12 The acute abdomen and intestinal obstruction
Aetiology
The causes of the acute abdomen may be subdivided into surgical, medical and gynaecological disorders. Surgical causes may be classified according to the organ involved, as well as the underlying pathological process (Table 12.1). The most common causes in any population will vary according to age, sex and race, as well as genetic and environmental factors (Tables 12.2 & 12.3).
Table 12.1 Possible causes of acute abdominal pain
| Surgical Inflammation |
| Obstruction |
| Ischaemia |
| Perforation |
| Medical Cardiovascular |
| Gastrointestinal |
| Abdominal wall conditions |
| Genitourinary |
| Neurological |
| Haematological |
| Endocrine |
| Metabolic |
| Infective |
| Gynaecological |
Table 12.2 Common causes of acute abdominal pain in UK adults requiring admission to hospital
| Condition | Approximate incidence (%) |
|---|---|
| Non-specific abdominal pain | 35 |
| Acute appendicitis | 30 |
| Acute cholecystitis and biliary colic | 10 |
| Peptic ulcer disease | 5 |
| Small bowel obstruction | 5 |
| Gynaecological disorders | 5 |
| Acute pancreatitis | 2 |
| Renal and ureteric colic | 2 |
| Malignant disease | 2 |
| Acute diverticulitis | 2 |
| Dyspepsia | 1 |
| Miscellaneous | 1 |
Table 12.3 Common causes of acute abdominal pain in UK children
Pathophysiology of abdominal pain
Somatic pain
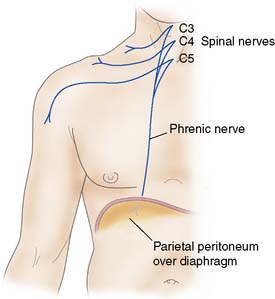
When the diaphragmatic portion of the parietal peritoneum is irritated peripherally, there will be pain, tenderness and rigidity in the distribution of the lower spinal nerves, but when it is irritated centrally, pain is referred to the cutaneous distribution of C3, 4 and 5 (i.e. the shoulder area, Fig. 12.1). Somatic pain is classically described as sharp or knife-like in nature, and is usually well localized to the affected area.
Visceral pain
Summary Box 12.1 Abdominal pain
• Visceral abdominal pain is mediated by the sympathetic nervous system and is typically deep-seated and ill localized to the area originally occupied by the viscus during intrauterine life
• Colic is a form of visceral pain that arises from a hollow viscus with muscle in its walls (e.g. gut, gallbladder, ureter), and results from excessive muscle contraction, often against an obstructing agent
• Patients experiencing colic are usually unable to remain still during the bout of pain but are pain-free between attacks. ‘Biliary colic’ is an exception (and the term colic may be a misnomer), in that pain often waxes and wanes on a plateau and there are no pain-free intervals
• Parietal pain, such as that caused by parietal peritonitis, is mediated by somatic nerves and is localized to the area of inflammation
• Reflex guarding and rigidity of the overlying muscles is usually present, and the patient is reluctant to move for fear of exacerbating the pain
• Some areas of the peritoneum (e.g. the pelvis, posterior abdominal wall) are ‘non-demonstrative’ in that parietal peritonitis may be present without tenderness or guarding of overlying muscles.
Pathogenesis
As one can see from the list of surgical conditions that may present with acute abdominal pain (Table 12.1), there are two main underlying pathological processes involved: inflammation and obstruction. These processes may be triggered by a variety of underlying abnormalities. It is important to realize that in any one patient a combination of abnormalities and processes may be involved.
Inflammation
Acute inflammation of an intra-abdominal organ or the peritoneum may occur as a result of a variety of irritants. These may be broadly classified into infective or non-infective in nature (Table 12.4).
Table 12.4 Injurious agents causing inflammation
| Infective |
| Non-infective |
Peritonitis
Inflammation of the peritoneum (peritonitis) may be classified according to extent (either localized or generalized) and aetiology (Table 12.5). In a surgical setting, the most common cause of generalized peritonitis is perforation of an intra-abdominal viscus. Inflammation of the peritoneum results in an increase in its blood supply and local oedema formation. There is transudation of fluid into the peritoneal cavity, followed by the accumulation of a protein-rich fibrinous exudate. In the normal state, the greater omentum constantly alters its position within the abdominal cavity as a result of intestinal peristalsis and abdominal muscle contraction. In the presence of inflammation, the greater omentum will adhere to and surround the abnormal organ. The fibrinous exudate effectively glues the omentum to the inflamed viscus, walling it off and preventing the further spread of inflammation. In addition, the exudate inhibits intestinal peristalsis, resulting in a paralytic ileus which also limits the spread of the inflammation and infection. As a result of the ileus, fluid accumulates within the lumen of the intestine and, along with the formation of large volumes of intra-peritoneal transudate and exudate, this will lead to a decrease in the intravascular volume, producing the clinical features of hypovolaemia.
Table 12.5 Classification of peritonitis
| Generalized peritonitis |
|---|
| Primary: infection of the peritoneal fluid without intra-abdominal disease |
| Secondary: inflammation of the peritoneum arising from an intra-abdominal source |
| Localized peritonitis |
|---|
Infarction
An infarct is an area of ischaemic necrosis caused either by an occlusion of the arterial supply or the venous drainage in a particular tissue, or by a generalized hypoperfusion in the context of shock (Table 12.6). The typical histological feature of infarction is ischaemic coagulative necrosis. An inflammatory response begins to develop along the margins of an infarct within a few hours, stimulated by the presence of the necrotic tissue.
Table 12.6 Aetiology of infarction
| Occlusive |
| Arterial |
| Venous |
| Non-occlusive |
| Shock |
| Vasoconstrictor drugs |
Perforation
Spontaneous perforation of an intra-abdominal viscus may be the result of a range of pathological processes. Weakening of the wall of the viscus, which might follow degeneration, inflammation, infection or ischaemia, will predispose to perforation. An increase in the intraluminal pressure of a viscus, such as occurs in a closed-loop obstruction (Fig. 12.2), will predispose to perforation, as will peptic ulceration, acute appendicitis and acute diverticulitis. Other less common causes are carcinoma of the colon, inflammatory bowel disease and acute cholecystitis.
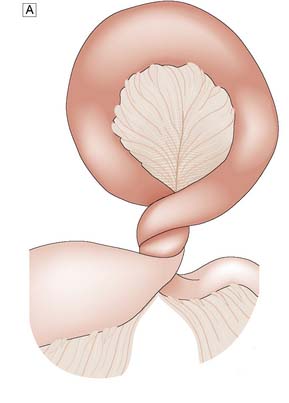

Fig. 12.2 Volvulus: an example of closed-loop obstruction.
A Diagrammatic representation of a volvulus. B X-ray showing volvulus of sigmoid colon.
Clinical assessment
History
The main presenting complaint of patients with an acute abdomen is pain. The characteristics of the pain (Table 12.7) give important clues to the likely underlying diagnosis, and these should be explored in depth. However, the importance of a full history cannot be overemphasized and is essential in all patients.
Table 12.7 Characteristics of abdominal pain
Site of pain
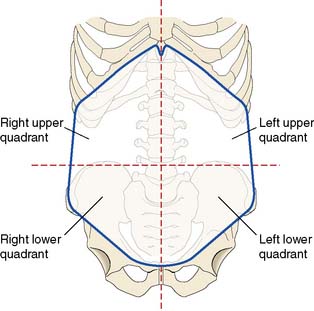
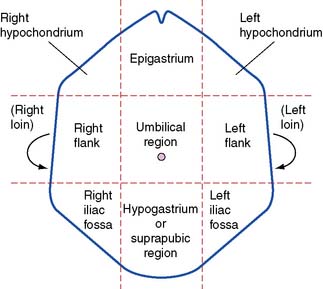
The site of abdominal pain is perhaps the most valuable pointer to the underlying diagnosis. In order to describe the site of pain, the abdomen is traditionally divided into either quarters or ninths (Figs 12.3 and 12.4).
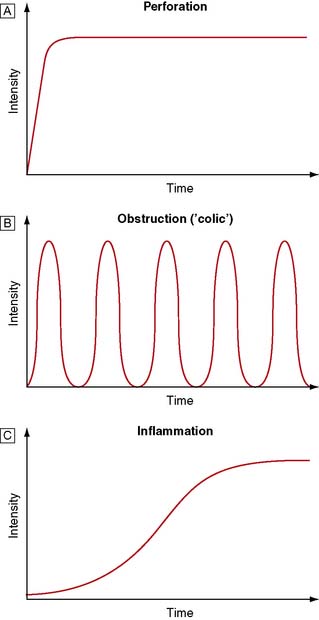
Onset of pain
The onset of pain can be sudden or gradual. Typically, pain from a perforation is sudden and that from inflammation is gradual. Patients with the former can usually remember exactly what they were doing at the time of onset, whereas in the latter localization in time is more difficult. The various characteristics of abdominal pain, as shown in Figure 12.5, are essential in helping the clinician formulate a differential diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree