FIGURE 39-1 The 64-pole Constellation basket mapping catheter is shown. It consists of eight splies, and each spline has eight electrodes.
FIGURE 39-2 The 64-pole Constellation basket mapping catheter deployed in the right atrium. An implantable loop recorder, 20-pole steerable catheter, and circular mapping catheter are also seen in the fluoroscopic image.
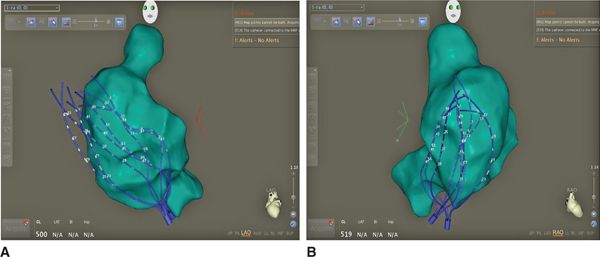
FIGURE 39-3 (A) An LAO image of a 3-dimensional shell of the right atrium derived from an intracardiac roving mapping catheter with the 64-pole basket catheter overlaid. The basket catheter clearly lies outside the shell of the atrium revealing a lack of complete reconstruction of the atrium with the roving catheter. (B) An RAO image of a 3-dimensional shell of the right atrium derived from an intracardiac roving mapping catheter with the 64-pole basket catheter overlaid.
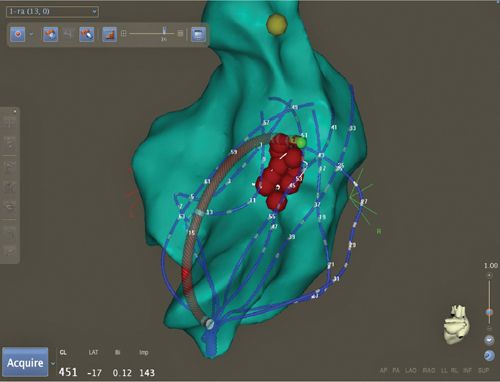
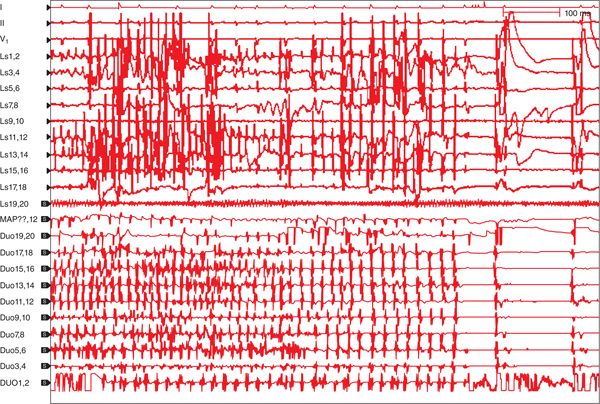
In each atria, after basket insertion and careful positioning, meticulous computer-based AF signal analysis was performed using specialized software (Topera, San Diego, CA, United States). After localizing these rotors in relation to the basket electrodes, radiofrequency (RF) ablation of these sites was applied in both atria (Figures 39-4 to 39-7). After matching the signal location in relation to the basket electrodes and confirming the signals with repeat recordings, several RF applications were applied to the site, which resulted in slowing and organization of the AF (see Figure 39-6). In the LA there was another rotor signal recorded on the posterior wall. Applying several RF applications resulted in acute termination of the AF to normal sinus rhythm (see Figure 39-7). The rotor ablation was complemented by conventional pulmonary vein isolation. On follow-up after 3 months, the patient was free of symptoms, and loop recorder interrogation showed no evidence of AF.
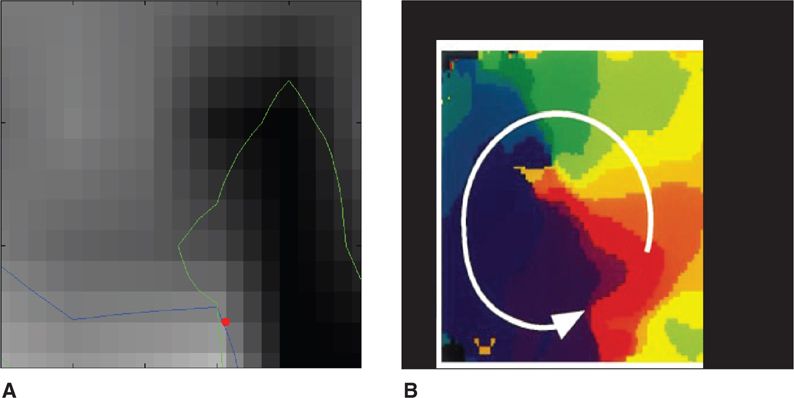
FIGURE 39-4 (A) The image is a still frame of a movie depicting the rotation of the rotor around the central core depicted by the red spot. This movie was created from the electrograms recorded from the basket electrode during AF. The signals are then processed to identify a rotor. (B) The right image is a map of the wavefront of activation of the rotor around its core.
FIGURE 39-5 This is an electroanatomic map displaying the 64-pole basket catheter deployed in the left atrium. The green shell represents the left atrium anatomy. The sites of delivery of RF current are marked by the red dots and are delivered at the region of rotor activation. The ablation catheter tip is highlighted in green.
FIGURE 39-6 More rapid atrial fibrillation cycle length (on left side of electrogram tracing) slows (longer cycle length and more organized AF tracing on right side of electrogram tracing) during RF ablation of a left atrial rotor.
FIGURE 39-7 Termination of atrial fibrillation during application of radiofrequency energy at a rotor site identified by processing of AF electrograms recorded from the 64-basket electrode.
EPIDEMIOLOGY AND PATHOPHYSIOLOGY
AF is the most common human arrhythmia and is characterized by chaotic contraction of the atrium. Mechanisms of AF can be divided into the mechanisms of initiation and mechanisms of perpetuation of arrhythmia. There are three widely held theories on the mechanisms of AF perpetuation: multiple random propagating wavelets, focal electrical discharges, and localized reentrant activity with fibrillatory conduction.
Multiple Wavelet Hypothesis
In 1959, Moe and Abildskov proposed the multiple wavelet hypothesis.1,2 This theory was experimentally confirmed in 1985 by the work of Allessie and colleagues.3 According to this hypothesis, AF results from the presence of multiple independent wavelets occurring simultaneously and propagating randomly throughout the LA and RA. This model suggests that the number of wavelets at any point in time depends on the atrial conduction velocity, refractory period, and excitable mass. The perpetuation of AF appears to require at least four to six coexisting wavelets and is favored by slowed conduction, shortened refractory periods, and increased atrial mass. One of the practical implications of this hypothesis was the fact that chronic AF could be cured in some patients by the placement of multiple surgical lesions (maze procedure) to compartmentalize the atria into regions presumably unable to sustain multiple wavelet reentry.5
Despite the fact that this theory was widely accepted, this hypothesis failed to answer many questions, such as why AF exhibits consistent spatial nonuniformities in rate and activation vectors, how ablation may terminate AF relatively early, in some cases before compartmentalization of meandering wavelets, or why extensive ablation often has little acute impact.6–8
Focal Triggers
In clinical practice, the concept of focal triggers as a cause of AF was verified to the greatest extent by Haissaguerre and colleagues who found that ectopic beats from the pulmonary veins initiated AF and that a localized catheter ablation procedure to eliminate these triggers could cure AF in some patients.9–11 This important finding made the pulmonary veins and the posterior wall of the LA the primary targets to cure AF.
Mother Rotors
Based on animal models, some authors have proposed that in the presence of an appropriately heterogeneous AF substrate a focal trigger can result in sustained high-frequency reentrant AF drivers (rotors).12–
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree