Jim McCarthy
Sutures, Needles, and Instruments
Sutures, needles, and instruments are the tools of the surgical team that are necessary to successfully complete a surgical procedure. It is the responsibility of the perioperative nurse to understand these tools and be proficient with their preparation for surgery. Although there are many other aspects of the perioperative registered nurse (RN) role that ensures the expected outcome of a surgical intervention, these items are the basis for surgical procedures. This chapter describes and illustrates a basic knowledge for the perioperative RN, but as the surgical arena continues to evolve, especially technologically, the perioperative RN should be receptive to change and develop proficiencies in new surgical devices and techniques.
Suture Materials
The development of surgical sutures has been closely associated with the development of the art and science of surgery. Medical writings of ancient Egyptian and Assyrian cultures dating back to 2000 BC mention the various materials used, to a limited extent, for suturing and ligating. The concept of suturing and ligating also is recorded in the writings of the father of medicine, Hippocrates, born 460 BC. Gut of sheep intestines was first mentioned as suture material by the ancient Greek physician Galen. The Persian physician and philosopher Rhazes is credited with using surgical gut, or catgut, in AD 900 for suturing abdominal wounds. However, the word catgut is a misnomer, and its use is inappropriate. According to the Oxford English Dictionary, it refers to the Dutch word kattedarm, “cat-intestine.” Use of the term catgut was adopted by the English around 1560 to 1600 under obscure conditions, possibly connected humorously with caterwauling.
Suture is a generic term for all materials used to repair and reapproximate incised or torn tissues. The primary goal is to encourage wound healing of the injured tissue to reduce the risk of infection. To suture is to stitch together cut or torn edges of tissue (Mosby’s Dictionary, 2012). A ligature is a strand of suture material used to tie off or occlude blood vessels to prevent bleeding, or to isolate a mass of tissue for excision. A variety of suture materials are available for ligating, suturing, and closing the wound. The choice of suture takes into consideration several characteristics, such as the following: absorbable versus nonabsorbable, tensile strength, monofilament or multifilament (braided), ease of knot tying, and the inflammatory response of the tissue. An understanding of the characteristics of suture materials, knowledge of the risk factors of wound healing, and awareness of the interactions between tissues and suture materials for proper wound healing is essential for the perioperative nurse, as well as all members of the surgical team.
Characteristics of Suture Material
Key features used to evaluate the general properties of suture material are (1) physical characteristics, (2) handling characteristics, and (3) tissue-reaction characteristics (Box 7-1).
The ideal suture material is one that causes minimal inflammation and tissue reaction while providing maximal strength during the lag phase of wound healing (see Chapter 9). There is no ideal suture for every application, and even the best application presents risks of individual suture failure. Perioperative nurses should evaluate the characteristics of sutures to determine the ideal choice for surgical patient care and incorporate research findings into their clinical practice.
Physical Characteristics.
Physical characteristics of sutures are defined and described by the United States Pharmacopeia (USP), which is the official compendium for suture manufacture. Characteristics can be measured or visually determined and include the following properties:
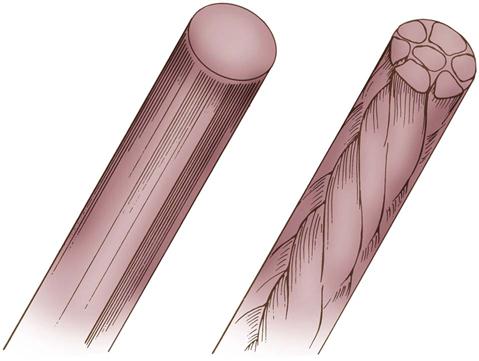
• Physical configuration: Suture material can be single-strand (monofilament) or multistrand (multifilament), containing numerous fibers rendered into a single thread by twisting or braiding (Figure 7-1).
• Capillarity: The ability to transmit fluid along the strand.
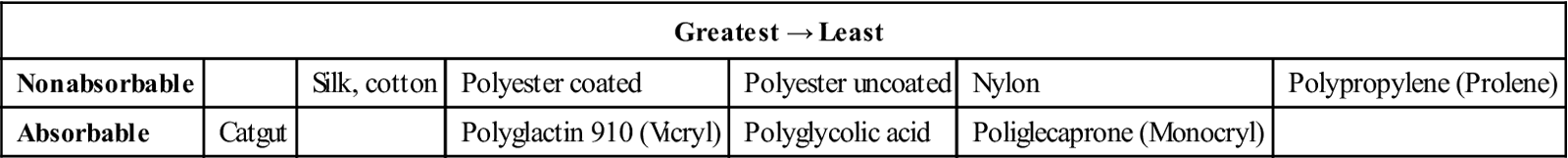
• Tensile strength: The amount of weight (breaking load) necessary to break a suture (breaking strength); it varies according to the type of suture material (Table 7-1)
TABLE 7-1
Relative Straight-Pull Tensile Strength of Suture Materials
| Greatest → Least | |||||||
| Nonabsorbable | Steel | Polyester (Mersilene) | Nylon (monofilamentous) | Nylon (braided) | Polypropylene (Prolene) | Silk | |
| Absorbable | Polyglycolic | Polyglactin 910 (Vicryl) | Polydioxanone (PDS) | Poliglecaprone (Monocryl) | Catgut | ||
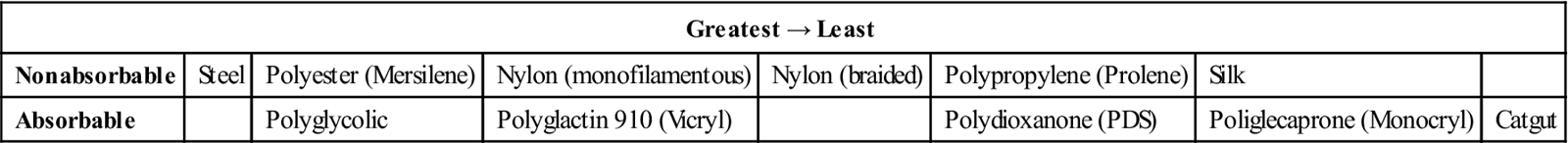
Modified from Ethicon wound closure manual, available at http://academicdepartments.musc.edu/surgery/education/resident_info/supplement/suture_manuals/ethicon_wound_closure_manual.pdf. Accessed March 10, 2013.
Handling Characteristics.
Handling characteristics of suture material are related to pliability (e.g., how easily the material bends) and the coefficient of friction (e.g., how easily the suture slips through tissue and can be tied). A suture with a high friction coefficient tends to drag through tissue. It is more difficult to tie because its knots do not set easily. Some suture materials are coated to reduce their coefficient of friction. This coating not only improves the way they pull through tissue on insertion but also lessens the force needed to remove the suture after the wound is healed. The coefficient of friction should not be too low, however, because then knots will be loosened too easily.
Tissue-Reaction Characteristics.
Because it is a foreign substance, all suture materials cause some tissue reaction. Tissue reaction begins when the suture inflicts injury to the tissue during insertion. In addition, tissue reacts to the suture material itself (Table 7-2). This reaction begins with an infiltration of white blood cells into the area; macrophages and fibroblasts then appear; and by about the seventh day, fibrous tissue with chronic inflammation is present. The reaction persists until the suture is encapsulated (nonabsorbable material) or absorbed (absorbable material) by the body.
TABLE 7-2
Relative Tissue Reactivity to Sutures
| Greatest → Least | ||||||
| Nonabsorbable | Silk, cotton | Polyester coated | Polyester uncoated | Nylon | Polypropylene (Prolene) | |
| Absorbable | Catgut | Polyglactin 910 (Vicryl) | Polyglycolic acid | Poliglecaprone (Monocryl) | ||
Modified from Ethicon wound closure manual, available at http://academicdepartments.musc.edu/surgery/education/resident_info/supplement/suture_manuals/ethicon_wound_closure_manual.pdf. Accessed March 10, 2013.
Types of Suture Material
Suture materials are classified into two main groups: absorbable and nonabsorbable. The suture may then be divided into two subgroups: braided and monofilament. Absorbable sutures have varying lengths of absorption time, which affects healing time and strength of the closure.
Absorbable Sutures.
The USP defines an absorbable surgical suture as “sterile, flexible strand prepared from collagen derived from healthy mammals, or from a synthetic polymer….” It is capable of being absorbed by living mammalian tissue but may be treated to modify its resistance to absorption. It may be modified with respect to body or texture. It may be impregnated with a suitable coating, softening, or antimicrobial agent. It may be colored by a color additive approved by the U.S. Food and Drug Administration (FDA).
Absorbable sutures can be digested (by enzyme activity) or hydrolyzed (broken down by reaction with water in tissue fluids) and assimilated by the tissues during the healing process. Absorbable sutures vary in treatment, color, size, packaging, and resistance to absorption, according to their purpose. Types of absorbable suture include plain or chromic surgical gut, collagen, and glycolic acid polymers (Table 7-3).
TABLE 7-3
Comparison of Absorbable Sutures
| Ethicon | Covidien | Configuration | Tensile Strength | Absorption Rate |
| Surgical gut (plain) | Plain gut | Twisted | 0% at 2-3 wk | Unpredictable (12 wk) |
| Surgical gut (chromic) | Chromic gut | Twisted | 0% at 2-3 wk | Unpredictable (12 wk) |
| Polyglactin 910 (Vicryl Rapide) | Braided | 0% at 14 days | Complete at 42 days | |
| Poliglecaprone (Monocryl) | Monofilament | 20%-30% at 2 wk | Complete in 91-119 days | |
| Polyglycolic acid (Dexon S) | Braided or monofilament | 20% at 3 wk | Complete in 60-90 days | |
| Polyester (Polysorb) | Braided | 30% at 3 wk | Complete in 56-70 days | |
| Polycaprolate (Dexon II) | Braided | 35% at 3 wk | Complete in 60-90 days | |
| Polydioxanone (Biosyn) | Monofilament | 40% at 3 wk | Complete in 90-110 days | |
| Polyglactin (Vicryl 910) | Braided or monofilament | 50% at 3 wk | Complete in 56-70 days | |
| Polydioxanone (PDS) | Monofilament | 60% at 3 wk | Complete within 6 mo | |
| Polyglyconate (Maxon) | Monofilament | Excellent until 6 wk | Complete within 6 mo |
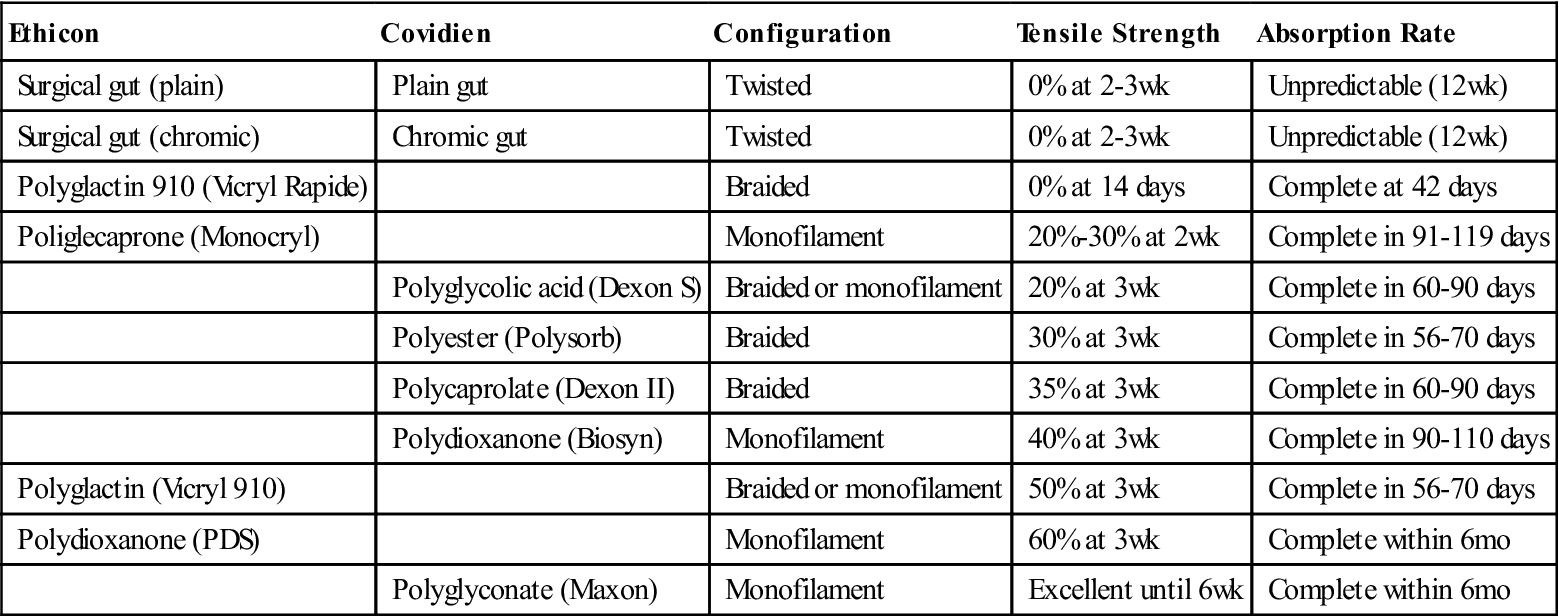
Modified from Ethicon wound closure manual, available at http://academicdepartments.musc.edu/surgery/education/resident_info/supplement/suture_manuals/ethicon_wound_closure_manual.pdf. Accessed, March 10 2013; Covidien suture catalog, available at www.covidien.com/campaigns/pagebuilder.aspx?topicID=181589&page=SPC:Main. Accessed March 10, 2013.
Surgical Gut.
Surgical gut is obtained from the collagen of the submucosal layer of the small intestine of sheep or the intestinal serosa of cattle or hogs. The processed strands or ribbons of collagen are either untreated (plain, type A) or treated with chromium salts (chromic, type C).
Chromatization delays absorption of the suture in living mammalian tissue. The strength of the chromium salt content and the duration of the chromatizing process are accurately controlled and tested. Proper chromatizing of gut ensures the integrity of the suture and maintenance of its strength during the early stages of wound healing. It enables a wound with slow healing power to heal sufficiently before the suture is entirely absorbed.
The elaborate processes of mechanical and chemical cleaning of the raw gut are followed by sterilization, usually with ionizing radiation, and storage in hermetically sealed packages. Modern manufacturing processes also ensure tensile strength, more controlled absorption, and more predictable results.
Absorption occurs by digestion of the gut by tissue enzymes. The absorption rate of surgical gut is influenced by the type of body tissue it contacts and, to some extent, by the patient’s general physical condition. Studies also show that surgical gut is absorbed faster in serous or mucous membranes than in muscular tissues. When fine chromic gut is properly buried in successive layers of the gastrointestinal tract, it retains its strength long enough for primary union to take place.
Surgical gut suture is wet-packaged in an alcohol solution to provide maximal pliability and should be used immediately after removal from the packet. When a gut suture is removed from its packet and is not used at once, the alcohol evaporates, which causes the strand to lose its pliability. If required, the strand’s pliability may be restored just before use by immersing it in sterile water or normal saline solution, preferably at body temperature, for only a few seconds. This immersion is recommended only for eye sutures; in other areas, tissue fluids moisten the gut sufficiently as it passes through the tissue when the surgeon sews. Excessive moisture reduces tensile strength.
Collagen Sutures.
Collagen sutures are derived from cattle tendons. They are chemically treated to remove noncollagenous material, purified, and processed into strands that have physical properties superior to those of surgical gut. Collagen suture is used most often as a fine suture material for the eye.
Synthetic Absorbable Sutures.
To produce synthetic absorbable sutures, specific polymers are extruded into suture strands. The base material for synthetic absorbable sutures is a combination of lactic acid and glycolic acid polymers (Vicryl, Dexon, and Polysorb). The molecular structure of these products has a tensile strength sufficient for approximation of tissues for 2 to 3 weeks, followed by rapid absorption.
Other synthetic polymers (PDS, Maxon, and Monocryl) provide wound support for longer periods (3 months). They are used when prolonged support for wound healing is desired, as with fascial closure or for elderly or oncology patients. They combine the desirable qualities of extended wound support and eventual absorbability.
An additional type of synthetic absorbable suture approved by the FDA is MonoMax. Recombinant deoxyribonucleic acid (DNA) technology is used to produce this poly-4-hydroxybutyrate suture. This suture has a high degree of flexibility and maneuverability, but may have limitations for use in patients who are allergic to the cells or the growth medium used for its production. The suture is not indicated for use in cardiovascular or neurologic tissues or for microsurgery or ophthalmic surgery. It has been used in laparotomy closure (Research Highlight).
Synthetic absorbable sutures are absorbed by slow hydrolysis in the presence of tissue fluids. Hydrolysis is the chemical process whereby the polymer reacts with water to cause an alteration of breakdown of the molecular structure. These sutures are degraded in tissue by this process at a more predictable rate than surgical gut (or collagen) and with less tissue reaction. These sutures are dry-packaged in sizes 10-0 to #3. They should not be dipped in solutions because moisture reduces their tensile strength. Some polymers have additional coatings to reduce drag in tissue.
Nonabsorbable Sutures.
Nonabsorbable sutures are strands of material that effectively resist enzymatic digestion in living animal tissue. The USP classifies nonabsorbable surgical suture as follows:
The strand of suture material may be uncoated or coated with a substance to reduce capillarity and friction when passing through the tissue. Several products are used for coating, including silicone, polytef (Teflon), and various polymers. Fibers may be uncolored, naturally colored, or impregnated with a suitable dye.
Nonabsorbable suture material is encapsulated or walled off by the tissues around it during the process of wound healing. Skin sutures, for which nonabsorbable materials are often the choice, are removed before healing is complete. The most common nonabsorbable suture materials are silk, nylon, polyester fiber, polypropylene, and stainless steel wire (Table 7-4).
TABLE 7-4
Comparison of Nonabsorbable Suture
| Sutures | Materials | Construction |
| Pronova Poly | Polymer blend of poly (vinylidene fluoride) and poly (vinylidene fluoride-co-hexafluoropolypropylene) | Monofilament |
| Ethibond Excel polyester | Polyester/Dacron | Braided |
| Mersilene polyester suture | Polyester/Dacron | Braided |
| Ethilon nylon suture | Nylon 6 | Monofilament |
| Nurolon suture | Nylon 6 | Braided |
| Permahand silk suture | Silk | Braided |
| Prolene polypropylene suture | Polypropylene | Monofilament |
| Surgical stainless steel suture | 316L stainless steel | Monofilament |
| Vascufil | Butylenes terephthalate and polyteramethylene ether glycol | Monofilament |
| TiCron | Polyethylene terephthalate | Braided |
| Monosof Dermalon | Nylon 6 and nylon 6.6 | Monofilament |
| Surgilon | Nylon 6.6 | Braided |
| Silk | Silk | Braided |
| Surgipro II Surgipro | Polypropylene | Monofilament |
| Steel | 316L stainless steel | Stainless steel |
Modified from Ethicon product catalog, suture/adhesives, drains, hernia repair, 2009, available at www.akinglobal.com.tr/medikal/tr/dokumanlar/JHONSON&JHONSON/SUTURES.pdf. Accessed March 10, 2013; Covidien suture catalog 2013, available at www.covidien.com/campaigns/pagebuilder.aspx?topicID=181589&page=SPC:Main. Accessed March 10, 2013.
Silk.
Silk is prepared from thread spun by the silkworm larva while making its cocoon. Top-grade raw silk is (1) processed to remove natural waxes and gum, (2) manufactured into threads, and (3) colored with a vegetable dye. The strands of silk are twisted or braided to form the suture, which gives it high tensile strength and better handling qualities. Silk handles well, is soft, and forms secure knots.
Because of the capillarity of untreated silk, body fluid may transmit infection along the length of the suture strand. For this reason surgical silk is treated to eliminate its capillarity properties (able to resist the absorption of body fluids and moisture). It is available in sizes 9-0 to #5, in sterile packets or precut lengths, and with or without attached needles. Silk should be kept dry. Wet silk loses 20% of its original strength. Silk is not a true nonabsorbable material. When buried in tissue, it loses its tensile strength after about 1 year and may disappear after several years.
Cotton.
Surgical cotton sutures are made from individual cotton fibers that are combed, aligned, and twisted to form a finished strand. Because new types of fibers have been introduced, cotton suture is rarely used. Some companies no longer manufacture it.
Umbilical tape, although not used for suturing, is produced by suture manufacturers and packaged in the same way as suture. It consists of long woven ribbons of cotton,  to
to  inch wide, and is used for retraction or suspension of small structures and vessels. (Other soft, pliant products, such as vessel loops, are available and more commonly used for this purpose.)
inch wide, and is used for retraction or suspension of small structures and vessels. (Other soft, pliant products, such as vessel loops, are available and more commonly used for this purpose.)
Nylon.
Surgical nylon (Dermalon, Ethilon, Surgilon, Nurolon, Bralon, Monosof) is a synthetic polyamide material. It is available in two forms: multifilament (braided) and monofilament strands. Multifilament nylon is relatively inert in tissues and has a high tensile strength. It is used in conditions similar to those in which silk and cotton are used. Monofilament nylon is a smooth material that is particularly well suited for closing skin edges and for tension sutures. Because of its poor knot security, the surgeon usually ties three knots in small sutures and a double square knot in large sutures. It is used frequently in ophthalmology and microsurgery because it can be manufactured in fine sizes. Size 11-0 nylon is one of the smallest suture materials available.
Polyester Fiber.
Surgical polyester fiber (polyethylene terephthalate, polyester/Dacron) is available in two forms: an untreated polyester fiber suture and a polyester fiber suture that has been specifically coated or impregnated with a lubricant to allow smooth passage through the tissue. Polyester fiber is available in fine filaments that can be braided into various suture sizes to provide good handling properties.
Polybutester (Novafil) is a special type of polyester suture that possesses many of the advantages of polyester and polypropylene. Because it is a monofilament, it induces little tissue reaction.
Polyester material has many advantages over other braided, nonabsorbable sutures. It has greater tensile strength, minimal tissue reaction, and maximal visibility and does not absorb tissue fluids. It is used frequently as a general-closure fascia suture and in cardiovascular surgery for valve replacements, graft-to-tissue anastomoses, and revascularization procedures.
Polypropylene.
Polypropylene is a clear or pigmented polymer. This monofilament suture material (Prolene, Surgilene, Surgipro, Dermalene) is used for cardiovascular, general, and plastic surgery. Because polypropylene is a monofilament and is extremely inert in tissue, it may be used in the presence of infection. It has high tensile strength and causes minimal tissue reaction. Sizes range from 10-0 to #2.
Stainless Steel.
Surgical stainless steel is formulated to be compatible with stainless steel implants and prostheses. This formula, 316L (L for “low carbon”), ensures absence of toxic elements, optimal strength, flexibility, and uniform size. Monofilament and multifilament surgical stainless steel sutures are known for their strength, inert properties, and low tissue reaction. Stainless steel suturing technique is very exacting, however. Steel can pull or tear out of tissue, and necrosis can result from a suture that is too tight. Barbs on the end of steel can traumatize surrounding tissue or tear gloves. Torn or cut gloves fail to provide an adequate and effective barrier for the patient or the surgeon and assistant and can remain undetected. Kinks in the wire can render it practically useless. For this reason, packaging has played an important part in the development of surgical stainless steel sutures. Surgical stainless steel is available in packets on spools or in packages of straight, precut, sterile lengths, with or without attached needles. This packaging affords protection to the strands and delivery in straight, unkinked lengths.
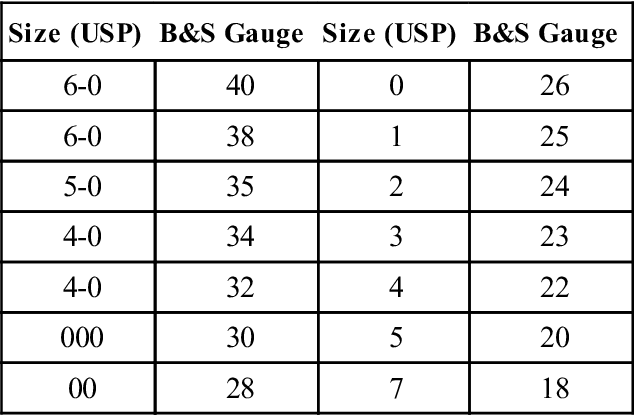
Before surgical stainless steel was available from suture manufacturers, it was purchased by weight with the Brown and Sharp (B&S) scale for diameter variations. Today the B&S gauge, along with USP size classifications, is used to distinguish diameter ranges. Table 7-5 compares steel suture sizes.
TABLE 7-5
| Size (USP) | B&S Gauge | Size (USP) | B&S Gauge |
| 6-0 | 40 | 0 | 26 |
| 6-0 | 38 | 1 | 25 |
| 5-0 | 35 | 2 | 24 |
| 4-0 | 34 | 3 | 23 |
| 4-0 | 32 | 4 | 22 |
| 000 | 30 | 5 | 20 |
| 00 | 28 | 7 | 18 |
Barbed Suture.
Barbed suture is a lesser known suture type. The suture has many small barbs cut into its monofilament core along its length, and is available in several absorbable and nonabsorbable polymers, including polydioxanone, PGA-PCL, and polypropylene. The barbs ensure that the suture stays in place and approximates the tissue without the need to tie knots, ensuring even distribution wound tension and decreased closure time. It is used extensively in plastic surgery and also has applications in other specialties as well such as orthopedics and general surgery (Lombardi et al, 2011) (Figure 7-2). If the suture breaks during suturing, the surgeon leaves it in place and begins again rather than removing it to prevent tissue damage.

Surgical Needles
Surgical needles vary in shape, size, point design, and wire diameter (Figure 7-3). Needle selection is determined by the type of tissue, suture material, and action to be performed. Surgical needles are made from stainless steel or carbon steel. Various metal alloys used in manufacturing surgical needles determine their basic characteristics. They must be strong, ductile, and able to withstand the stress imposed by tough tissue. Stainless steel is the most popular, not only because it provides these physical characteristics, but also because it is noncorrosive. The three basic parts of a surgical needle are the eye, the body, and the point or tip.
Eye
The eye of the surgical needle falls into the following three general categories:
1. Eyed needles, in which the needle must be threaded with the suture strand, and two strands of suture must be pulled through the tissue (Figure 7-4, A)
2. Spring, or French, eyed needles, in which the suture is placed or snapped through the spring (see Figure 7-4, B)
3. Eyeless needles, a needle-suture combination in which a needle is swaged (permanently attached) onto one or both ends of the suture material (see Figure 7-4, C)
The use of eyed needles has all but been eliminated in current surgical practice. The swaged needle is universally available and the preferred method of suture application. The swaged suture is a single strand of suture material that when drawn through the tissue is less traumatic to the tissue than is an eyed needle and suture. The swaged needle may need to be cut off with suture scissors or swaged for controlled release of the suture (semi-swaged), commonly referred to as a “pop off.” With semi-swaged suture, the needle remains attached until the surgeon releases it with a straight tug of the needle holder.
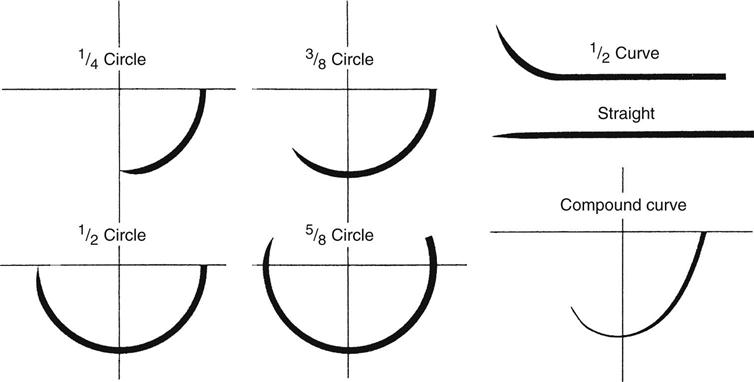
Body
The body, or shaft, of the needle may be round, triangular, or flattened. Surgical needles also may be straight or curved; the curve is described as part of an imaginary circle (see Figure 7-3). As the radius of the imaginary circle increases, the size of the needle also increases. The body of a round needle gradually tapers to a point.
Point
Taper needles, which are round with a point, are the most common needles used and are provided as swaged sutures in many sizes for both absorbable and nonabsorbable materials. Blunt needles are generally indicated for organ biopsy or repair and very delicate tissue that may be torn or injured when penetrated by a sharp needle. The cutting needle, which is round with sharp triangular edges at the objective end of the needle, is most often used for dense or tough tissues such skin closure, thick scar, or bone (Table 7-6).
TABLE 7-6
| Needle Type | Description of Body | Use |
| Taper point | Round shaft, straight or curved, taper point, no cutting edge | Soft tissue closure, such as gastrointestinal, fascial, vascular, and most soft tissues below skin surface |
| Penetrating point | Taper body with finely sharpened point; optimal penetration with less tissue wound | Ligaments, tendons, and calcified, fibrous, and cuticular tissue; mostly used for vascular, thoracic, plastic, obstetrics/gynecology, and orthopedic surgery; excellent penetration through synthetic grafts and scar tissue during repeat surgeries |
| Blunt point | Taper body with rounded point, no cutting edge | Friable tissue, fascia, liver, intestine, kidney, muscle, uterine cervix (note recommendations regarding use of blunt needles, p. 192) |
| Protect-point | Taper body with blunted point, no cutting edge | Primarily in fascia and mass closure to minimize potential of needlesticks |
| Reverse cutting | Triangular point with cutting edge on outer curvature | Skin closure; retention sutures; subcutaneous, ligamentous, or fibrous tissues |
| Cutting taper | Reverse-cutting tip with taper shaft | In microsurgery for excellent penetration through tough tissue, such as vasovasostomy, tuboplasty |
| Hand-honed reverse cutting | Same as reverse cutting but hand-honed for added sharpness | Primarily in plastic surgery for delicate work and where good cosmetic result is priority |
| Spatula side cutting | Two cutting edges in horizontal plane | Ophthalmic surgery for muscle and retinal repair; also for delicate eyelid or plastic surgery; cutting edges “ride” along scleral layers |
| Regular cutting | Triangular point with cutting edge on outer curvature | General skin closure, subcutaneous tissue; sometimes for ophthalmic surgery, plastic, or reconstructive surgery |
| Lancet, inverted lancet | Spatula needle with cutting edge (lancet) or outer (inverted lancet) curvature | Ophthalmic surgery and microsurgery |
Modified from Ethicon product catalog, suture/adhesives, drains, hernia repair, 2009, Available at www.akinglobal.com.tr/medikal/tr/dokumanlar/JHONSON&JHONSON/SUTURES.pdf. Accessed March 10, 2013.
Available blunt protect-point needles have been recommended as an alternative to taper point needles. Interest in blunt needles has evolved because of the risk of bloodborne exposure from percutaneous injuries (PIs).
The use of blunt needles represents a key strategy to reduce risk to the surgical team. Blunt needles are associated with a statistically significant reduction in PIs and can be substituted for conventional curved needles in a variety of surgical procedures.
Triangular needles have cutting edges along three sides. The cutting action may be conventional or reverse. The cutting edge of the conventional cutting needle is directed along the inner curve of the needle, facing the wound edge when suturing is performed.
The reverse cutting needle is preferred for cutaneous suturing. When it transects the skin lateral to the wound, the outside cutting edge is pointed away from the wound edge, and the inside flat edge is parallel to the edge of the wound. This cutting action reduces the tendency for suture to tear through tissue.
For certain types of delicate surgery, needles with exceptionally sharp points and cutting edges are used. Microsurgery, ophthalmic surgery, and plastic surgery require needles of this type; special honing wheels provide needles of precision-point quality for surgery in these specialties. In some instances the application of a microthin layer of plastic to the needle surface provides for easier penetration and reduces drag of the needle through tissue.
Suture Packaging, Storage, and Selection
Types of Packaging
For packaging, the suture material is sealed in a primary inner packet, which may or may not contain fluid; placed inside a dry outer peel-back packet; and sterilized. This method permits easy dispensing onto the sterile field. Various forms of foil, plastic, and special paper are used for the inner and outer packets.
Each primary suture packet is self-contained, and its sterility for each patient is ensured as long as the integrity of the packet is maintained. Some suture packets have expiration dates that relate to stability and sterility. Packages should be stored in moisture-proof and dust-proof containers in units of one size and type.
Suture without needles are packaged as multiple strands and in reels for delivery as free ties. Suture with swaged needles can be packaged as single stitches or as multipacks containing several of the same sutures commonly used for the planned procedure. Multipacks may be permanently swaged needles that require being cut for tying or control-release (pop-off) for easy needle detachment. Some sutures may be double-armed, with a needle at each end of the strand. Double-armed sutures are most commonly used for vascular procedures such as anastomoses and vessel repairs.
Color Codes.
Color-coded packaging based on suture fiber is used by most companies to make identification quicker and easier. Each individual packet is color-coded, as is the dispenser box. Although most color codes are universal across companies, there are some exceptions. Ethibond, a coated polyester, is coded orange, whereas most polyesters are coded in shades of green. Dexon, a glycolic acid polymer, is gold, whereas Vicryl, a comparable polymer, is violet.
Suture Selection
The choice of suture material, size, needle, and type depends on the procedure, the tissue being sutured and type of reapproximation required by the general condition of the patient, and the surgeon’s preferences. A surgical services committee or project team may be responsible for establishing standard suture uses for various operations. Current guides published by suture manufacturers should be consulted. These guides list the specific suture materials recommended for various wounds and are based on current clinical practice and research. Although the perioperative nurse is not responsible for choosing the suture material used, he or she must be knowledgeable of the suture properties to ensure the best possible outcome for the surgical patient.
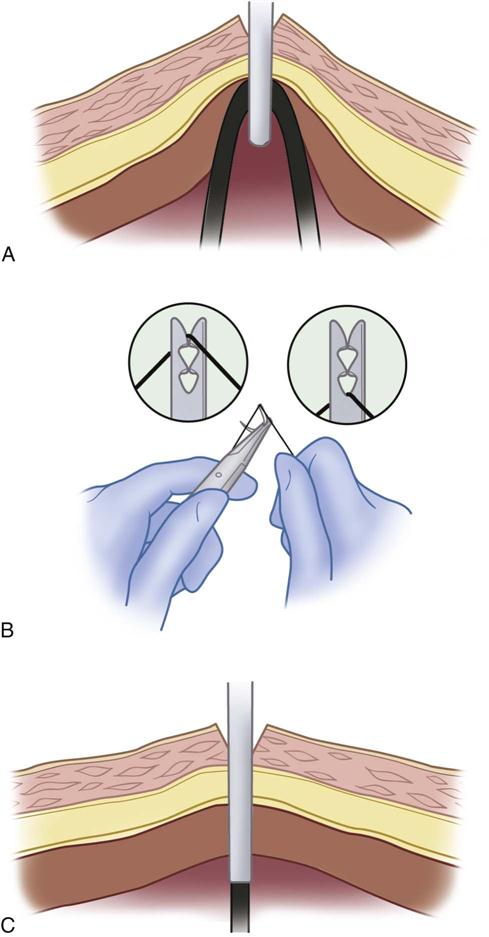
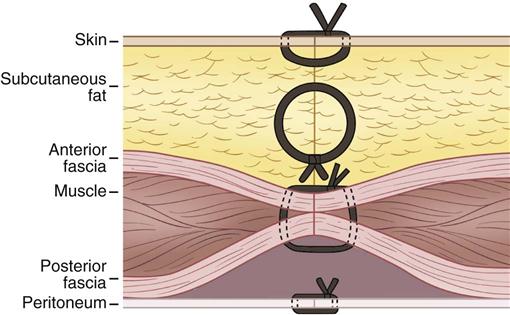
Suturing Techniques/Wound Closures
Surgeons may use suture or other devices to accomplish wound closure. The primary suture line refers to sutures that obliterate dead space, prevent serum from accumulating in the wound, and hold the wound edges in approximation until healing takes place (Figure 7-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree