each patient. The systems currently in use for program licensure or accreditation, billing, reimbursement, and funding would not support unbundled treatment. However, the ASAM Criteria encourage exploration of unbundling by suggesting ways to match risk and severity of needs with specific services and intensity of services.
UNDERSTANDING THE ASAM CRITERIA
Four features characterize the ASAM Criteria: (1) comprehensive, individualized treatment planning, (2) ready access to services, (3) attention to multiple treatment needs, and (4) ongoing reassessment and modification of the plan.
Functionally, the criteria are used to match services, interventions, and treatment settings to each individual’s particular problems and treatment needs as well as his or her strengths, skills, and resources. By expanding the criteria to incorporate more use of outpatient care, especially for those in early stages of readiness to change; expanding to five levels of withdrawal management; and encouraging flexible lengths of stay, the ASAM Criteria are designed to assist in reducing waiting lists for residential treatment and thus improve access to care.
To be effective, treatment must address any associated medical, psychological, social, vocational, legal, and recovery environment problems. Through its six assessment dimensions, the ASAM Criteria underscore the importance of multidimensional assessment and treatment.
Principles Guiding the Criteria
Several important principles have guided development of the ASAM Criteria.
Goals of Treatment
The goals of intervention and treatment determine the methods, intensity, frequency, and types of services provided. The health care professional’s decision to prescribe a type of service, and subsequent discharge of a patient from a level of care, are based on how that treatment and its duration will help resolve dysfunction and positively alter the prognosis for the patient’s long-term outcome. Thus, in addiction treatment, the treatment may extend beyond simple resolution of observable signs and symptoms to the achievement of overall healthier functioning, the difference between abstinence alone and recovery.
Individualized Treatment Plan
Treatment should be tailored to the needs of the individual and guided by an individualized treatment plan that is developed in collaboration with the patient. Such a plan should be based on the patient’s goals for treatment and a comprehensive biopsychosocial assessment of the patient and, when possible, a comprehensive evaluation of the family as well. As with other disease processes, length of service should be linked directly to the patient’s response to treatment rather than a predetermined time frame based on the length of the treatment program or available reimbursement.
Choice of Treatment Levels
The preferred level of care is the least intensive level that meets treatment objectives, while providing safety and security for the patient. Moreover, while the levels of care are presented as discrete levels, in reality they represent benchmarks or points along a continuum of treatment services that could be used in a variety of ways, depending on a patient’s needs and response. For patients who have been previously treated and have relapsed, the choice of the current level of care should be based on an assessment of the patient’s history and current functioning, not automatic placement in a more intensive level of care.
Continuum of Care
To provide the most clinically appropriate and cost-effective treatment system, a continuum of care must be available, offered by a single provider or multiple providers. For the continuum to work most effectively, it is best distinguished by three characteristics: (1) seamless transfer between levels of care, (2) philosophical congruence among the various providers of care, and (3) timely arrival of the patient’s clinical record at the next provider.
Progress Through the Levels of Care
As a patient moves through treatment in any level of care, his or her progress in all six dimensions should be continually assessed. Such multidimensional assessment ensures comprehensive treatment. The appearance of new problems may require services that can be effectively provided at the same level of care or that require a more or less intensive level of care.
Length of Stay
The length of stay or service is determined by the patient’s progress toward achieving his or her treatment plan goals and objectives. Fixed length of stay or program-driven treatment is not individualized and does not respond to the particular problems of a given patient.
Clinical Versus Reimbursement Considerations
The ASAM Criteria are not intended as a reimbursement guideline, but rather as a clinical guideline for making the most appropriate placement recommendation for an individual patient with a specific set of symptoms and behaviors.
Treatment Failure
Two incorrect assumptions are associated with the concept of “treatment failure.” The first is that the disorder is acute rather than chronic, so that the only criterion for success is total and complete cure and elimination of the problem. The second assumption is that responsibility for treatment “failure” always rests with the patient. However, poor treatment outcomes also may be related to a provider’s failure to provide services tailored to the patient’s needs. Some benefit managers require that a patient “fail” at one level of care as a prerequisite for approving admission to a more intensive level of care. In fact, such a requirement is no more rational than treating every patient in an inpatient program or using a fixed length of stay for all.
Should a patient drink or use drugs during treatment, the immediate response should be to revise the treatment plan rather than automatically change the level of care or administratively discharge the patient. Additionally, some benefit managers require that a patient be “motivated for sobriety” as a requirement for admission to a program. Given the characteristic signs of ambivalence and lack of readiness to change of addiction disorders, the only requirement should be that the patient is willing to enter treatment. Clinicians then facilitate the patient’s self-change process along the stages of change.
ASSESSMENT DIMENSIONS
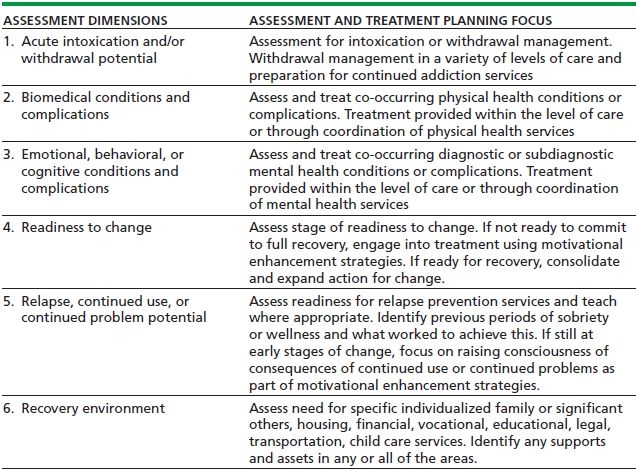
The ASAM Criteria contain descriptions of treatment programs at each level of care, including the setting, staffing, support systems, therapies, assessments, documentation, and treatment plan reviews typically found at that level. The criteria identify six assessment areas (dimensions) as the most important in formulating an individualized treatment plan and in making subsequent patient placement decisions. Table 27-1 outlines the six dimensions and the assessment and treatment planning focus of each dimension.
TABLE 27-1. ASAM CRITERIA ASSESSMENT DIMENSIONS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


