In the previous chapters we have considered the nuts and bolts of epidemiology. In this and the next few chapters we move on to look at how epidemiology is used in practice to improve public health. We start with ‘surveillance’ as, without the ability to gather timely information on emerging and changing health problems, public health can be paralysed or, at best, inefficient. In this chapter we discuss the design and use of surveillance systems that allow health officials to detect new risks and diseases such as Ebola promptly, track known diseases and generate data needed for effective health planning and resource allocation.
The scope of surveillance
Surveillance is a cornerstone of public health activities as it provides data and intelligence for development of policy, disease prevention programmes, estimation of disease burden, detection of outbreaks and applied research. It was originally applied primarily to infectious diseases, and we will mainly discuss surveillance in this context, but the approach, principles and practice have broadened to include chronic diseases, injuries, health system outcomes, risk factors and even potential hazards to human health. Surveillance is defined as the: ‘systematic and continuous collection, analysis, and interpretation of data, closely integrated with the timely and coherent dissemination of the results and assessment to those who have the right to know so that action can be taken’ (Porta, 2014). Ultimately, these data should be used to inform public health interventions and action to prevent human illness. The emphasis of this definition, and the feature that separates surveillance from the collection of data for monitoring purposes, is the dissemination of data for the purposes of public health action.
A good example of the importance of public health surveillance comes from the Ebola virus disease epidemic in West Africa in 2014–2015 – a crisis in international health (Box 12.1). The Ebola virus is spread by close contact with an infected person during the symptomatic phase of their illness, or contact with the body of someone who died from the disease. In the outbreak in West Africa, the international community focussed on controlling the outbreak rapidly, supported by establishment of surveillance for possible Ebola infections. This surveillance was critical to determine when disease activity had declined in a given regional area (WHO Ebola Response Team, 2014).
Detection of the primary event: In March 2014, Guinea reported an outbreak of febrile illness among 49 people with a high case fatality rate (59%); it was later confirmed as Ebola virus. Epidemiological investigation of the reports identified that the primary case was likely to have been a two-year-old child who died in December 2013 (Baize et al., 2014).
International response: The international response to the outbreak initially seemed effective, but cases continued to spread in Guinea and to neighbouring countries, leading to Médecins Sans Frontières declaring that the outbreak was ‘out of control’ in June 2014. The World Health Organization (WHO) published a roadmap to control in August 2014 (WHO, 2014) and declared the outbreak a ‘Public Health Emergency of International Concern’.
Controlling the outbreak: With support from international partner organisations, affected countries established programmes to identify cases, deaths and those who had been in contact with them. This required investigative teams to travel from house to house in very remote areas to track down contacts. The resulting information was entered into specialised databases and communicated through regional and country offices to WHO. The data were discussed at daily meetings and used to identify areas of high risk and those where the infection had been cleared. This ‘surveillance’ was vital for detecting new cases and outbreaks and for monitoring spread of infections to neighbouring countries.
Preparedness of unaffected countries: Despite the challenges, the WHO Africa region now advocates integrated surveillance of disease and, in response to this outbreak, international agencies have assisted neighbouring countries to strengthen their surveillance and control activities (WHO Ebola Response Team, 2014).
Epidemiology has a fundamental role in public health surveillance:
epidemiology provides the tools to guide data collection, collation and analysis;
the concepts of rates of infection and analysis by subpopulations are key to analysis of surveillance data;
epidemiology provides a systematic framework for assessing potential biases that are inherent in surveillance data; and
surveillance provides much of the data essential to descriptive epidemiology (see Chapter 3).
Why conduct surveillance?
Public health surveillance provides information on the changing nature of diseases in populations and, ideally, there is a clear link between the surveillance system outputs and control programmes or interventions, such as introduction of a vaccine or health promotion campaign. There are several reasons why it is important to conduct surveillance:
To inform public health policy. For some diseases, such as influenza, information arising from surveillance of circulating strains in one hemisphere is used to inform decisions about vaccine composition for the next influenza season in the other hemisphere.
To detect clusters or outbreaks. Diseases that are prone to occurring in clusters or outbreaks require surveillance to allow timely and effective investigation to identify a source. We will discuss this further in Chapter 13.
To monitor the effect of interventions. Public health and other agencies may institute control measures that should reduce the incidence and prevalence of diseases; the effects of these can be observed in disease-specific surveillance data.
To monitor the introduction of new pharmaceutical drugs. New drugs are often licensed before long-term safety data are available. Electronic databases now make it much simpler to link prescribing and health databases to identify unexpected safety concerns more rapidly than before.
To quantify the burden of disease. Surveillance data can be critical to identifying the effects that diseases have on affected populations in terms of cases, hospitalisation, disability and deaths.
To support disease elimination and eradication. Multiple modes of surveillance play a critical role during the phases of elimination and eradication of a disease (e.g. during the eradication of smallpox, see Box 1.5) and surveillance efforts are intensive due to the need to have highly sensitive systems for detecting cases.
Surveillance can provide dynamic data on population risks, morbidity and mortality – all key indicators for epidemiological intelligence on community health. However, given the limited resources of public health, it is important that only conditions of public health importance are considered for surveillance. Public health importance may be defined by a range of factors (we will discuss these further below) that should be well articulated before a condition is put under surveillance.
Surveillance essentials
To understand the basics of surveillance, we need to consider the exposure–disease–diagnosis pathway as this influences whether cases progress from exposure through to reporting to a surveillance system. Firstly, a person must be exposed to a hazard, such as another infectious person, and there will then be a latency or incubation period that depends on the agent. In some instances, there may be some other necessary cause, such as prior exposure to antibiotics or a comorbid illness, that will potentiate or result in the person moving on to develop disease. There are then other factors that predict whether a diseased person goes on to seek diagnosis and medical treatment. These include the proportion of people who develop symptoms, the severity of the major signs and symptoms and how communicable the disease is. Finally, for a case to be reported to a surveillance system, the health care provider making the diagnosis must recognise that it fits the criteria (whether these are specific tests for a clearly defined condition or the more general characteristics of a disease syndrome) for a reportable condition.
The steps in this pathway highlight many important criteria of surveillance, including timeliness of the data, the sensitivity of the system to detect a case, the representativeness of cases that are reported and, ultimately, the cost of the system. The key steps in surveillance are (1) collection of data, (2) collation and cleaning of data, (3) analysis and interpretation and (4) dissemination of data to those who can take action and, importantly, back to those who provided the data. Surveillance systems should have well-defined aims and objectives that are clearly communicated to stakeholders for surveillance to be successful.
It is likely that only a proportion of people with the disease under surveillance will present to a health care recorder, be tested and test positive for the disease in question. This is equivalent to the ‘sensitivity’ of the system (we will discuss this further in Chapter 15) and is the complement of ‘undercount’, the proportion of those with disease who are not counted. For diseases where some people may experience mild symptoms and not present for medical attention, such as Salmonella infections, the undercount may be substantial. In contrast, for a condition with a severe outcome, such as meningococcal meningitis where most of those affected are very ill and present to a hospital, there may only be a small degree of undercount inherent in surveillance. A system with low sensitivity may be acceptable if there is still a reasonable probability of identifying outbreaks. Undercount in surveillance is typically represented by a pyramid showing loss of cases through the system. Figure 12.1 shows the reporting pyramid for surveillance of a disease transmitted by contaminated foods where a person must visit a doctor and submit a specimen for testing in order to be counted as a case.
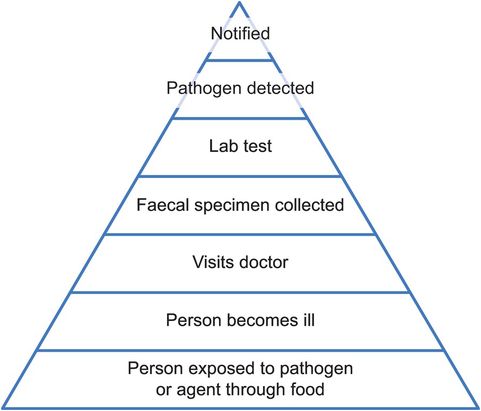
The surveillance pyramid for gastrointestinal illnesses.
Health care recorders are those who provide reports of cases or other details about disease. They include physicians in community clinics or microbiologists in a laboratory.
In the USA an estimated 29 Salmonella infections – a common cause of foodborne disease – occur in the community for every one that is reported to surveillance (Scallan et al., 2011).
Depending on the nature of the disease and the aims of surveillance, the response to a single case will be different. For many diseases, health departments do not follow up all cases. However, they may interview all cases of diseases with epidemic potential, if there is a planned evaluation of an intervention or where there is a requirement to provide prophylaxis. For example, the incidence and burden of hepatitis A has declined globally due to improvements in sanitation and hygiene (Franco et al., 2012). It is routine for health department staff to contact and interview all cases of hepatitis A in high-income countries to determine if there is a need to offer hepatitis A immunoglobulin (prophylactic vaccination) to contacts, and to use their exposure histories to identify links between cases that might indicate an outbreak is occurring.
Defining a case for surveillance purposes
All forms of surveillance rely on some form of case definition which specifies elements of person, place and time. The case definition may be syndromic in nature and specify clinical signs and symptoms, or it may be more specific and require particular pathology, but it is important to recognise that what defines a case for surveillance purposes may differ from what a doctor might use to diagnose a condition in a patient. This is particularly true for surveillance during outbreak settings when there may be multiple case definitions representing greater degrees of certainty about whether a patient is a true case or not.
Where a case definition is based on a syndrome, it is called ‘syndromic surveillance’. Syndromic surveillance can be much more sensitive as it picks up cases of illness that may be due to many different disease-causing agents, but it may not be very specific and may consequently be less useful for public health action. Syndromic surveillance is very useful for diseases where there is a need for a sensitive indicator of disease activity. Box 12.3 shows an example of this with surveillance for acute flaccid paralysis (AFP) – the syndrome potentially signalling the presence of cases of poliovirus in a community (Porter et al., 2015).
By 2001, polio had largely been limited to two states in India with only 268 new cases that year, but in 2002 there was a resurgence with 1600 new cases. In 2003, a network of 248 medical officers trained in surveillance assisted Indian health authorities with surveillance for acute flaccid paralysis (AFP), the critical clinical marker of polio. The WHO criteria for assessing the quality of polio surveillance require that
non-polio AFP should be detected at a rate of ≥1 per 100,000 in the population aged <15 years (to ensure that ‘background’ AFP cases are being detected at a level showing the detection system is working) and
adequate stool specimens are collected from ≥80% of people with AFP for polio diagnosis.
India had been meeting these criteria since 2000, but in 2003 the non-polio AFP rate was <1/100,000 in seven small states and stool specimens were inadequate in 11 states covering one-third of India’s population. Investigation showed that during 2002, the proportion of infants aged <1 year who received three or more routine doses of oral poliovirus vaccine had fallen to only 21% in some states. Vaccination rates increased again in 2003 and only 225 wild poliovirus cases were reported that year (Anonymous, 2004). In February 2012, India was finally removed from the list of polio-endemic countries. This list now includes only six countries in the Eastern Mediterranean Region including Afghanistan and Iraq, and 23 African countries. Of these, all six Eastern Mediterranean countries but only 15 of the African countries (down from 20 in 2013) met both surveillance quality indicators in 2014 (Porter et al., 2015).
Collection of surveillance data
Data collection for surveillance relies on a combination of reports on paper or electronically from recorders and supplementary information obtained from interviews of case patients or next of kin. In low-resource settings, novel data collection strategies can be useful, such as short-messaging system (SMS) reporting of syndromic surveillance data via mobile phone to a central system (Box 12.4).

In Papua New Guinea, mobile phones were trialled for surveillance of syndromes such as haemorrhagic fever, bloody diarrhoea, AFP and acute watery diarrhoea, which may indicate the occurrence of important illnesses of national and international significance. The objectives of the system were to rapidly identify outbreaks of illness and provide confirmation of events to complement other surveillance. The system was piloted in several sites where health workers in provinces sent weekly text messages to the central coordinating unit in the national Department of Health. The text messages reported the numbers of cases of different syndromes. For urgent conditions reports were sent immediately, and this proved very effective at identifying cases of AFP and dengue haemorrhagic fever. The pilot system was more timely, complete and sensitive than reporting through existing systems although it required development of software and a secure online database, along with the costs associated with preparation of investigational materials, mobile phones and field missions (Rosewell et al., 2013).
 Public-domain epidemiology software
Public-domain epidemiology software
Surveillance data are entered or captured into computer-based databases which are usually built for this purpose. Simple databases for surveillance can be developed quickly and cheaply using free public-domain software and agencies have developed specific systems for certain diseases, such as those caused by organisms resistant to antibiotics. However, these databases may not be sufficient for sophisticated systems housing millions of records of data, and health agencies often commission the development of expensive systems for collecting and managing data.
Surveillance is commonly described in terms of whether managers of surveillance actively seek reports from recorders (‘active surveillance’) or wait for them to be sent in (‘passive surveillance’). Many traditional notifiable disease systems are passive in that health departments do not actively seek reports from doctors or laboratories. This is in contrast to what may occur in an outbreak of a new infection. Active surveillance, such as that used for Ebola in Box 12.1, is based on specific collection of data from health care providers or institutions, both as a need arises and in the longer term. Active surveillance can produce more complete data of better quality than that provided by other systems. However, it is resource-intensive to maintain, especially to produce timely output of information. It is used, for example, during outbreaks of foodborne illness or measles when health care providers may be contacted and asked to provide details of any possible cases they have seen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



