Technique of Colostomy Construction and Closure
Ian C. Lavery
A colostomy may be constructed as an end colostomy or a loop colostomy. An end colostomy is usually permanent, constructed after removal or permanent exclusion of the distal bowel. A loop colostomy is usually constructed with an intention to reverse it at a later date after a definitive procedure is performed. The number of permanent colostomies has decreased in recent years, and intestinal continuity is being restored with increasing frequency. Modern stapling equipment allows the construction of a temporary loop stoma. For an operation to proceed well technically and for the stoma to function satisfactorily, there must be great attention to detail, including preoperative counseling of the patient and preoperative planning by the surgeon.
End colostomies are usually constructed in the sigmoid colon or the distal end of the descending colon. They are formed as part of the reconstruction after an abdominoperineal resection. Less commonly, they are constructed as a permanent diversion for radiation proctitis, incontinence, or perianal sepsis. A temporary end colostomy may be constructed in an emergency situation, such as after a resection for perforated sigmoid diverticulitis or trauma of the distal bowel.
Temporary loop stomas are constructed to relieve a distal obstruction or to prevent stool from flowing over a recently constructed distal anastomosis.
If a colostomy is to be made electively, preoperative counseling and psychological preparation of the patient are desirable. A visit with an enterostomal therapist or a specially trained visitor from a lay organization, such as the United Ostomy Association, is helpful.
The most common problems that occur after construction of a stoma relate to placement of the stoma or peristomal sepsis. A stoma located incorrectly predisposes the patient to problems that cannot be managed conservatively (i.e., with changes in the stoma equipment). The objective of stoma construction is to provide an anatomically stable opening that allows placement of an ostomy management system that will maintain a seal for stool and gas for 5 to 7 days.
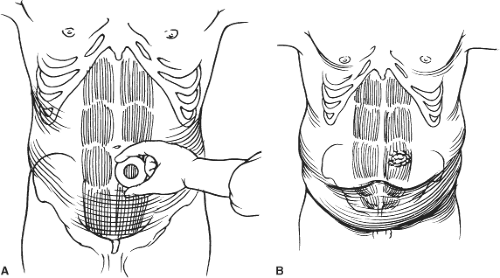
Most abdomens are not flat, muscular, and without scars. Most patients have some protuberance to their abdomen and lax musculature. Frequently, there are old incisions creating creases and weak musculature from neurovascular interruption. These circumstances make planning the location crucial to minimize postoperative problems. Locating the stoma is performed with the patient awake. An appropriately sized piece of equipment or a prepared disk of the same dimensions is used. The patient is marked while in supine, sitting, and bending positions. When the optimal site is determined, a tattoo is made with a sterile 27-gauge needle and indelible ink, so that when the abdomen is prepared and opened and the anatomic relationships are distorted, the site cannot be mistaken. The usual site in an average individual is on the apex of the subumbilical fat roll (Fig. 1A).
Primarily, the stoma must be constructed so that it is visible (i.e., not located on the inferior surface of a pendulous abdomen). The stoma should be away from the umbilicus, skin creases, scars, and bony prominences. Skin damaged by radiation or skin grafts should be avoided. In an obese individual with a pannus, the stoma is located in the upper abdomen, away from creases, where it is visible and the skin flat (Fig. 1B).
End Colostomy
An end colostomy is usually constructed in conjunction with some other procedure. If a stoma is to be constructed, my preference is to make the abdominal incision in the midline to avoid interfering with the rectus sheath or the rectus muscle and to preserve each quadrant of the abdomen for future use, should the need arise for relocation or revision of the stoma. One of the prerequisites to constructing an adequate stoma is to have sufficient bowel mobilized to bring the terminal portion to the skin level without tension. The left colon and the sigmoid colon must be mobilized, and the splenic flexure is taken down in certain circumstances. After an abdominoperineal resection, the sigmoid colon is mobilized as part of the primary procedure. Mobilization commences at the peritoneal reflection in the left paracolic gutter, and the dissection is carried medially in the avascular plane anterior to the gonadal vessels and the ureter. Mobilization is taken to the midline and medial to the duodenojejunal flexure. The more obese the patient, the more mobilization is necessary. Mobilization to the medial aspect of the duodenojejunal flexure allows the colon to be draped anterior to the small intestine en route to the stoma site in the rectus muscle. This avoids the need to close the mesenteric defect and essentially eliminates the possibility of a volvulus of the
small intestine around the left colon. Mobilization should be sufficient to enable several centimeters of bowel to protrude without tension through the abdominal wall.
small intestine around the left colon. Mobilization should be sufficient to enable several centimeters of bowel to protrude without tension through the abdominal wall.
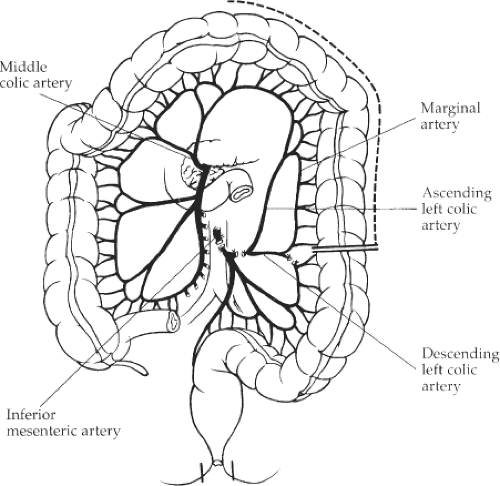
An adequate blood supply is an integral part of achieving the construction of a satisfactory end colostomy. When performed in conjunction with an abdominoperineal resection, the inferior mesenteric artery is divided at its origin, proximal to the origin of the left colic artery. The left colic artery is divided proximal to its bifurcation into the ascending and descending left colic artery. As the inferior mesenteric artery is divided at its origin, the entire sigmoid colon must be resected because its arterial blood supply has been divided. The bowel is transacted at the junction of the descending and sigmoid colon, where it is perfused with blood from the middle colic artery through the marginal artery. A collateral blood supply is provided through the descending left colic and the ascending left colic arteries, through which the blood flow is reversed (Fig. 2). It is absolutely essential to check the blood supply, especially in the aged population, in which atheroma may be prominent, and diminish the blood supply through the marginal artery. If the end colostomy is being constructed for a condition that does not require resection of the sigmoid and rectum, there is less likelihood of a compromise of the blood supply. However, it is important to check the blood supply and ensure that the vasculature to the descending or sigmoid colon is not undercut during division of the mesentery. The blood supply is checked by observing the blood flow from the cut end of the bowel. If the blood flow is not bright and pulsatile, further bowel should be resected until this is achieved.
At the time of transection of the bowel, both ends of the colon are closed with a suture, or, more conveniently, with a stapling instrument. This maneuver minimizes contamination and allows the divided bowel to be brought through the site in the abdominal wall with minimal contamination.
Preparation of Ostomy Site
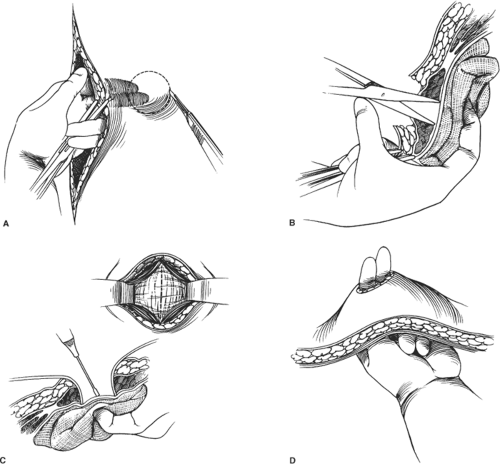
Before the abdomen is opened, the optimal site for the stoma is marked, as discussed previously. The layers of the abdominal wall are oriented correctly and held in place with clamps attached to the edge of the rectal sheath and the dermis of the skin. While the layers of the abdominal wall are held in alignment, a circular disk of skin 2 cm in diameter (approximately the size of a quarter) is excised (Fig. 3A). Only the skin is removed, which preserves subcutaneous fat. This procedure is best performed with a scalpel to ensure that the opening is circular. A circular opening facilitates postoperative management. After the skin disk has been removed, while the abdominal wall is elevated and alignment of the layers of the abdominal wall is maintained, the fat is incised with a vertical incision down to the anterior rectus sheath. A linear incision is made in the anterior rectus sheath to expose the rectus muscle. The fibers of the rectus muscle are then split longitudinally by opening an instrument perpendicular to the line of the fibers (Fig. 3B). This procedure results in little or no bleeding unless the deep inferior epigastric vessels are encountered and divided deep to the rectus muscle. Caution should be taken to avoid this injury, as it can cause troublesome bleeding. If injury to the blood vessels occurs, hemostasis is secured by inserting an instrument through the opening in the abdominal wall and reflecting the medial part of the incision upward so that the vessel is exposed from the peritoneal aspect of the operative field, where it may be controlled with electrocoagulation or ligation.
After the rectus muscle is split and retracted, the posterior rectus sheath is divided (Fig. 3C). The opening in the abdominal wall should allow two average-sized fingers to pass through to the second phalanx (Fig. 3D). An opening of this size permits the construction of a colostomy through the strongest fascia and muscle of the abdominal wall, which minimizes the development of a hernia or prolapse, although with the passage of time, both these situations may develop. All muscle fibers and the fibers of the anterior and posterior rectus sheath remain intact and help to support the intestine as it passes through the abdominal wall.
After preparation of the stomal opening, the terminal portion of the intestine is grasped with a noncrushing clamp and slowly maneuvered through the abdominal wall so that 3 to 4 cm protrudes without tension (Fig. 4A). With adequate medial mobilization of the left colon, it is unnecessary to attempt to close the mesenteric defect by suturing the mesentery to the parietal peritoneum. With the terminal portion of the intestine through the abdominal wall, the remainder of the intraperitoneal operation is completed. The abdominal wound is closed, and the skin adjacent to the stoma is approximated in the usual manner. In obese patients, or if the wound has been contaminated, it is desirable to leave the skin wound open or to close it loosely and hold it open with wicks. The wound is then protected, and the closed terminal portion of the intestine is excised (Fig. 4B). At this stage, it is important to be sure the blood supply is adequate by seeing pulsatile bleeding. If bleeding is not pulsatile, further
resection is required. The maturation of the colostomy usually requires eight evenly spaced sutures in the circumference, which sutures the full thickness of the bowel to the dermis of the abdominal wall (Fig. 4C). Sutures of 3-0 chromic catgut are used. After construction of the stoma, an appliance is placed over the stoma. If the stoma works in the early postoperative period, an appliance prevents the adjacent abdominal incision from being contaminated, and the patient is not subjected to the indignity of having feces on the abdomen.
resection is required. The maturation of the colostomy usually requires eight evenly spaced sutures in the circumference, which sutures the full thickness of the bowel to the dermis of the abdominal wall (Fig. 4C). Sutures of 3-0 chromic catgut are used. After construction of the stoma, an appliance is placed over the stoma. If the stoma works in the early postoperative period, an appliance prevents the adjacent abdominal incision from being contaminated, and the patient is not subjected to the indignity of having feces on the abdomen.
Special Considerations
Obesity
The morbidly obese patient poses special problems when it comes to constructing a colostomy. The stoma must be located in the upper abdomen, where the skin is flat and the stoma is visible to the patient. Preoperative marking is essential. In a thin individual, location of the stoma in a less than perfect position can usually be managed, albeit with difficulty. In an obese patient, this is not possible, and any attempt to locate the stoma without previous marking inevitably leads to serious postoperative difficulties. With respect to mobilization of the colon, much more colon needs to be freely mobilized to allow the terminal portion to reach the skin without tension. The entire left colon needs to be mobilized. The distal transverse colon frequently needs to be mobilized with removal of the greater omentum from the colon to minimize the amount of tissue within the abdominal wall. It is sometimes necessary to divide the
inferior mesenteric vein at the lower border of the pancreas to release the tethering action at this level. This maneuver provides an extra length of bowel that is quite remarkable and does not interfere with the blood supply.
inferior mesenteric vein at the lower border of the pancreas to release the tethering action at this level. This maneuver provides an extra length of bowel that is quite remarkable and does not interfere with the blood supply.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree