Learning Objectives
- Define global surgery
- Describe the history of surgical care and issues in international health
- Describe the global burden of surgical disease including its impact on noncommunicable diseases and other disease control programs
- Discuss surgical capacity building as part of global health initiatives in resource-constrained environments
Introduction
Today 84% of the world’s population lives in developing countries where 93% of the world’s disease burden exists but only 11% of global health research dollars are spent.1 Although deaths in developing countries from communicable diseases such as tuberculosis (TB), malaria, and HIV/AIDS are slowly decreasing, the prevalence of noncommunicable diseases (NCDs) such as cancer, diabetes, cardiovascular disease, and chronic respiratory disease are steadily rising. With the urbanization of towns and cities in developing countries, traffic crashes and injuries have become more common place. A high baseline prevalence of communicable diseases, along with rising rates of NCDs and injuries, will create inordinate future health system demands and may impede overall progress on the Millennium Development Goals (MDGs). Many of these diseases require surgical treatment to save lives, decrease suffering, and prevent or end disability to restore health and livelihoods. At present, access to complete surgical care in most developing countries is not readily available.
The Alma-Ata Declaration of 1978 identified primary health care as the cornerstone to achieving “health for all.” This historic document highlighted the gross inequities in health and access to care between people living in developed and developing countries. Although the Alma-Ata Declaration strongly supports primary care for all, it also “addresses the main health problems in the community, providing promotive, preventive, curative and rehabilitative services.” Appropriate, cost-effective curative and rehabilitative surgical interventions are secondary and tertiary preventive services and a necessary response to diseases that elude primary prevention.2
The volume of major surgeries performed worldwide is estimated to be between 187.2 million and 281.2 million procedures per year. A total of 73.6% of these surgeries occur in high-income countries and 22.9% in countries in transition, and only 3.5% take place in developing countries where most of the world’s population lives.3,4 The imbalance in the numbers of operations performed per capita in developed countries versus developing countries is due largely to the lack of available surgical care in these resource-challenged nations.
- Define global surgery.*
- Present a historic overview of surgical issues in international health.
- Describe the global burden of surgical disease, including its impact on NCDs and other disease control programs.
- Discuss surgical capacity building as part of global health initiatives in resource-constrained environments.
- Discuss ways in which surgical providers can become integrated with global public health.
The word surgery is an Anglicized derivation of the Latin word chirurgia, meaning “hand work.” A surgeon is any health provider who treats surgical conditions through manipulation of tissues and provides invasive measures such as incisions and punctures with the intent to cure disease. Surgical care is not always invasive, and in some cases surgeons attend to a patient without performing an operation as in the treatment of splenic or liver injuries, fractures, and closed head injuries. Although an operation may not be performed in some of these cases, surgical expertise is needed. Surgery can be performed by a range of providers, including physicians with formal specialty training in surgical care and techniques, general practitioners with limited training in surgical care and techniques, and nonphysician health care providers who have had focused training in certain surgical techniques. In resource-constrained environments such as sub-Saharan Africa, many surgical and anesthetic services are limited to those provided by general practitioners or nonphysician health care providers. For the purposes of this discussion, surgeon refers to any physician with formal training in surgical care and techniques unless otherwise indicated.
International surgery, also referred to as global surgery,† is often represented as a humanitarian branch of medicine concerned with post disaster emergency care and with elective treatment of congenital anomalies such as cleft lip and palate, cardiac birth defects, and musculoskeletal deformities.5 This work depends not only on the voluntary participation of trained specialists but also on the cooperation and understanding between donor and recipient nations. International surgery programs increasingly include education, research, capacity development, philanthropy, and advocacy. In addition, these programs include the delivery of anesthetic services, obstetric care, nursing care, and postoperative rehabilitative care. Global surgery fosters cooperation and understanding between nations. It includes north-to-south and south-to-north learning as well as south-to-south collaborations. It focuses on vulnerable populations even in high-income countries. One of the most notable deployments of international humanitarian surgical aid took place in 2010 in response to the earthquake in Haiti. Medical teams from all over the world descended on Haiti to treat the injured. Shortly after the earthquake, Médecins Sans Frontières (MSF) dispatched the largest nonconflict surgical team in its history, treating over 550,000 Haitian patients and performing more than 4,000 surgical interventions in 10 weeks.6 Although a high-profile disaster such as the Haiti earthquake is seen by many as humanitarian surgical care, it is the day-to-day surgical care needed in developing countries that is the true “disaster.”
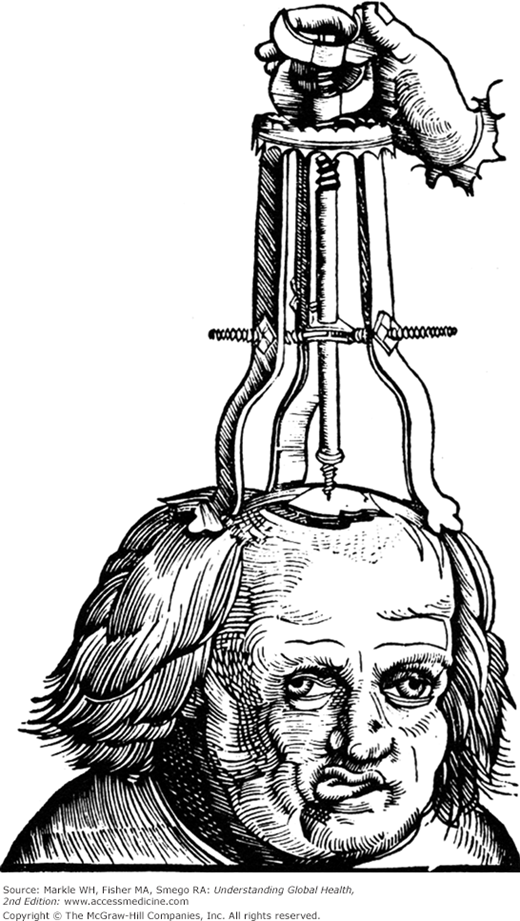
Surgical treatment dates back to as early as 10,000 to 5,000 bc. Early medical providers were known as healers, shamans, priests, barbers, and medicine men. Originally all medical providers were essentially surgeons as they treated wounds, drained infections, set broken bones, and stopped bleeding by applying hot metal or hot oil to wounds. Some of the oldest surgical procedures included the closure of lacerations using suture made of tendons threaded through needles made of sharpened bone. Trepanation, the act of drilling openings into the skull to release so-called evil spirits from the body dates back to the Mesolithic period (Figure 14-1).7 Hieroglyphics in ancient Egypt and textbooks that were the foundation of Ayurvedic medicine (the Sushruta Samhita) describe many operations, including cesarean deliveries, rhinoplasty, craniotomy, and laparotomy performed while using wine and Cannabis indica as anesthetic agents.8
Wars and conquests throughout history have taken soldiers and their field surgeons to foreign lands, and care of battlefield injuries has provided surgery with some of its greatest technical advances as a result of working in very difficult field environments. These advances include improvements in anesthesia, in transportation and care of the injured, in achieving hemostasis and in treating sepsis. John Snow, the father of public health, also assisted in the development of surgical anesthesia as we know it today. Snow, well known for his epidemiologic work identifying the Broad Street pump handle as the source for London’s 1854 cholera outbreak, was also an anesthetist and an advocate for the use of inhalation anesthesia during difficult childbirth.9
Colonial expansion brought surgical treatment to parts of the new world. As European colonialists, slave traders, and pirates moved throughout the Caribbean, Americas, and Pacific regions, they brought with them communicable diseases that would devastate native populations. In addition, they had new opportunities to understand tropical illnesses and apply medical and surgical treatments to a host of new maladies. Over time missionary physicians and surgeons were employed to keep the colonialists healthy and to assure the health of local human assets that were needed to sustain colonial economies.10 They built, supported, and staffed hospitals in some of the most challenging locations. In addition to the Caribbean, Americas, and Pacific regions, colonialism in Africa fostered development of the Colonial Medical Service with training and research conducted at the London School of Tropical Medicine and Hygiene and other institutions. Medical and surgical teaching programs were established throughout the continent with early training programs flourishing in Sierra Leone, Nigeria, and Uganda.11
Early support for international medical and surgical education and public health training also came from the Rockefeller Foundation’s International Health Board, the World Bank, the Pasteur Institute, and the World Health Organization (WHO). However, years of political and civil unrest in many of these sub-Saharan African countries left what were once grand academic medical institutions in disarray, and surgical services deteriorated as a result of deficient infrastructure and support. Médecins Sans Frontières (MSF), established in 1971 by a small group of French doctors in response to the Biafra crisis, filled a health care void created by war. MSF quickly added surgical services in 1983 after seeing the need for field operating theaters manned by expatriate surgeons who provided treatment for refugees from Chad and Liberia’s wars. In a short period of time, MSF became one of the largest, most respected providers of international medical and surgical care in areas of civil unrest and natural disasters as well as in areas of nonconflict. Today MSF works in over 70 countries providing medical care, including general surgery, orthopedic surgery, obstetric emergency procedures, and surgical care for the injured.12 The organization also advocates vigorously for human rights and health equity.
In the 1990s, investment in surgical service development in developing countries was minimized. In the World Bank’s 1993 World Development Report, “Investment in Health,” the Bank recommended governments in developing countries invest more heavily in “cost-effective programs that help the poor” through prevention rather than in direct medical care services.13 The report emphasized the prevention and treatment of communicable diseases, including HIV/AIDs, malaria, and TB, all of which represented the most significant burdens of disease among developing countries. This report, authored along with the WHO, was very influential in defining the direction global health has taken today. Shortly after its release, a cascade of private health-directed philanthropy began. In 1999, Bill and Melinda Gates established the Gates Foundation, which stimulated an unprecedented effort to address specific diseases such as TB, HIV/AIDs, and malaria. In 2001, the MDGs were established and included mandates to reduce maternal and child mortality. The Global Fund to fight AIDs, Tuberculosis, and Malaria (GFATM) followed in 2002, and in 2003 the US Congress approved the establishment of the President’s Emergency Plan for AIDs Relief (PEPFAR), which has committed over $63 billion to date, making it the largest health initiative addressing a single disease in US history. NCDs and injuries, neglected tropical diseases (NTDs), as well as health system strengthening, were not addressed in this global development agenda. The development of surgical services was not included as a goal of this unprecedented philanthropy because these services were perceived to be too expensive and therefore not cost effective. 20 years after the 1993 World Bank Report made the statement “Public money is spent on health interventions of low cost-effectiveness, such as surgeries for most cancers, at the same time that critical and highly cost-effective interventions such as treatment of TB or STDs remain underfunded,”13 the mortality rates from cancers, injuries, and other NCDs in developing countries are increasing at alarming rates and the need for surgical interventions and horizontal health development programs has been recognized. Prevention strategies for these diseases include early detection and treatment as well as palliative care to relieve suffering. All of these can be accomplished through the addition of appropriate surgical services.
For years, teams made up of volunteer surgeons, operating room nurses, and technicians from developed countries have provided surgical care in many developing countries. Short duration surgical subspecialty groups like Operation Smile, Smile Train, Operation Hernia, Cure International, Orbis, and Children’s Heartlink have filled the void of specialty surgical care for children living in developing countries who have cleft lip and palate, hernias, life-threatening congenital cardiac anomalies as well as other congenital musculoskeletal defects. Both military and civilian surgeons have been involved in international responses to natural disasters and wars such as Haiti, Banda Aceh, and conflicts in the Middle East and the Horn of Africa.14 Even in conflict situations, more than 50% of the surgeries performed are for routine, nonviolent, usually obstetric or infectious problems, illustrating that even during war the need for general surgical care is great.15,16
The number of short surgical missions conducted in developing countries has grown over the past decade. These “outreach” or “mission visits” provide a valuable service, but many lack sustainability. The 2006 WHO Work Force Report recognized that these efforts were necessary until the local workforce improved. Nonetheless, concerns have been expressed over the quality, safety, appropriateness, and motives of these types of surgical missions.17–20 Coordination of volunteer surgical outreaches with local providers, hospitals, and Ministries of Health is necessary to reduce duplication of efforts and burden on local staff. Follow-up care should also be planned in advance. The cost of conducting these short duration surgical missions is as difficult to estimate as is the total number of operations they provide. Maki et al conservatively estimated well over $250 million per year is spent on sending teams to provide care in developing countries.21
Programs such as the Pan-African Academy of Christian Surgeons (PAACS), established in 1997, and the Royal College of Surgeons of England have begun to address workforce shortage issues by committing to full time, in-country, primary surgical training programs in Gabon, Ethiopia, Cameroon, and Kenya.22,23 Many universities based in developed countries such as Johns Hopkins, Duke, University of California San Diego, University of California San Francisco, University of Michigan, University of Virginia, McMaster, and University of British Columbia have established academic exchanges with universities in sub-Saharan Africa, Latin America, and the Middle East to strengthen the surgical capacity of these regions through education and research.24 Integration of academic surgical training along with outreach surgical care allows coordinated programs to create sustainable solutions while delivering much needed surgical services.
In 2005, as interest in surgical care strengthening grew, the WHO responded by establishing the Global Initiative on Emergency and Essential Surgical Care (GIEESC).25 WHO GIEESC’s mission is to create guidelines for member Ministries of Health to use in order to reduce death and disability from road traffic accidents, trauma, burns, injuries, pregnancy-related complications, domestic violence, disasters, and other surgical conditions in low-and middle-income countries. Manuals and workshops for training doctors and nonphysician surgeons in safe emergency surgical care and how to outfit rural hospitals with the minimum equipment needed to do so are available. Over the past 8 years, WHO GIEESC has grown and now includes input from over 400 surgeons working in more than 60 countries. Annual international surgery meetings such as the Alliance for Surgical and Anesthesia Presence (ASAP), the Bethune Round Table, and the Center for Global Surgery’s Extreme Affordability Conference address issues pertinent to surgical capacity building and the surgical burden of disease. Professional organizations such as the American College of Surgeons’ Operation Giving Back, the Royal Australasian College of Surgeons’ International Program, Global Partners in Anesthesia and Surgery, and the Society of International Humanitarian Surgeons provide avenues for advocacy, information, research, volunteer opportunities, and education (Table 14-1).
World Health Organization Global Initiative for Emergency and Essential Surgical Care (WHO GIEESC) |
Bellagio Essential Surgery Group |
American College of Surgeons Operation Giving Back |
Surgeons Over OverSeas |
Alliance for Surgical and Anesthesia Presence |
Global Partners in Anesthesia and Surgery |
Pan-African Academy of Christian Surgeons (PAACS) |
Canadian Network for International Surgeons |
Royal Australian College of Surgeons International Program |
In 2009, the US Global Health Initiative (GHI) expanded its portfolio of aid beyond disease specific acute care to include more sustainable aid by health system strengthening and the development of human resources for heath (HRH). Much of this work is funded through the National Institute of Health’s (NIH) Medical Education Partnership Initiative (MEPI) grants. In addition to medical and public health education and training, MEPI grants support surgical education and research. Two MEPI grants were recently awarded to surgical capacity building programs in Mozambique and Rwanda.
Despite all of this initial work and a movement toward sustainable surgical capacity development, there are still significant challenges to the delivery of surgical care in resource-constrained environments. Further efforts are needed in defining the enormous unmet surgical need in developing countries, its economic impact, as well as prospective studies that evaluate surgical capacity building programs.
*In this chapter the term international surgery is used to describe broadly the delivery of surgical care. This care includes the delivery of anesthesia, obstetrics, and surgical nursing.
†The use of the term global surgery links the integration of surgical interventions, humanitarian aid, and the education and training of surgical workforces into global health strategies. Global health is a multidisciplinary strategy with the priority of improving health through training of health care workforces, incorporation of social justice, development fostering health care solutions as well as population-based prevention. International or global surgery is one of the disciplines that constitute global health.
Burden of Surgical Disease
Describing the global burden of surgical need is important because a detailed analysis allows for measurement of frequency of disease (incidence and prevalence); its severity (mortality and disability); its consequence on populations (health, social, and economic impacts), and who is most affected (age, gender, socioeconomic position, region). This information assists with prioritization of strategies yielding the greatest benefit, identifying emerging trends, establishing spending priorities, and assisting in setting global health research agendas. In 1991, the World Bank commissioned the Global Burden of Disease Study (GBD) to quantify the burden of disease using mortality, disability, risk factors, and disease prevalence data projection by age, gender, and geographic region from 2000 to 2020. Diseases were classified into three broad groups based on the WHO ICD classification system (Table 14-2). Murray and Lopez published the first reports estimating the global burden of disease26 with updates by the WHO in 2010. The Global Burden of Disease, Injury and Risk Factors 2010 Study, conducted by the Institute for Health Metrics and Evaluation, is the most comprehensive evaluation of disease burden to date. It includes analysis of more than 220 conditions and injuries, over 40 risk factors, and over 230 nonfatal health condition sequelae in 21 regions of the world. While death rates from infectious diseases such as malaria, AIDS, and TB are decreasing, there has been a steady rise in chronic diseases such as diabetes, cancer, and cardiovascular disease as well as injuries. Hospital bed occupancies in developing countries are shifting from patients with predominantly infectious diseases to patients with diabetic complications, cardiovascular disease, cancers, and those debilitated by injuries such as femur fractures. This disease burden transition is due largely to population aging, reduced childhood mortality, and control of some communicable diseases. It is also the result of globalization and urbanization with behavior shifts toward poor diets, cigarette smoking, and decreased levels of activity. The prevalence of NCDs is expected to rise by more than 40% by 2030 and will account for an estimated 70% of deaths and 57% of disability-adjusted life years (DALYs) worldwide. Developing countries will be most dramatically impacted by increasing NCDs. Rates of injuries in developing countries are also increasing as these countries undergo urbanization, and traffic and factory production increase. Mortality, morbidity, and disability data collected by the GBD Study are the best estimates of the burden of disease, and they take into account the available sources of information in a country or region while correcting for bias. See Chapter 2 for more information on the burden of disease and Chapter 13 for information about injuries.
Group 1: Infectious communicable diseases, perinatal, maternal, and nutritional disorders. |
Group 2: Noncommunicable diseases: neoplasms, diabetes, cardiovascular disease, pulmonary, congenital anomalies, and psychiatric disorders. |
Group 3: Intentional and unintentional injuries and violence. |
The prevalence of surgical conditions is not known. Many of the disease conditions described in the Global Burden of Disease Study analysis are amenable to surgical interventions if care is available, but many surgical conditions such as intestinal obstruction, gallbladder disease, appendicitis, and hernias are not included in the GBD data. Table 14-3 lists the medical conditions that would benefit from surgical intervention. The burden of surgical conditions (BoSC) is defined as disability, death, or illness that is wholly or partially curable by surgical intervention, and it includes all causes of surgical conditions. The BoSC, like the GBD, is expressed as DALYs. (See Chapter 2 for an explanation of the DALY.) The DALY measures mortality due to disease states as well as associated disability.
Disorder | Surgical treatment |
|---|---|
| NCDs | |
Cancers: breast, cervical, colon, gastric, lung | Resection for cure, bypass for palliation |
Chronic lung disease: asthma, COPD, emphysema | Lung volume reduction |
Cardiovascular disease: acquired and congenital | Valve replacement, angioplasty |
Diabetes: wound infections, limb loss, retinopathy | Debridement, amputation, laser retinal surgery, dialysis access |
Thyroid masses due to iodine deficiency | Thyroidectomy |
Communicable and NTDs | |
Trachoma, Filariasis, Buruli ulcers | Excision, skin grafts, skin flaps, tarsal flap rotation |
Ascariasis, induced bowel obstructions | Exploratory surgery, bowel resection, enterectomy |
Tuberculosis: Pulmonary TB | Lung resection, decortication, plumage, thoracoplasty |
Abdominal TB | Exploratory laparotomy, bowel resection or bypass |
Potts disease (spine) | Debridement, fixation, rodding |
Malaria: hypersplenism and spontaneous rupture | Splenectomy |
Millennium Development Goals 4 and 5 | |
Ectopic pregnancy | Salpingectomy, salpingostomy |
Dystocia, cephalopelvic disproportion, fetal distress | Emergency cesarean section |
Obstetrical fistulas | Repairs |
Congenital abnormalities: | |
Cleft lip/palate | Repair |
Club foot | Ponseti technique |
Hernias | High ligation |
Imperforate anus | Colostomy/definitive care |
Branchial cleft, thyroglossal cyst | Excision |
Random unpreventable diseases (many of these conditions are not included in the GBD data) | |
Appendicitis | Appendectomy |
Cholecystitis | Cholecystectomy |
Necrotizing fasciitis | Debridement and reconstruction |
Cellulitis and abscess | Incision and drainage |
Incarcerated hernia | Repair and possible bowel resection |
Foreign body: oral, nasal, ear | Removal possibly with exam under anesthesia |
Miscellaneous mass | Excisional biopsy |
Injury and violence | |
Burns | Debridement, skin grafting, contracture release, escharotomies |
Blunt trauma | Exploratory laparotomy, bowel, liver, spleen repair, flail chest fixation, fracture stabilization |
Penetrating trauma | Exploratory laparotomy, bowel, liver, spleen removal. Repair of vascular, tendon, nerve injury |
It is difficult to quantify surgically treatable conditions in developing countries because data collection and reliable reporting is limited. Most data come from hospital records and incomplete death registries. In 2006, Debas et al reported the first rough estimate of the global BoSC based on a survey of 18 surgeons working throughout all WHO regions. Surgically treatable conditions were estimated to be responsible for approximately 11% of all DALYs (Tables 14-4 and 14-5).27 The authors recognized that their data under estimated the true burden of disease because they do not take into account the true total number of operations performed or the number of “surgical opportunities” missed due to lack of access to surgical care.28 Weiser et al, estimated the annual volume of surgical interventions in developing countries to be 8 million, or just 3.5% of surgical care worldwide.29 Bickler et al defined the burden of surgical disease based on the ability to address surgical need. They defined surgery as met surgical need (actual surgical care provided), unmet surgical need (potential surgical care), and unmeetable surgical need (unpreventable death or disability despite surgical care) (Table 14-6).30 Current estimates of surgically treatable disease are based predominantly on met surgical need taking place in facilities such as hospitals, and they underestimate surgical conditions that go undiagnosed. With Bickler’s classification, these “missed surgical care opportunities” are included in the data (Figure 14-2).30
Trauma (38%) |
Cancer (19%) |
Random unpreventable disease such as appendicitis or hernias (19%) |
Congenital anomalies (9%) |
Obstetric complications (6%) |
Cataracts (5%) |
Perinatal conditions (4%) |
Group | % DALYs in World26 | % DALYs in Developing Countries26 | % DALYs Surgical27 |
|---|---|---|---|
I | 20.1 | 22.2 | 10 |
II | 59.7 |