T-cell Prolymphocytic Leukemia
Kathryn Foucar, MD
Key Facts
Etiology/Pathogenesis
Key leukemogenic role of TCL1 oncoprotein overexpression
Translocations of TCL1 gene(s) into promoter/enhancer regions of TCRα/δ
Image Findings
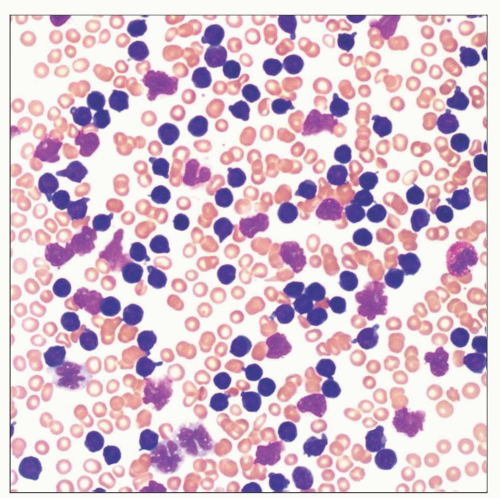
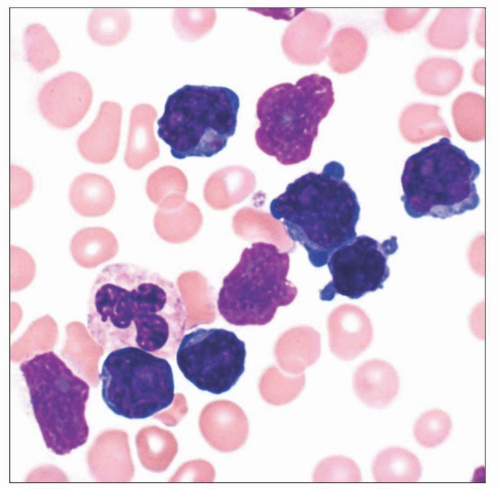
CBC and blood smear morphology
Rapidly rising white blood cell count (WBC)
Microscopic Pathology
Striking lymphocytosis in blood
Extensive diffuse bone marrow effacement with variable reticulin fibrosis
Ancillary Tests
Key test to determine lineage and stage of maturation by flow cytometry
Flow cytometry useful in distinguishing T-PLL from other T-cell leukemias
Recurrent cytogenetic marker in 90% of cases
inv(14)(q11q32) results in translocation of TCL1
TCL-1 oncoprotein overexpression is leukemogenic
Top Differential Diagnoses
Sézary syndrome
Adult T-cell leukemia/lymphoma
T-cell large granular lymphocytic leukemia
T lymphoblastic leukemia
Reporting Considerations
Integrate morphology, immunophenotype, and cytogenetics
Alert clinician regarding CAMPATH (alemtuzumab) therapy
TERMINOLOGY
Abbreviations
T-cell prolymphocytic leukemia (T-PLL)
Synonyms
T-cell chronic lymphocytic leukemia
Definitions
Mature T-cell leukemia composed of small to medium-sized lymphocytes
Variably prominent nucleoli
Variable nuclear irregularity
Scant to moderate amounts of cytoplasm
Recurrent cytogenetic finding: inv(14)(q11q32)
ETIOLOGY/PATHOGENESIS
Leukemogenesis
Key leukemogenic role of TCL1 oncoprotein overexpression
Translocations of TCL1 gene(s) into promoter/enhancer regions of TCRα/δ dysregulates TCL1
ATM deletions and haploinsufficiency of CDKN1B also leukemogenic
CLINICAL ISSUES
Epidemiology
Incidence
2% of chronic leukemias in adults
Increased incidence in patients with ataxia telangiectasia
No association with environmental exposure
No link to infections established
Age
Median: 65 years (range: 30-90 years)
Gender
Male predominance (3:1)
Ethnicity
No key ethnic associations
Site
Blood, bone marrow, spleen, liver, lymph nodes
Less often skin, effusions
Presentation
90% of patients symptomatic
Key symptoms include abdominal distension, bulky lymph nodes, skin rash
Marked splenomegaly and hepatomegaly typical
Skin lesions and pleural effusions in subset
Laboratory Tests
Key laboratory tests include CBC with differential, flow cytometric immunophenotyping, and conventional cytogenetics
CBC shows marked lymphocytosis (WBC > 100 × 109/L in 50% of cases)
Additional CBC findings include anemia (25%) and thrombocytopenia (50%)
Natural History
Aggressive disease; 20% overall 5-year survival rate
Better outcome for responders to CAMPATH-1H
Treatment
Drugs
Various agents used, including purine analogs
Best results achieved with humanized monoclonal antibody alemtuzumab (anti-CD52) (CAMPATH-1H)
Newer treatments include
Other monoclonal antibody agents
Nonmyeloablative stem cell transplant
Radioimmunotherapy
MICROSCOPIC PATHOLOGY
Microscopic Features in Blood and Bone Marrow
Striking lymphocytosis in blood
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree