T-cell Large Granular Lymphocytic Leukemia
Kaaren K. Reichard, MD
Key Facts
Clinical Issues
Asymptomatic
Symptomatic: Recurrent infections (neutropenia)
Rheumatoid arthritis/other autoimmune diseases
Splenomegaly
Pure red cell aplasia
Microscopic Pathology
Peripheral blood
LGL lymphocytosis
LGLs generally > 2 × 109/L
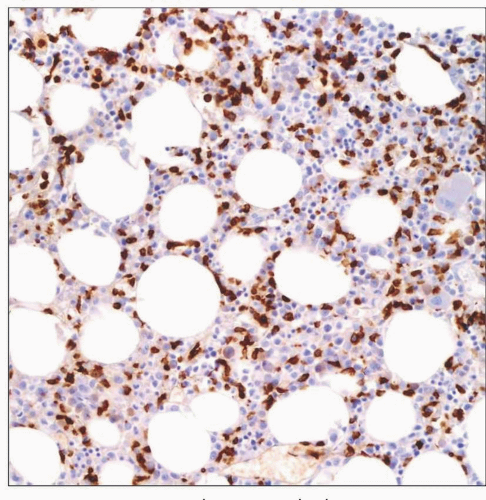
Bone marrow (BM)
Extent of involvement is variable
Interstitial/intrasinusoidal patterns common
May be morphologically occult
Immunostains helpful to identify T-LGL infiltrate
Ancillary Tests
Immunophenotype
CD3(+), CD8(+), CD57(+), CD94(+), TCR-α/β(+)
Cytoplasmic granules TIA-1, perforin, GZMM(+)
Uniform expression of TCR-Vβ or KIR molecules
Molecular
T-cell receptor genes rearranged
Top Differential Diagnoses
Reactive/persistent LGL lymphocytosis
Chronic natural killer (NK) cell leukemia/lymphocytosis
Immunophenotype: CD2(+), CD3(-), CD16(+), CD56(+)
Aggressive NK cell leukemia
Epstein-Barr virus associated
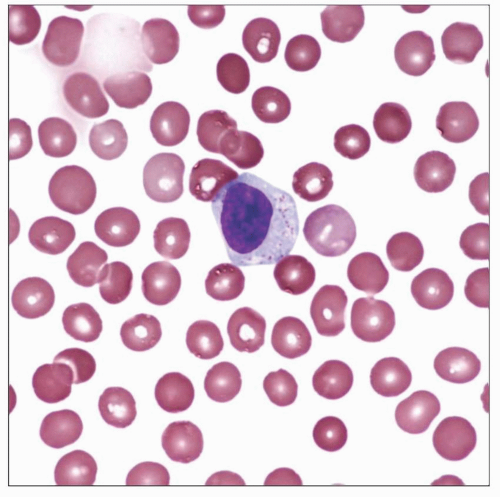 Classic appearance of a large granular lymphocyte (LGL) is shown. LGLs constitute up to 15% of circulating white blood cells normally. Immunophenotyping shows that most are cytotoxic T cells. |
TERMINOLOGY
Abbreviations
T-cell large granular lymphocytic leukemia (T-LGL leukemia)
Definitions
Persistent clonal proliferation of T-cell large granular lymphocytes (T-LGLs)
ETIOLOGY/PATHOGENESIS
Hypotheses
Chronic antigenic stimulation resulting in proliferation of T-cell large granular lymphocytes (T-LGLs)
Exogenous antigens such as HTLV
Endogenous autoantigens
Inhibition of apoptosis resulting in accumulation of T-LGLs
Dysregulation of FAS/FAS-L
Infectious Agents
Role of retroviral infection unclear
Most patients do not show evidence of HTLV-I or HTLV-II infection
Reactivity against small peptide derived from an HTLV-I envelope protein has been reported
Etiology of Neutropenia
FAS/FAS-L-induced premature apoptosis of granulocytic precursors
CLINICAL ISSUES
Epidemiology
Incidence
Comprises 2-3% of chronic lymphocytic leukemias
Age
Median age: 60 years
Predominantly affects adults
Gender
No gender predilection
Site
Peripheral blood (PB)
Bone marrow (BM)
Spleen
Liver
Presentation
Asymptomatic
Incidental discovery of T-LGL lymphocytosis
Asymptomatic
Cytopenias
No clinically appreciated effects
Rheumatoid arthritis or autoimmune disorder (25-35% of patients)
Splenomegaly (20-50% of patients)
Symptomatic
Development of cytopenias
Neutropenia
Thrombocytopenia
Anemia: May be due to red cell aplasia
Development of recurrent infections
Often bacterial
Mucocutaneous
Splenomegaly
Systemic symptoms
LGL lymphocytosis: LGLs generally > 2 × 109/L
Laboratory Tests
Clinical examination
Complete blood cell count with differential
PB examination
BM examination if needed
Flow cytometry of PB &/or BM
T-cell receptor clonality studies
Natural History
Clinically heterogeneous
Some spontaneous regressions
Association with immune disorders
High proportion of patients will require treatment at some point
Treatment
Asymptomatic
Careful observation
Symptomatic
Methotrexate or cyclophosphamide or cyclosporine A
Treatment should be continued for at least 4 months to assess response
Corticosteroids
As monotherapy, not very effective long-term
Rapid improvements in symptoms/cytopenias if used in conjunction with methotrexate, cyclophosphamide, cyclosporine A
Prophylactic use of antibiotics if severe neutropenia
Hematopoietic growth factors
GM-CSF or G-CSF for neutropenia
Erythropoietin (EPO) for anemia
Clinical trial
As available
Progressive disease
Nucleoside analogues
Alemtuzumab: Anti-CD25 monoclonal antibody
Hematopoietic stem cell transplantation
Prognosis
Generally indolent
Related to control of cytopenias and associated symptoms
MICROSCOPIC PATHOLOGY
Peripheral Blood
LGL lymphocytosis
LGLs generally > 2 × 109/L
Occasional cases LGLs < 2 × 109/L
Circulating T-LGLs
Intermediate size
Round/slightly indented nucleus
Inconspicuous nucleoli
Abundant pale cytoplasm
Cytoplasmic azurophilic granules
Variable degrees/types of cytopenias
Generally unremarkable red blood cell, platelet, and myeloid morphology
Bone Marrow
Variably cellular
Usually normo- or hypocellular

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree