FIGURE 16-1 MRI of transposition of the great arteries following atrial switch operation. Note the baffling of the superior vena cava (SVC) and inferior vena cava (IVC) towards the mitral valve and left ventricle (LV). There is no access to the tricuspid valve from the systemic venous side or the IVC.
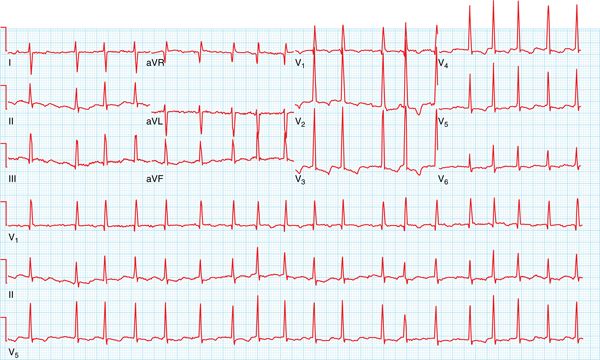
FIGURE 16-2 The patient’s clinical atrial flutter.
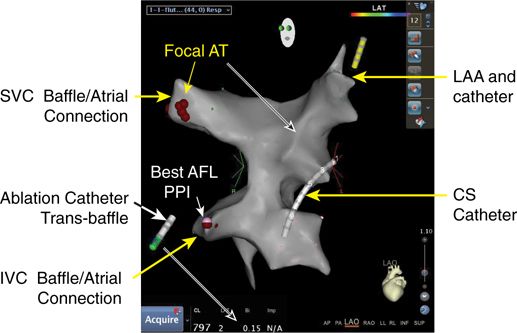
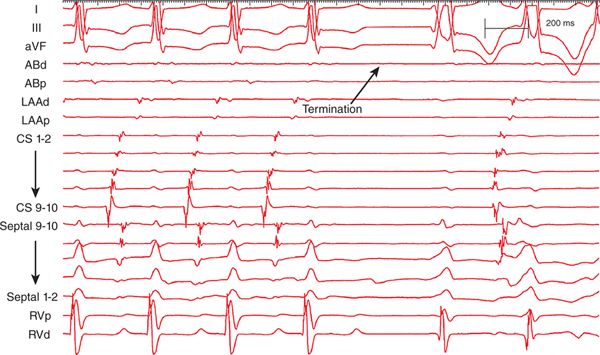
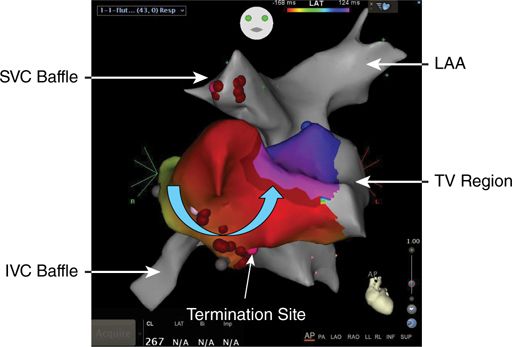
As is all too common in this population two separate arrhythmias were induced: an atrial tachycardia that had not been seen clinically (Figure 16-3) and atrial flutter (Figures 16-4 and 16-5). Mapping was initially performed on the systemic venous side, and the atrial tachycardia location was identified and ablated. In order to map the atrial flutter, a transbaffle puncture was performed to access the tricuspid valve and the pulmonary venous side (Figure 16-6). Entrainment mapping was used to identify the circuit (see Figure 16-5). The atrial flutter was successfully ablated (Figure 16-7) by placing lesions from the IVC to the baffle on the systemic venous side and then from the baffle to the tricuspid valve on the pulmonary venous side (Figure 16-8). She has had no recurrence of her atrial flutter.
FIGURE 16-3 Atrial tachycardia induced in the EP laboratory.
FIGURE 16-4 Atrioventricular block was induced during catheter manipulation, which makes the flutter waves easier to identify.
FIGURE 16-5 Entrainment mapping used to define flutter circuit.
FIGURE 16-6 Carto map of the systemic venous baffle. Note the site of successful atrial tachycardia ablation. The ablation catheter is on the pulmonary venous side of the baffle.
FIGURE 16-7 Atrial flutter terminated with radiofrequency ablation.
FIGURE 16-8 Both systemic and venous baffles are outlined. In order to completely ablate the flutter isthmus it was necessary to cross the baffle and ablate from the IVC to the tricuspid valve.
EPIDEMIOLOGY
• Over one million adult congenital heart disease (CHD) patients are living in the United States.1
• Forty-five percent have simple defects (atrial septal defect, ventricular septal defect, valve stenosis).
• Forty percent have moderately complex heart disease (tetralogy of Fallot).
• Fifteen percent have severely complex deflects (single ventricle anatomy, Fontan palliation, atrial switch procedure for transposition of the great arteries).
• Any patient who has had an atriotomy incision is at risk for supraventricular arrhythmias.
• Thirty-four percent of older patients with TOF develop symptomatic supraventricular arrhythmias.2
• Older style Fontans, that is, atriopulmonary, have up to a 50% incidence of atrial arrhythmias due to atrial dilation and suture lines.3
DIAGNOSIS AND MANAGEMENT
Atrioventricular Reentry and Twin AV Nodes
The embryological abnormalities that cause congenital heart defects may also have a direct impact on the conduction system. The AV node and the His bundle may only be displaced, or there may be accessory or duplicated AV connections with the possibility of reentrant arrhythmias.
Atrioventricular Reentry
• Common in some types of congenital heart disease.
• Ebstein anomaly (Figure 16-9) is associated with Wolf-Parkinson-White syndrome in 20% of cases. Nearly half of these patients will have multiple accessory pathways.
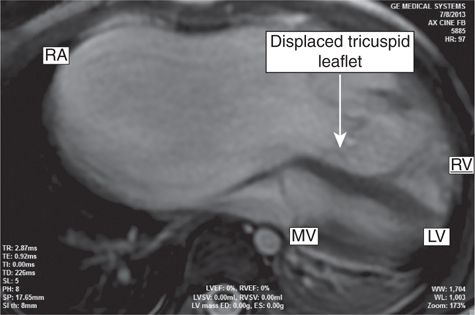
FIGURE 16-9 MRI of Ebstein anomaly of the tricuspid valve. Note the diminutive right ventricle, the displaced tricuspid valve, and the large right atrium.
• Patients with L-TGA, that is, corrected transposition, also have a high incidence of accessory pathways; many of these patients also have Ebstein anomaly of their left-sided tricuspid valve.
• Given the atrial dilation in these patients the risk of atrial fibrillation with rapid conduction is becoming increasingly problematic in adolescence and adulthood (Figure 16-10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree