The Abdominal Hysterectomy
William N. Spellacy
Mitchel S. Hoffman
Evelyn G. Serrano
Introduction
The hysterectomy operation is the second most common surgical procedure performed in the United States, with cesarean section being the most common. About 25% of hysterectomies are vaginal and the remainder abdominal operations. A small percentage of hysterectomies involve the use of laparoscopic techniques. It has been estimated that in the United States about 600,000 hysterectomies are performed annually at a cost of about $3 billion to $5 billion. Approximately one third of women 65 years of age have had a hysterectomy. The number of operations varies by year, geographic location, age, and race. The peak year for procedures was 1975, with more than 700,000 operations being done. The rate decreased in the 1980s as many new medical therapies became available to gynecologists. The highest rates are in the South and the lowest rates in the Northeast. This rate difference is 2.5-fold. The highest rate occurs in the perimenopausal age group of 40 to 50 years.
About 85% of hysterectomies are performed in the treatment of myoma, endometriosis, endometrial hyperplasia, cancer, or prolapse. Prolapse is usually corrected by vaginal hysterectomy, whereas most of the others are treated abdominally. Of the above indications, uterine myomas are the most frequent. Because myomas are more common in African-American women, they have a higher incidence of having an abdominal hysterectomy. Symptoms usually reported by women with these diseases are abnormal bleeding, chronic pelvic pain, abdominal mass, abnormal Papanicolaou (Pap) test, or pressure in the vagina. The frequency of hysterectomy is significantly higher in women who have been previously sterilized. This may represent the fact that they readily accept surgical therapy for their problems, including family planning. Except for cancer, surgery should not generally be the first approach to therapy. Effective medical therapy exists for many of the benign diseases like myomas, endometriosis, and endometrial hyperplasia. Examples of these medical therapeutic agents are gonadotropin-releasing hormone agonists to establish early reversible medical castration for myomas and endometriosis, antiprogestins (RU486) for myomas, androgens (danazol) for endometriosis, and progestins for endometrial hyperplasia. Less extensive surgery is also available for these conditions like myomectomy, laparoscopic laser coagulation for endometriosis, dilation curettage for endometrial hyperplasia, endometrial ablation or progestin-type intrauterine devices for menorrhagia, and pelvic artery embolization for myomas. In general, the original complaint may be corrected by performing a hysterectomy, but on long-term follow-up, new problems can develop as a result of castration, such as weight gain, decreased libido, adhesions, and hot flashes.
Procedure
Shaving the abdominal skin before surgery is usually unnecessary. A Foley catheter must be inserted into the bladder before surgery and attached to straight drainage. This reduces the size of the bladder and prevents incidental bladder damage when entering the lower abdomen and when taking the bladder off the lower uterine segment and cervix. Entry into the abdomen is usually by either a lower abdominal midline incision or by a transverse Pfannenstiel incision. It is important to incise the fascial layer down to the symphysis pubis if midline incision is used, as the lower portion of the incision is critical for adequate visualization of the cervix and vagina. The Pfannenstiel incision provides a more limited exposure and is contraindicated if there is a very large uterine mass or a bleeding tendency, or if inspection or surgery may be necessary in the upper abdomen. The advantage of the Pfannenstiel incision above the cosmetic absence of a visible scar is that it is less painful for the patient postoperatively and therefore allows earlier ambulation and recovery. There is no difference in dehiscence rates with a vertical or transverse incision.
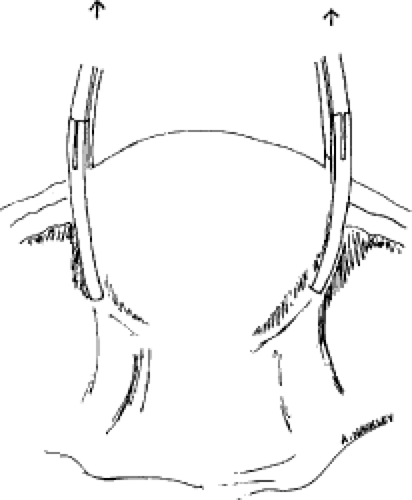
Once the abdomen has been entered, inspection and palpation takes place. Assuming all the pathology is found to be limited to the uterus, then the bowel is packed out of the pelvis into the upper abdomen using moist packs to prevent serosal injury. Adhesions, if present, may need to be lysed either bluntly or sharply with scissors. A self-retaining retractor can then be fixed in place, giving good visualization of the pelvic structures. The uterus can be grasped and held with long clamps (e.g., Kocher) placed along the ovarian round ligaments at their uterine insertion (Fig. 1).
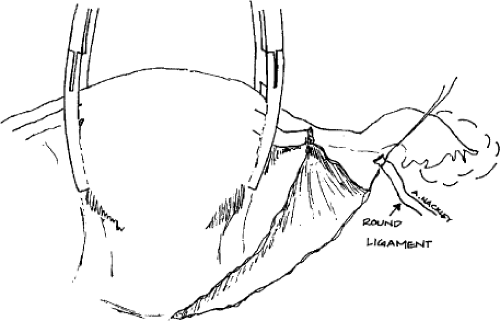 Fig. 2. The round ligaments are clamped, cut, and sutured bilaterally as the first step and initial incisions. This opens the retroperitoneal space. |
The initial uterine incisions on each slide should begin at the round ligaments. These are clamped, elevated, sutured, and then cut (Fig. 2). The external iliac vessels are in close proximity. Division of the round ligament lateral to the utero-ovarian vascular anastomosis avoids hemorrhage and facilitates isolation of the upper vascular pedicle. One small artery (Sampson artery) runs under this ligament and should be included in the suture. Back bleeding is prevented by the uterine-holding clamps. The pelvic peritoneum can then be opened laterally ahead and behind the round ligament. This peritoneal incision is carried from each side completely across the front of the uterus at the vesicle uterine fold
(Fig. 3A,B). This allows the bladder to then be bluntly pushed in the midline inferiorly off the cervix. If there are any adherent areas, they must be sharply dissected in order to prevent bladder injury. This is commonly a problem in women who have previously had low segment transverse cesarean sections. If bladder damage is suspected at any time during the operation, the bladder should be filled with a sterile colored solution, which will quickly identify a cystotomy. One easily obtained solution that will not permanently stain the tissues is sterile nursery formula. Dyes like methylene blue can also be used, but if there is a cystotomy, the spilled dye will attach to the pelvic tissues and they will remain stained during the remainder of the operation.
(Fig. 3A,B). This allows the bladder to then be bluntly pushed in the midline inferiorly off the cervix. If there are any adherent areas, they must be sharply dissected in order to prevent bladder injury. This is commonly a problem in women who have previously had low segment transverse cesarean sections. If bladder damage is suspected at any time during the operation, the bladder should be filled with a sterile colored solution, which will quickly identify a cystotomy. One easily obtained solution that will not permanently stain the tissues is sterile nursery formula. Dyes like methylene blue can also be used, but if there is a cystotomy, the spilled dye will attach to the pelvic tissues and they will remain stained during the remainder of the operation.
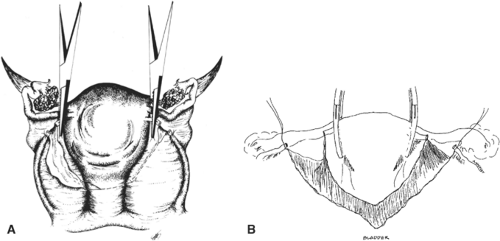 Fig. 3. The vesicouterine peritoneum is incised (A), and the bladder is pushed away from the cervix (B). |
The surgeon can then bluntly dissect the retroperitoneal space posterior to the round ligament. This will allow visualization of the iliac vessels on the lateral pelvic wall and the ureter on the medial peritoneal fold. A decision about retaining or removing the ovaries should be discussed with the patient prior to surgery. In general, if the ovaries are normal and the woman is 50 years of age or older, it is recommended that they be removed. Removal of ovaries in younger women will reduce their estrogen and androgen hormone levels and is not routinely done unless there is obvious gross ovarian pathology, a strong family history of ovarian cancer, or a disease process where ovarian hormones either aggravate the disease or may in fact harbor the disease, such as with endometriosis or chronic pelvic infection.
If the ovaries are to be removed, then the infundibulopelvic ligaments need to be identified bilaterally, doubly clamped with instruments like the Heaney clamps, cut, and ligated (Fig. 4). Because there are many large vessels in these ligaments, they are first ligated with a free tie, and then a suture ligature is placed distal to that first tie for permanent closure. This prevents the formation of a hematoma if the needle should penetrate a vessel. If the ovaries are to be preserved, the uteroovarian ligaments are clamped, cut, and ligated in a similar manner (Fig. 5). These ligaments should be clamped as close to the uterus as possible to reduce ovarian blood flow disruption and ovarian hypofunction.
The broad ligament support of the uterus is then excised from the top of the uterus in a series of clamps onto the cardinal and then vaginal mesentroid ligaments below the cervix (Fig. 6). The number of clampings needed will depend on the uterine size and cervical length. Because the ureter passes approximately 1.5 cm lateral to the uterus and under the uterine artery, it is important to keep the clamp applied close to the uterus. When clamping tissue in curved areas of the uterus the Heaney clamp is useful, whereas when clamping in straight areas as along the cervix a straight Ballantine clamp is helpful. Clamping occurs in sequence down the broad ligament to the upper vaginal cuff area. After each clamp the tissue is cut and then ligated with a transfixation ligature. Each suture is cut after it is tied. In general, absorbable (Vicryl, chromic) 0 or 1 suture is used.
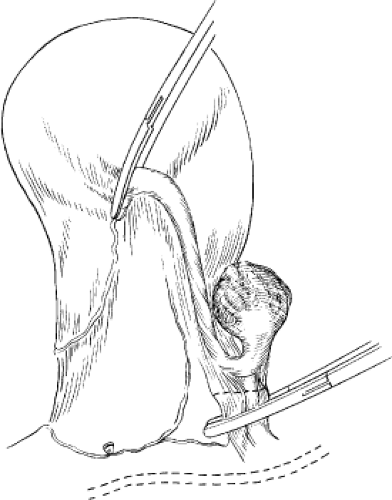 Fig. 4. The infundibulopelvic ligaments are identified, clamped, cut, and sutured if the ovaries are to be removed. Care is taken to avoid the ureter. |
The hysterectomy can be done with complete removal of the cervix, which is the usual procedure (Fig. 7), or the cervix can be left in place in a subtotal hysterectomy (Fig. 8A,B). If the latter procedure is selected, cervical disease should have been excluded with a normal preoperative pelvic examination and Pap test. Retaining the cervix may be elected in some patients based on the theory that the cervix is important for orgasm or pelvic wall support. If there is difficulty in dissecting off the bladder or if the patient develops significant intraoperative problems like cardiac arrhythmias, the surgeon may decide to shorten the operative time and leave the cervix. In some cases of advanced ovarian cancer the cervix is retained to prevent cancer growth into the vagina. When the cervix is left, the endocervical canal should be excised or cauterized to prevent later bleeding from retained endometrium.
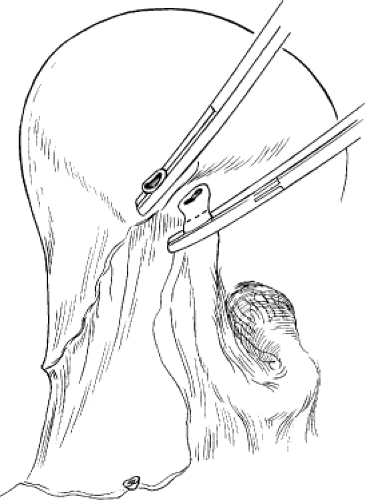 Fig. 5. The utero-ovarian ligaments are clamped, cut, and sutured when the ovaries are to be preserved. |
When the cervix is to be removed with the uterus, the end of the cervix can be palpated and a bulge can usually be seen at this area of the vaginal apex. Heaney clamps can be placed across the vaginal cuff and when the tissue is cut, it will be clear that the vagina has been entered. Using a scissor like the Jorgenson type allows the vaginal apical cuff to be totally cut across. Inspection of the uterus will determine if the entire cervix is in the operative specimen. The vaginal cuff can then be grasped with clamps (e.g., Kocher) including both the vaginal mucosa and fascia. The cut edge will have small bleeders, but the main arterial systems are at 3 and 9 o’clock as ascending branches of the pudendal artery. The cuff can be closed with running stitches (Fig. 9A,B) or it can be left open. In the latter case the lateral angles can be sutured with a Ball-type stitch to obstruct those ascending arteries and secure the vagina to the cardinal ligaments. The cut edge can then be made hemostatic with a running locking suture (Fig. 10A,B). If the vaginal cuff is left open, the peritoneum should be used to cover the opening to prevent bowel herniation into the vagina. Less granulation tissue is present in the vagina postoperatively if Vicryl suture is used on the cuff. An advantage of leaving the cuff open is that pelvic drains can be placed if there has been infection or excessive bleeding, and pelvic collections of fluid postoperatively can be easily drained if they occur. Oncology follow-up may also be facilitated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree