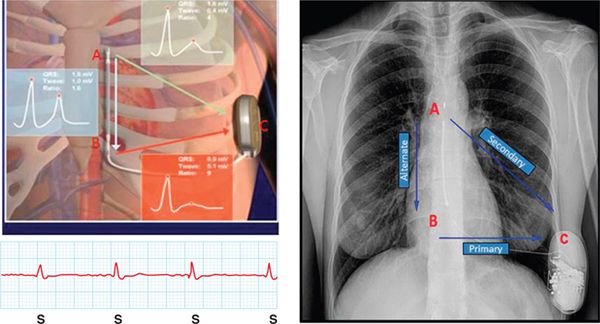
FIGURE 72-1 PA and lateral view of a chest X-ray of a 32-year-old patient with complex CHD and multiple corrective surgeries.
During follow-up she received appropriate therapy for ventricular tachycardia, but she also experienced inappropriate therapies that were managed by reprogramming the sensing vector of the S-ICD.
FUNCTION OF S-ICD
Subcutaneous ICDs are commercially available for management of sudden cardiac death. Patients that potentially can benefit from this therapy are those who have accepted indications for ICD implantation,1 who do not require antibradycardia pacing, or who have pace-terminable ventricular tachycardia.
Not every patient that has an ICD indication is suitable to be implanted with an S-ICD. Patients have to pass a prescreening 3-lead ECG in the supine and upright position. This prescreening ECG consists of three cutaneous electrodes placed in the proximity where the subcutaneous lead electrodes will be later implanted. This step has to be fulfilled in order to have the device implanted.
The advantage of the S-ICD is that there is no intravascular lead (Figure 72-2). Consequently, the implantation risks related to an intravascular procedure are eliminated, and the long-term risk of endocarditis due to lead infection and the risk associated with lead extraction are also minimal.
FIGURE 72-2 (A) Schematic representation of SICD pulse generator and subcutaneous electrode and sensing vectors. The electrogram obtained by the SICD is similar to an ECG tracing. (B) Chest x-ray of a patient with an SICD and a schematic representation of the vector.
The ability of the S-ICD to sense and defibrillate ventricular arrhythmias has been originally questioned, but the safety and efficacy of the system has recently been confirmed in a landmark study of 330 patients worldwide.2
The system consists of a subcutaneous electrode (SE) and a pulse generator (PG). The SE is a multistrand cable-core design, which is unlike a hollow core-design like TV leads. A multistrand design confers a stronger electrode. The polyurethane insulation was designed to withstand cardiopulmonary resuscitation forces, and the subcutaneous placement avoids intracardiac biomechanical stresses. This SE does not need to be as flexible as a TV lead. The PG is a 69-cc device capable of delivering 80 J, postshock, on-demand pacing at 50 beats per minute for up to 30 seconds and storing electrograms for approximately 48 episodes. The S-ICD can be programmed as a single zone in which the rate cut-off is the only determinant for providing therapy, or as a two-zone in which the second zone offers additional discriminators beyond just rate.
S-ICD SENSING AND INAPPROPRIATE SHOCKS
The sensing algorithm used by the S-ICD is a crucial component for appropriate detection and to minimize inappropriate therapies. It differs significantly from the TV ICD in two main ways.
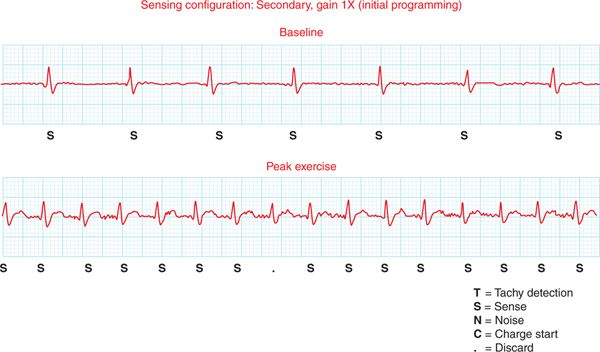
The first difference between the S-ICD and TV-ICD systems is that there is no endocardial sensing lead with an S-ICD. Sensing, therefore, is accomplished via three electrodes. Two of the electrodes are located along the subcutaneous lead (electrode A is at the tip of the lead and electrode B is 15 cm from the tip), and the third electrode is the PG (C electrode) (Figure 72-2). From these three electrodes, three different vectors are generated. The S-ICD automatically chooses the vector with the largest QRS to T-wave ratio, but that vector can be overridden by reprogramming. The QRS to T-wave ratio may vary under different conditions. It can change with body position (patient in the supine versus upright position) or during exercise (Figures 72-3 to 72-5). We have learned that testing sensing during an exercise treadmill test, particularly in young patients, is quite useful in preventing T-wave oversensing (Figure 72-6). In the patient presented in the case story, there were no further inappropriate therapies with reprogramming of the S-ICD sensing vector from secondary to primary vector configuration.
FIGURE 72-3 Baseline and exercise showing the QRS to T-wave ratio. This tracing discarded a single beat because that could not be classified (.).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree