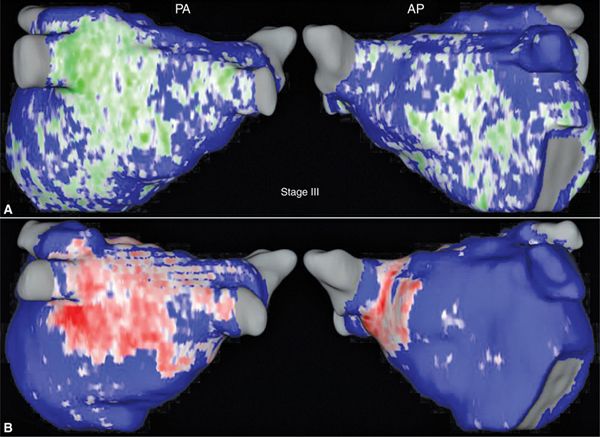
FIGURE 40-1 Three-dimensional LA reconstruction showing LASRM (A) and chronic LA Scar (B) after PVAI. (A) LASRM estimated at 12% (stage II). (B) LGE-MRI was obtained 10 months post-AF ablation, exhibiting 12.5% LA scar. Blue, healthy myocardium; green, LASRM; red, scarred tissue. Dark green/red indicates transmurality; white indicates nontransmurality. Wall contours are smoothened.
CASE 2
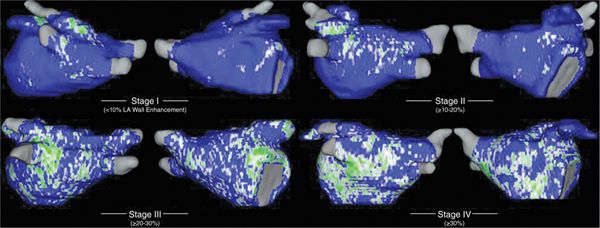
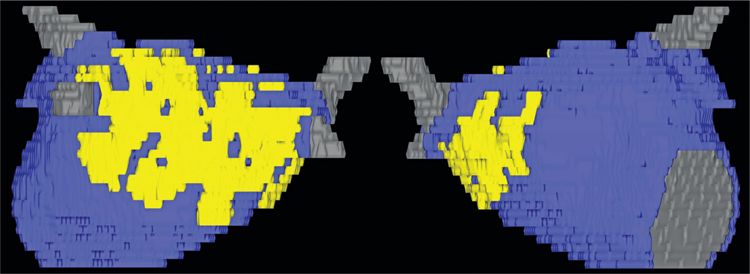
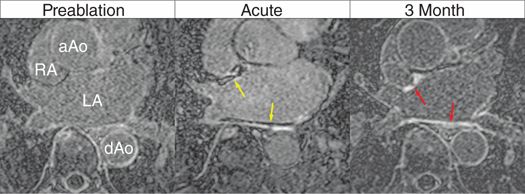
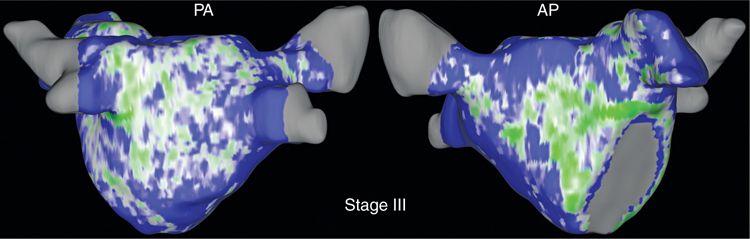
A 68-year-old man presents who was first diagnosed with paroxysmal AF at the age of 52. Initially, episodes lasted 2 to 3 days and were associated with palpitations. Over the following 15 years, the frequency, duration, and severity of symptoms of AF episodes increased, some lasting for weeks. While initially he only felt palpitations, with time he increasingly had shortness of breath, with a sensation of not getting enough oxygen, and lightheadedness. He always, however, converted spontaneously to sinus rhythm. During those episodes his quality of life was significantly impacted. Antiarrhythmic drug therapy with flecainide failed after a short period of success in suppressing AF. Four years ago he experienced a stroke, which occurred 1 day after a liposuction procedure. Fortunately he does not exhibit any residual effects. No other significant cardiovascular risk factors were apparent, thus having a CHADS2 score of 2. Due to increased symptoms, he elected to undergo AF ablation. Cardiac LGE-MRI was performed, and postimage acquisition processing revealed 22% atrial tissue fibrosis (Figure 40-2), fitting with stage III disease as depicted in Figure 40-3, which illustrates the Utah classification. Based on this individual’s extent of fibrosis, he was deemed eligible for ablation with an approach tailored to pulmonary vein antrum isolation (PVAI) and fibrotic area debulking. Immediate postablation, MRI demonstrated acute tissue lesions with regions of “no-reflow” at the posterior and septal wall (Figure 40-4), a predictor of appropriate scarring or lesion formation on MRI. Three months later MRI was repeated to assess chronic atrial scarring, which showed a scar burden of 19% of the LA volume (see Figure 40-2). Figure 40-5 illustrates 3 consecutive MRIs at preablation, immediate postablation, and 3 months postablation. At follow-up of 12 months the patient remains free of AF.
FIGURE 40-2 Three-dimensional LA reconstruction showing LASRM (A) and chronic LA scar (B) after PVAI and PWD. (A) LASRM estimated at 22% (stage III). (B) LGE-MRI 3 months post-AF ablation, exhibiting 19.1% LA scar.
FIGURE 40-3 Utah classification of LASRM, a quantitative LGE-MRI based clinical staging system reflecting disease progression of atrial fibrillation. Utah stage I (minimal) as <10% LASRM, stage II (mild) as ≥10% and <20%, stage III (moderate) as ≥20% and <30%, and stage IV (extensive) as ≥30%.
FIGURE 40-4 Three-dimensional LA reconstruction showing areas of no-reflow (yellow) indicating regions of catheter-induced tissue injury, immediately after AF ablation. Regions of no-reflow later enhance on 3 months postablation LGE-MRI, predicting permanent scar formation. Yellow, regions of no-reflow; blue, normal myocardium.
FIGURE 40-5 LGE-MRIs prior to ablation with LASRM, immediate postablation with dark regions of no-reflow at the posterior and septal wall (yellow arrows), and their transformation into areas that enhance on LGE-MRI, indicating permanent atrial scarring (red arrows) 3 months postablation.
CASE 3
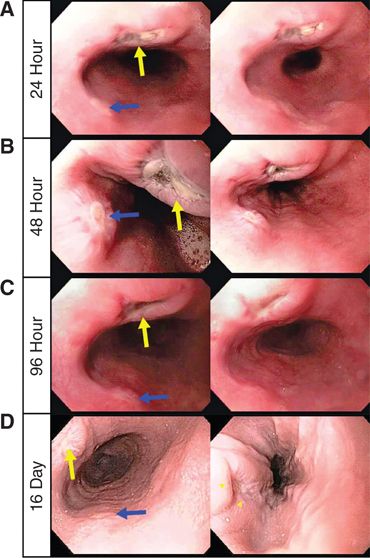
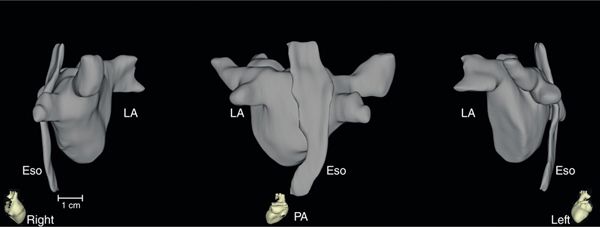
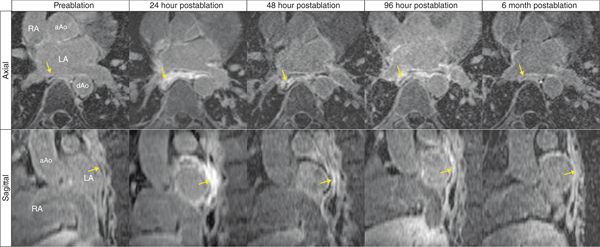
A 29-year-old man was referred to our electrophysiology clinic for paroxysmal AF. He reported having episodes of fast heart rates for several years, occurring at a frequency of 1 to 3 times per months, each lasting about 2 to 3 days. He had a remarkable family history with many family members with sudden cardiac death (SCD), cardiomyopathy, and early onset AF. A thorough workup including cardiac MRI was performed given his significant family history of SCD. MRI showed normal left ventricular function, no signs of ventricular delayed enhancement, myocardial infarction, or scar. Postimage acquisition processing revealed 24% left atrial fibrosis (Utah stage III; Figure 40-6). Hence the patient was eligible for catheter ablation for AF with a tailored approach of pulmonary vein antrum isolation (PVAI) and posterior wall debulking. Acute postablation MRIs were performed within 24 hours and uncovered extensive posterior wall and esophageal enhancement. A day following ablation the patient complained of symptoms of heartburn and some pain with swallowing. Endoscopy was performed showing esophageal injury at the level of the left atrium (maximum diameter 11 mm) with no bleeding 30 to 31 cm from the incisors (Figure 40-7). LGE-MRI was repeated at 48 and 96 hours following AF ablation. Three-dimensional segmentations of the preablation MRI in this patient demonstrated the close topographic anatomical relationship between the left atrium and the posteriorly located esophagus (Figure 40-8). Figure 40-9 shows the temporal evolvement of the esophageal lesions. Proton pump inhibitors were initially given intravenously, sucralfate suspension (1 gram per mouth 4 times a day for 5 weeks), and mechanically soft diet was instituted for 5 weeks. Repeat endoscopies over the next days showed progressive healing of the esophageal ulcerations. After a clinical follow-up of more than 12 months, the patient remains free of AF, without any gastrointestinal symptoms.
FIGURE 40-6 Three-dimensional LA reconstruction showing preablation LASRM of 24% fibrosis (stage III). Note the extensive fibrosis in this young patient (aged 29 years) with a CHADS2 score of 0.
FIGURE 40-7 Repeat upper gastrointestinal endoscopies at (A) 24 hours, (B) 48 hours, (C) 96 hours, and (D) 16 days post-AF ablation. Spatial and temporal development of two distinct esophageal lesions (lesion 1, yellow arrows; lesion 2, blue arrows).
FIGURE 40-8 Three-dimensional reconstruction of the LA and esophagus in right-lateral (left), PA (middle), and left-lateral (right) views. Note the close spatial anatomical proximity between the anterior-located LA to the posterior-located esophagus. The distance between these structures varies among individuals and is about 3 to 13 mm away from the LA endocardium (frequently around 5 mm).
FIGURE 40-9 Consecutive 2-D LGE-MRI slices in axial (top) and sagital (bottom) views. Catheter ablation caused significant LA posterior wall and esophageal wall (yellow arrows) enhancement, indicating remarkable thermal tissue injury. Note the spatial extention and temporal behavior of the thermal eosphageal injuries.
MRI TECHNOLOGY FOR IMAGING ATRIAL TISSUE
Late gadolinium enhancement magnetic resonance imaging has emerged as a key noninvasive modality in the armory of heart imaging in modern cardiology. The well established ability to assess precisely myocardial viability and accurately depict anatomy and function has lead to its widespread clinical use. Left atrial and pulmonary vein anatomy (including anatomic variability) and major thoracic structures such as the esophagus have been thoroughly investigated using MRI.1,2 Recently, the utility of LGE-MRI has been significantly expanded with the demonstration of its ability to assess atrial tissue changes that contribute to the arrhythmic substrate, as well as acute and chronic postablation tissue lesions. In this chapter, we illustrate these MRI-based approaches and emphasize how the clinical application of these modalities are instrumental in tailoring treatment by selecting appropriate ablation candidates and the adequate ablation strategy, and predicting individual ablation outcome.
ASSESSMENT OF ATRIAL STRUCTURAL REMODELING
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree