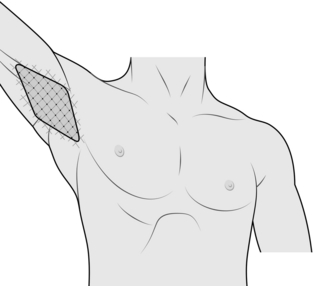
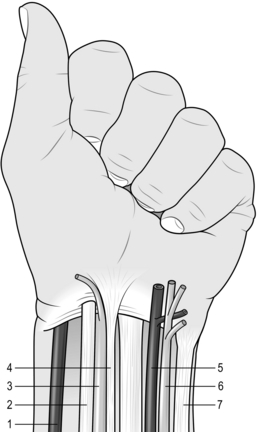
25 1. Hyperhidrosis is uncontrolled profuse sweating. It is classified as either local, affecting only specific areas, or general, affecting most parts of the body. It affects up to 2% of the population, and there is probably a genetic predisposition. The axillae are affected in 60% of cases, the palms (often with the feet) in 30%, the head and neck in 10% and the rest of the body, especially under the breasts in females and groins in 5%. Even in localized cases of hyperhidrosis more than one localized area is often affected. 2. It is a social problem. Confirm the diagnosis is of hyperhidrosis (hyper = over + hidros = sweat) and not a complaint of malodour or other dermatological problems such as hydradenitis suppurativa (chronic infection of the apocrine sweat glands). In general those with hyperhidrosis do not have body malodour and the sweat is clear and profuse. Examine each potentially affected area to confirm this. 3. Identify an underlying cause. Primary causes tend to result in generalized rather than localized hyperhidrosis. Endocrine causes include thyroid dysfunction and progesterone/oestrogen imbalance, as occurs with polycystic ovary syndrome or the menopause. Take blood samples on the first consultation. Head injury or the use of certain medications can also produce hyperhidrosis. 4. Determine the severity of the hyperhidrosis by determining specific occasions when hyperhidrosis is a problem. Sweating may occur at a lower than usual ambient temperature and may be precipitated during social confrontation. It is not always necessary to use a social anxiety psychological scoring systems to demonstrate this, but determining the use of avoidance techniques indicates the degree of severity. Axillary sweaters often prefer wearing black or dark tops, doubled so sweat stains do not show. They insert tissues or commercially purchased pads and avoid loose singlets. Palm sweaters may carry a hand-held article to avoid shaking hands on greeting and hold hands only outside in the cold. True plantar sweaters wear loose, regularly replaced shoes, because sweat rots the fabric. Forehead sweaters tend to avoid spicy foods. For research purposes the degree of sweating within a heated ambience can be assessed by the weight increase of applied blotting paper. 5. Arrange a sensitively conducted psychological assessment, clarifying its potential benefits. Emphasize that hyperhidrosis is a life-long problem capable only of alleviation by intervention, not cure. 1. Aim to treat both the physical and psychological effects. Tailor the range of proffered management to the site, severity, awareness of involved area and perceived severity of disability. Involve the fully informed patient in planning management, fully aware of the implications, actively concurring. Re-discuss the planned treatments and potential side-effects before you embark on a new treatment. 2. Patients with localized hyperhidrosis will usually have tried over-the-counter antiperspirants, often aluminium salt-based. The low pH of these can produce skin irritation, but if they are effective further treatment is not necessary. For primary generalized hyperhidrosis consider oral medications, in particular anticholinergic drugs, such as propantheline or glycopyrrolate (Robinul). After warning of potential anticholinergic side-effects, such as headaches, nausea, urinary hesitancy, blurred vision and palpitations, start with a morning low dose and build up. It is usually best taken in the morning as clients find it is effective for only 4 to 6 hours. Do not normally prescribe it for localized hyperhidrosis except as an adjunctive. 3. Iontophoresis is a ‘home based’ machine method of reducing localized hyperhidrosis. The treatment involves immersing the affected feet or hands area in baths of shallow tap water or placing a wet pad in the axilla. The machine discharges an electronic current through the water which is channelled to the affected area by placing two electrodes in contact with the patient to form a circuit. Iontophoresis can also be used to deliver a chemical through the skin by adding glycopyrolate to the solution. Published results are good, but compliance is often poor, as the bulky machine has to be used regularly. This is time consuming and in practice results are variable. 1. subdermal injection of Botox, by its localized anticholinergic action, is very successful at reducing hyperhidrosis. The effect lasts for 6 months as the acetylcholine vesicles regenerate. 2. It is used predominantly to manage axillary hyperhidrosis; its use in palmar or plantar hyperhidrosis often requires a local nerve block as the subdermal injections are uncomfortable. Ensure that you are fully trained in how to deliver ulnar and median blocks: repeated general anaesthesia instead is not appropriate. There is a small risk of infection which could result in palmar fasciitis, and the injections can lead to localized fingertip numbness. Botox injection to the forehead and hairline has some effect on reducing the sensation of facial sweating. 1. Define the area of hyperhidrosis by painting the affected region with iodine and, when dry, sprinkling starch powder over it. The affected area will be a blackened colour. Mark the outer margins of the area and then mark out a 1-cm square grid within it (Fig. 25.1). 2. Ensure that the Botox solution is drawn up beforehand; 4 ml of 2% lidocaine is added to 100 units of Botox and drawn up into four 1-ml syringes with fine needles (as used by insulin-dependent diabetics). Deliver a 0.1 ml dose to the centre of each grid. Work smoothly and quickly over a couple of minutes. 3. The patient is free to leave 30 minutes later after ensuring there are no systemic side-effects, which are rare. 1. Make a small skin crease incision less than 0.5 cm in the mid axilla. 2. Through the incision inject about 200 ml of normal saline with 15 ml of 1% lidocaine and adrenaline subdermally, using a long needle and syringe. This tumescence lifts the skin off the under-lying adipose tissue of the axilla. 3. A curette (3 mm) is then passed through the incision just deep to the skin out to the margin of the hairline. With the roughened edge faced upwards and the curette tenting the skin, it is with-drawn towards the incision, abrading the underside of the skin and destroying the subdermal structures. The procedure is repeated in a sweeping fashion clockwise around the incision so that all the hyperhidrosis area is treated. Take time to ensure that all areas are treated and take care not to make the skin too shallow and button-hole it, or pass the curette too deep and damage deeper structures. 4. A steri-strip over the wound is sufficient. Place a gauze swab in the axilla and secure it firmly with wide adhesive tape.
Sympathectomy and the management of hyperhidrosis
ASSESSMENT OF HYPERHIDROSIS
Appraise
MANAGEMENT OF HYPERHIDROSIS
SUBDERMAL INJECTION OF ATTENUATED BOTULINUS TOXIN (BOTOX)
Appraise
Action
LOCALIZED RETRODERMAL AXILLARY CURETTAGE
Action
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sympathectomy and the management of hyperhidrosis